Kobe University Hospital
Dr. Motoko Tachihara
Improved features of GuideSheath Kit 2

Detection of peripheral pulmonary lesions is increasing as the process of using computed tomography (CT) scans expands. The development of highperformance CT technologies allows us to identify the bronchial anatomy involved in the lesions and access them easily using bronchoscopes. In our hospital, endobronchial ultrasound with a guide sheath (EBUS-GS) is performed to increase accurate biopsy at peripheral pulmonary area. GuideSheath Kit 2 is used in our procedure. This product is improved from the previous model (GuideSheath Kit) in terms of efficiency and time-reduction in EBUS-GS biopsy include braided wire incorporated into the guide sheath to improve kink-resistance, allowing physicians to approach the target lesion with radial probe and devices smoothly. In addition, the device stoppers were changed to a clip-type, allowing physicians to maintain the device position for sampling. Herein, are the key points in using GuideSheath Kit 2 and a clinical example from my experiences with effective adoption of this product.
Approaches to peripheral pulmonary lesions –effective selection of bronchoscopes and guide sheath–
One of the critical points in bronchoscopy for peripheral lesions is to collect sufficient tissues for both definitive diagnosis of lung cancer and multi-gene panel tests. In our hospital, EBUS-GS are performed to increase the accurate diagnosis and to collect sufficient tissues. I also try to choose scopes depending on the type and position of legions. The combination of BF-P290 or BF-P260F and the guide sheath kit for 2.0mm channel scopes is mainly used for peripheral pulmonary lesions. If possible, a forceps biopsy is performed after guide sheath withdrawal. An ultra-thin bronchoscope, BF-MP290F, is the first option for peripheral pulmonary lesions in the fifth order or deeper bronchi. Alternatively, the guide sheath kit for 2.8mm channel scopes is selected for lesions in the third order, or more shallow bronchi, which are relatively close to the hilum or the inflammatory lesions, suspected as ground glass opacity or organizing pneumonia to obtain larger biopsy samples. I’m willing to use guiding devices and PeriView FLEX when I confirm the target bronchus reaches the boundary of the lesion with CT scan imaging and when an adjacent to lesion is suspected with an EBUS image. In any case, even after starting the examination, we do not hesitate to replace the bronchoscope with other models if it was judged more appropriate. Currently, regarding adaption to gene mutation screening, we aim to collect 10 samples from one lesion when using miniforceps. We need to perform biopsy safely and efficiently.
Combination of GuideSheath Kit 2 and PeriView FLEX in use of BF-P290
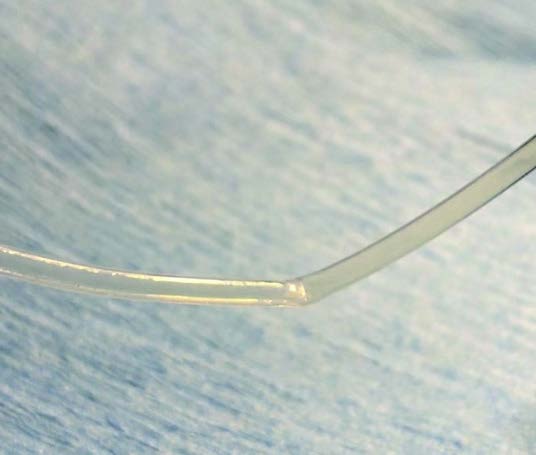
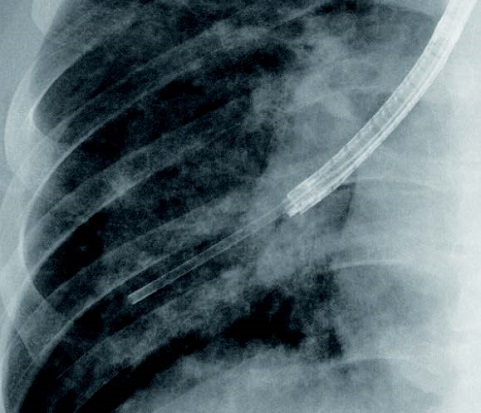
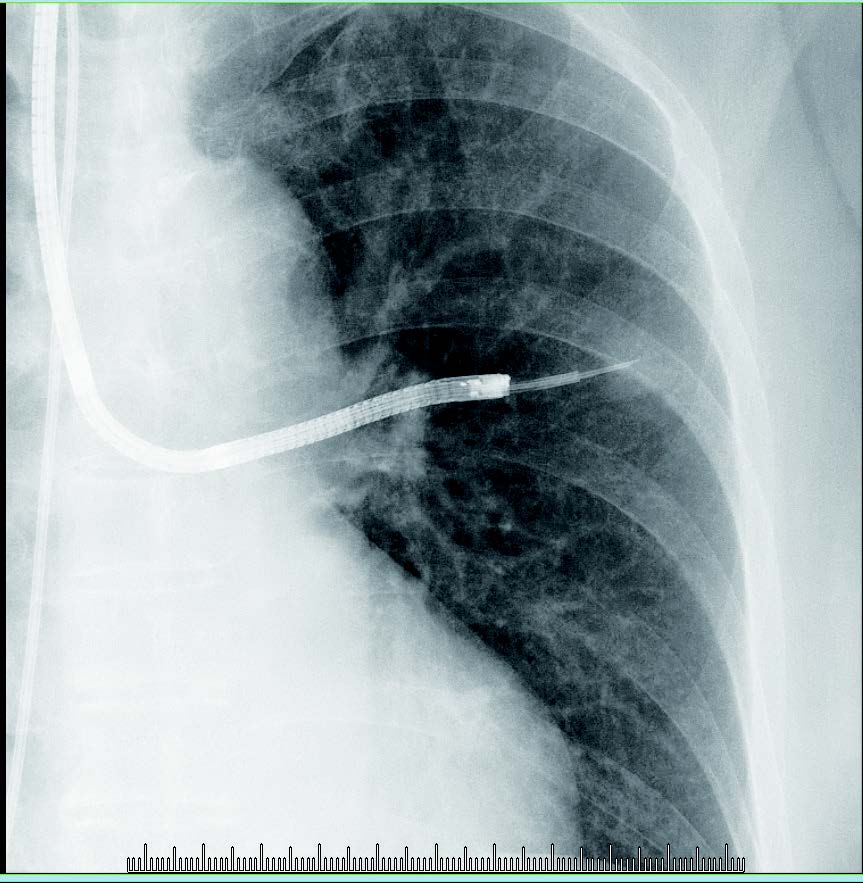
GuideSheath Kit 2 is designed to reduce the occasionally happening of wrinkling and kinking of the previous model (Figure 1). Especially when approaching lesions in the lung apex and S6, the sheath in the previous series was kinked in some cases. The kinked sheath prevented the insertion of biopsy forceps and cytology brushes into the distal part, even if the EBUS probe could be reached within the lesion. In addition, the visibility of the guide sheath itself under fluoroscopy is also improved (Figure 2). These improvements contribute to both time-reduction and safe procedure during the examination. Furthermore, puncture of peripheral lesions has become easy due to the flexible transbronchial aspiration needle, PeriView FLEX which is compatible with BF-MP290F or with Guide Sheath Kit 2 using BF-P290 and BF-P260F.
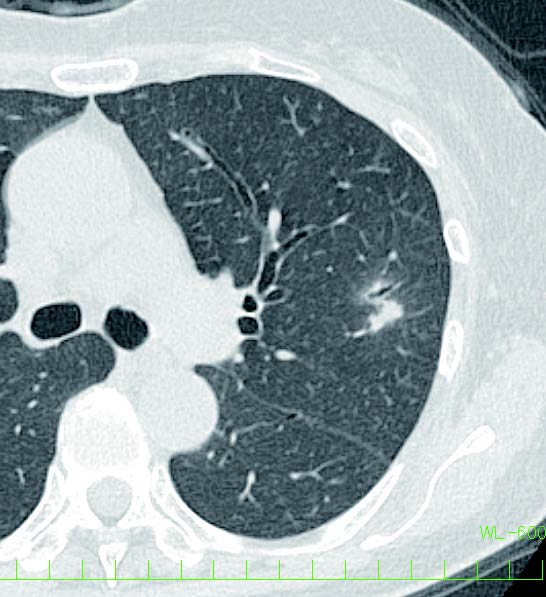
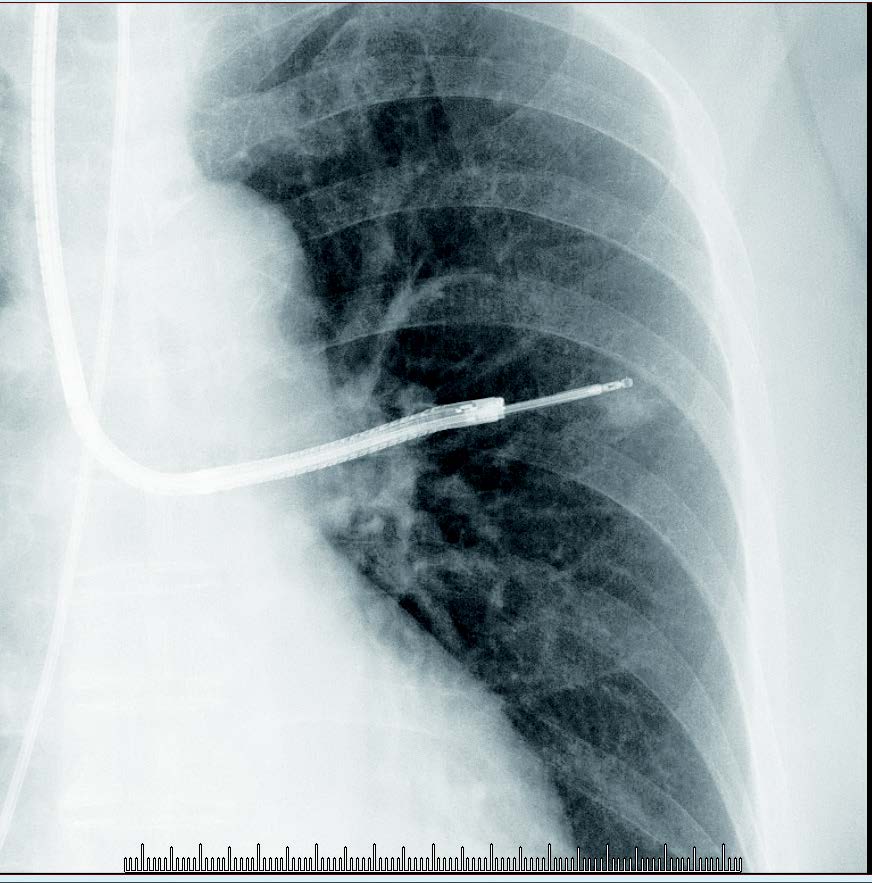
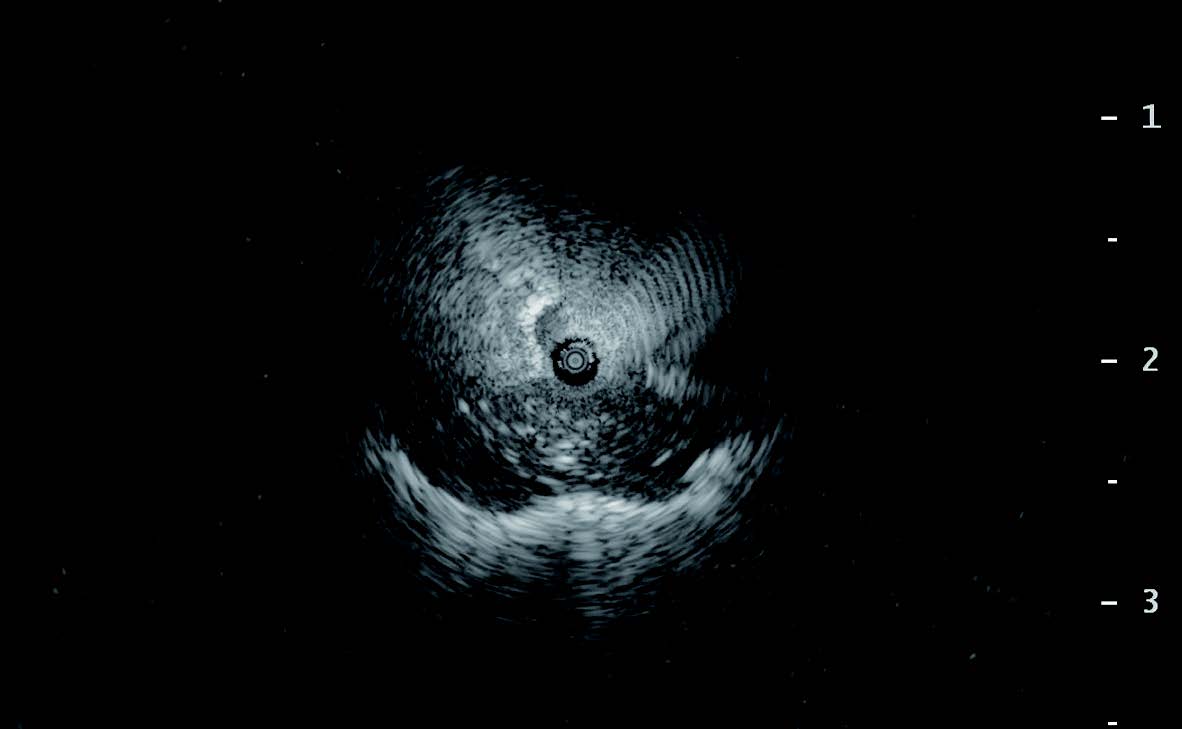
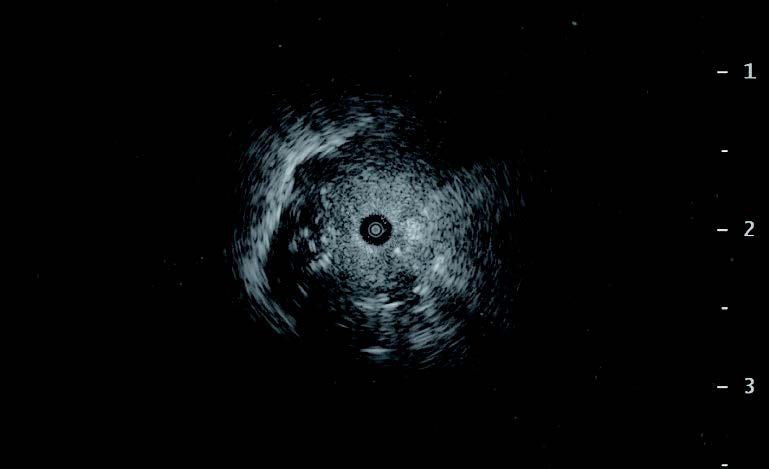
Herein, the case of a nodule in the left S3a is presented. The involved bronchus was not detected clearly, but the B3aii bronchi, which was located at an anterosuperior position to the lesion, was the closest one to the lesion (Figure 3). BF-P290 and the guide sheath kit for 2.0mm channel scopes were used for the approach to this lesion. As expected, it was confirmed with the EBUS image as an adjacent legion. I performed four transbronchial biopsies with EBUS-GS (EBUS-TBB), followed by two needle aspirations with PeriView FLEX via an inserted guide sheath (Figure 4). Fluoroscopy showed that the needle tip was positioned at the center of the lesion and followed EBUS showed that the probe position reached within the lesion. Thus, EBUS-TBB was additionally performed three times (Figure 5). The diagnosis result was an inflammatory nodule.
In transbronchial biopsy using any diameter of bronchoscope without a guide sheath, bleeding or edema of the respiratory tract epithelium can occur, preventing multiple biopsies in some cases. In addition, needle aspiration biopsy frequently causes bleeding after the puncture. The guide sheath can be used for hemostasis, and this is one of the benefits of EBUS-GS.
Figure 1. Problems of guide sheath in the previous model
Figure 2. Visibility of the guide sheath under fluoroscopy
Figure 3. CT images of a nodule in the left B3aii
Figure 4.
Figure 5.
Conclusions
In bronchoscopic examinations of peripheral pulmonary lesions, EBUS-TBB is a crucial procedure because of the availability of multiple biopsies from the appropriate area. Both multiple biopsies and puncture with PeriView FLEX are performed to collect sufficient samples for cancer gene mutation analysis. The guide sheath is required to be durable against multiple and various biopsies, and sufficiently kink resistant to provide a smooth approach to the lesion. The visibility of the guide sheath and bronchoscopic devises under fluoroscopy is also needed to perform a biopsy safely and efficiently. GuideSheath Kit 2 meets these requirements.
Kobe University Hospital

7-5-2 Kusunoki-cho, Chuo-ku, Kobe City, Hyogo Prefecture, JAPAN, 650-0017
Number of beds: 934
We provide advanced medical care as a regional core hospital and work as an institution for clinical education and research. We are committed to the treatment of many lung cancer cases as a regional cancer medical care base hospital.
*Disclaimer* Any content or information (“Content”) presented herein is illustrative in nature and does not guarantee or represent specific information, outcomes, or results. Olympus Medical Systems Corp. and its parents, subsidiaries, affiliates, directors, officers, employees, agents, and representatives (collectively “Olympus”) does not represent to or warrant the accuracy or applicability of the Content. Under no circumstances shall Olympus be liable for any costs, expenses, losses, claims, liabilities, or other damages (whether direct, indirect, special, incidental, consequential, or otherwise) that may arise from, or be incurred in connection with, the Content or any use thereof.Dr Motoko Tachihara is paid consultant to Olympus.Trademarks, product names, logos, or trade names used in this document are generally registered trademarks or trademarks of each company.
- Keyword
- Content Type