Department of Respiratory and Critical Care Medicine Director,

Department of Respiratory and Critical Care Medicine
Disclaimer:
- NBI™, RDI™ and TXI™ Technologies are not intended to replace histopathological sampling as a means of diagnosis
- The positions and statements made herein by Dr. Valipour and Dr. Sperk are based on their respective experiences, thoughts and opinions. As with any product, results may vary, and the techniques, instruments, and settings can vary from facility to facility. The content hereof should not be considered as a substitute for carefully reading all applicable labeling, including the Instructions for Use. Please thoroughly review the relevant user manual(s) for instructions, risks, warnings, and cautions. Techniques, instruments, and setting can vary from facility to facility. It is the clinician’s decision and responsibility in each clinical situation to decide which products, modes, medications, applications, and settings to use.
- The EVIS X1™ endoscopy system is not designed for cardiac applications. Other combinations of equipment may cause ventricular fibrillation or seriously affect the cardiac function of the patient. Improper use of endoscopes may result in patient injury, infection, bleeding, and/or perforation. Complete indications, contraindications, warnings, and cautions are available in the Instructions for Use (IFU)
- Dr. Valipour and Dr. Sperk, the authoring physician(s) of this presentation, are/ is a paid consultant(s) to the Olympus Corporation.
Scope: BF-1TH1100
Patient information: Female, 61 years old
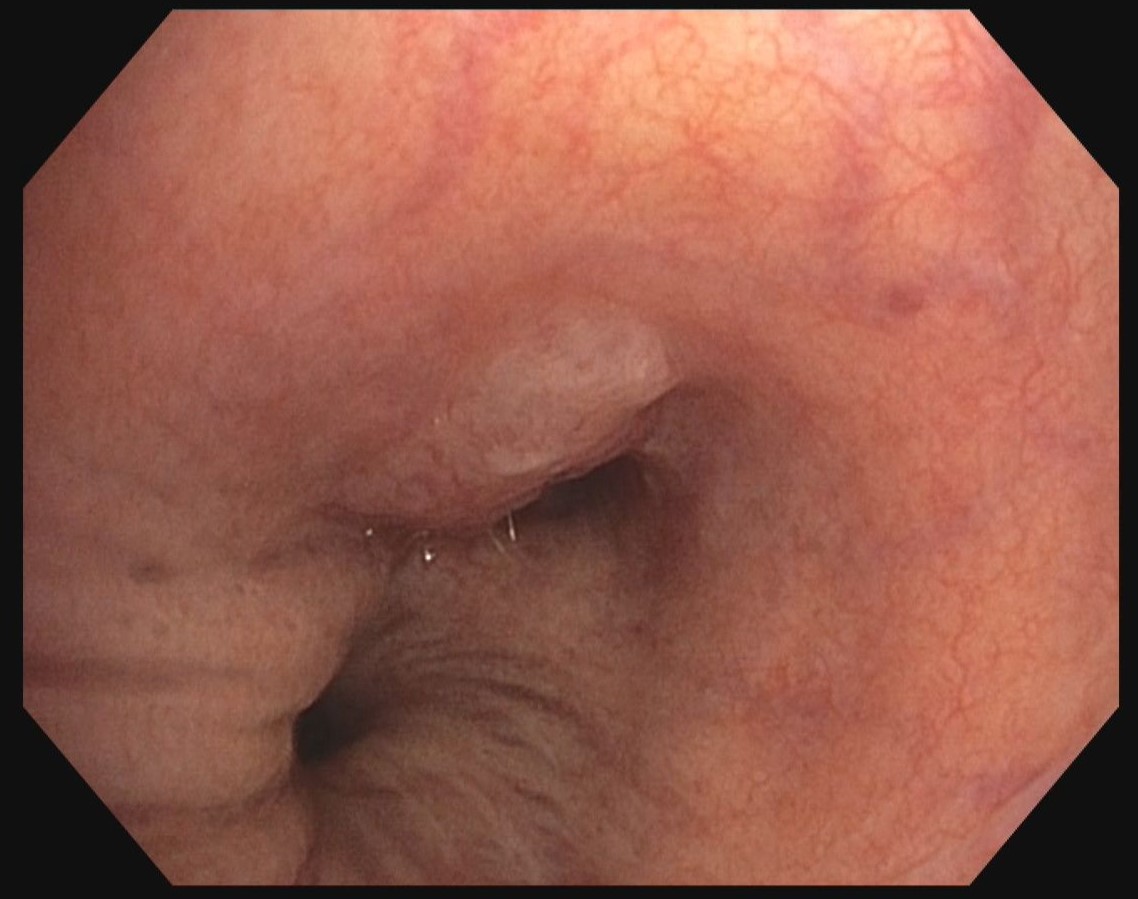
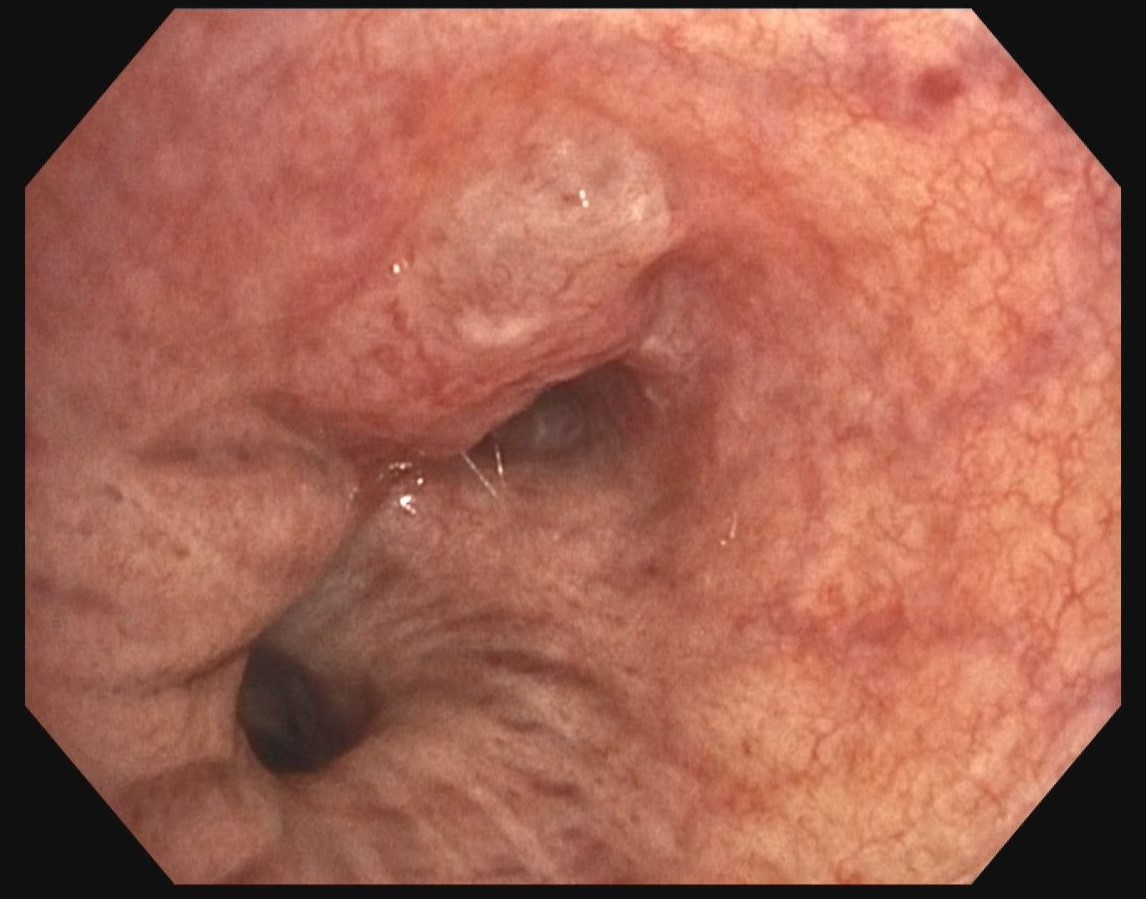
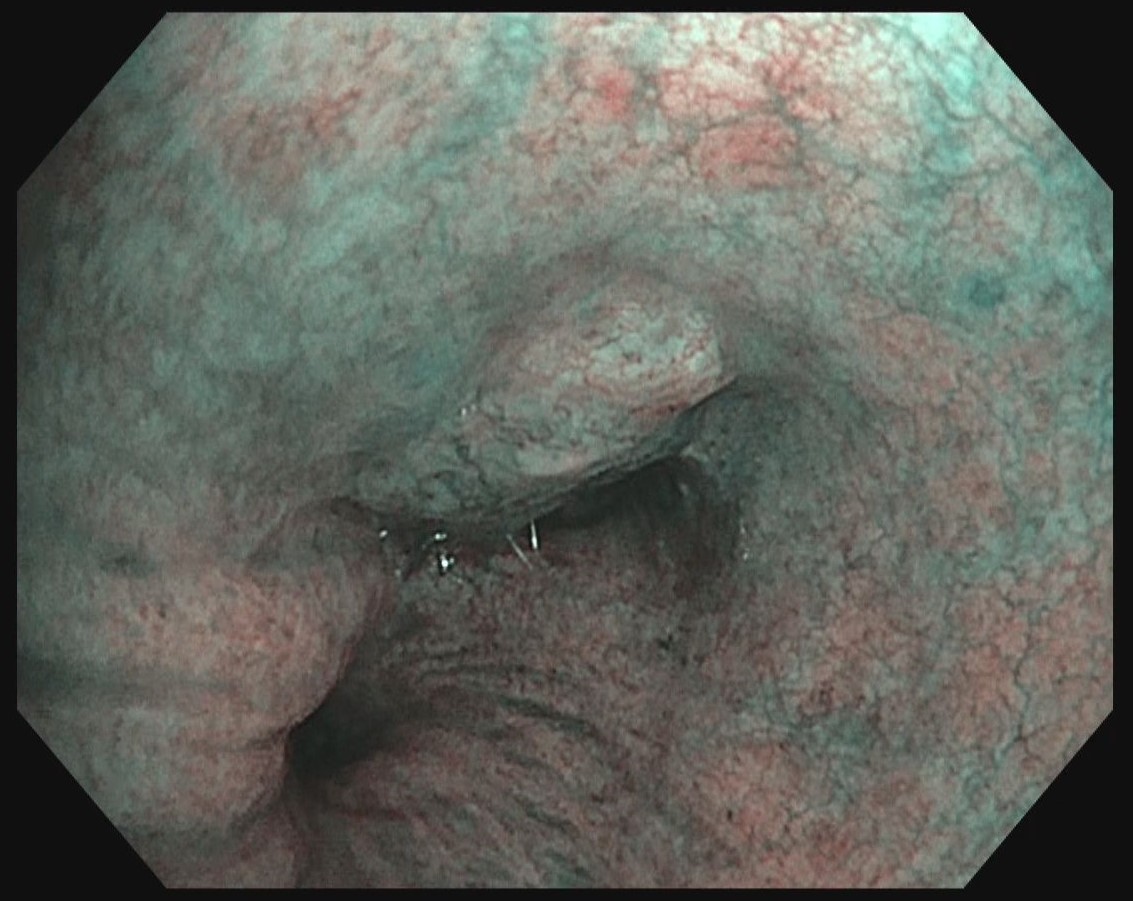
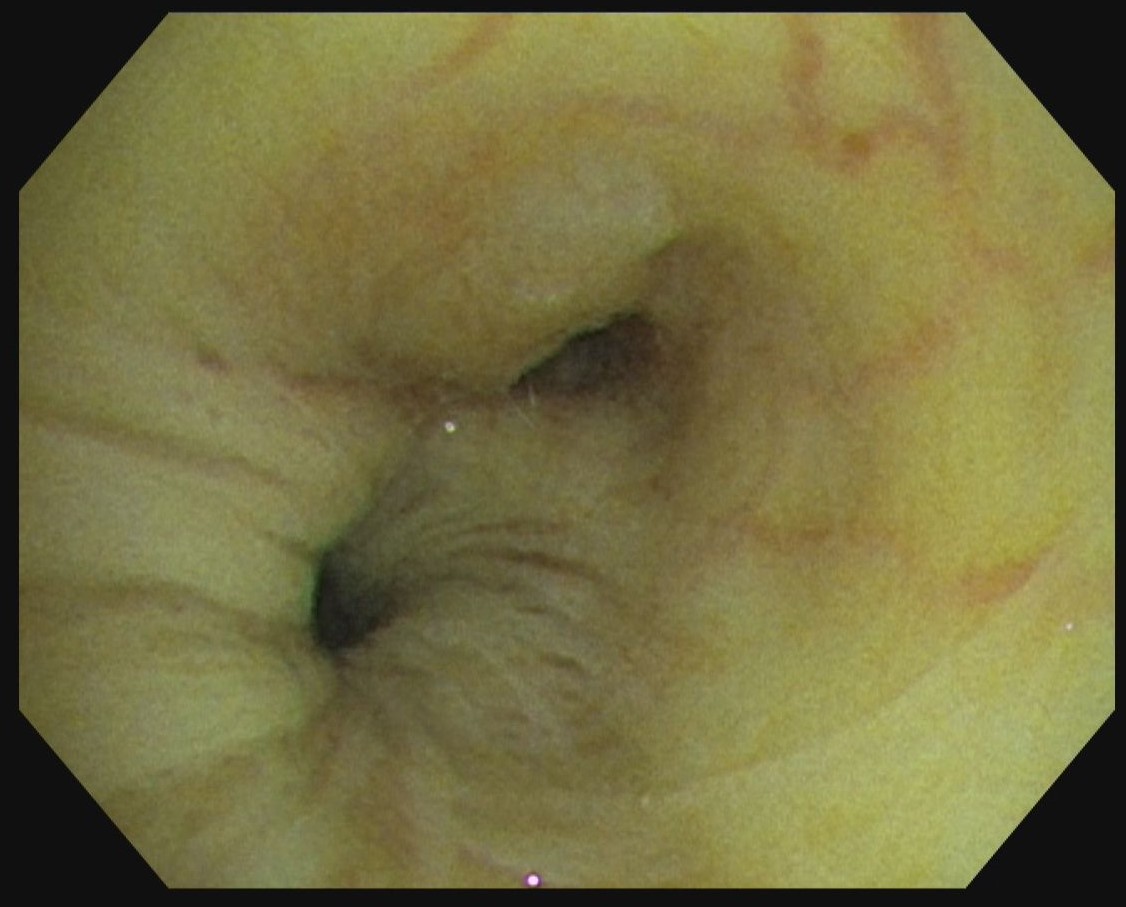
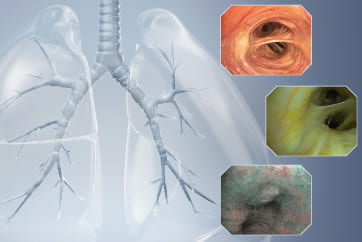
Medical history: Referral from our outpatient clinic to follow up an atelectasis of the left upper lobe caused by a central tumor mass.
Case video
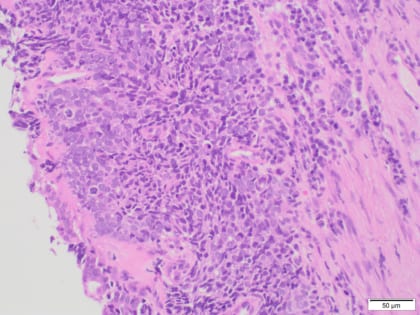
Pathological Findings
Lung biopsy tissue with formations of small cell lung cancer (NEC 3), bronchial mucosa with squamous cell metaplasia.
Overall Comment
Examination of the transition area between the lateral wall of the distal left main bronchus and the left upper lobe revealed a plain submucosal foreign tissue infiltration extending to a convex stenosis of the lumen of left upper lobe stem bronchus. This results in a subtotal occlusion of the left upper lobe. Especially TXI™ technology mode highlights visibility of mucosal foreign tissue mass in this case.
* Specifications, design and accessories are subject to change without any notice or obligation on the part of the manufacturer
- Keyword
- Content Type