Fumihiro Asano, MD, PhD
Department of Pulmonary Medicine,
Gifu Prefectural General Medical Center
Disclaimer:
- TXI™ and RDI™ Technologies are not intended to replace histopathological sampling as a means of diagnosis
- The positions and statements made herein by Dr. Asano, are based on Dr. Asano’s experiences, thoughts and opinions. As with any product, results may vary, and the techniques, instruments, and settings can vary from facility to facility. The content hereof should not be considered as a substitute for carefully reading all applicable labeling, including the Instructions for Use. Please thoroughly review the relevant user manual(s) for instructions, risks, warnings, and cautions. Techniques, instruments, and setting can vary from facility to facility. It is the clinician’s decision and responsibility in each clinical situation to decide which products, modes, medications, applications, and settings to use.
- The BF-1TH1200 used in this case is not available in the US market at this time nor is there an established time for its release. The safety and effectiveness of this product and or the use of these products has not yet been established in the United States market.
- The EVIS X1™ endoscopy system is not designed for cardiac applications. Other combinations of equipment may cause ventricular fibrillation or seriously affect the cardiac function of the patient. Improper use of endoscopes may result in patient injury, infection, bleeding, and/or perforation. Complete indications, contraindications, warnings, and cautions are available in the Instructions for Use (IFU)
- Dr Asano, the authoring physician(s) of this presentation, are/ is a paid consultant(s) to Olympus Corporation
Scope: BF-1TH1200
Case:Right lung tumor
Location:From the lower trachea to the right main bronchus
Patient information: Male, 70 years old
Medical history:Having experienced a persistent cough for about 1 month, the patient went to a local clinic. A chest X-ray revealed an abnormal shadow in the right middle lung field, and he was referred to our institution.
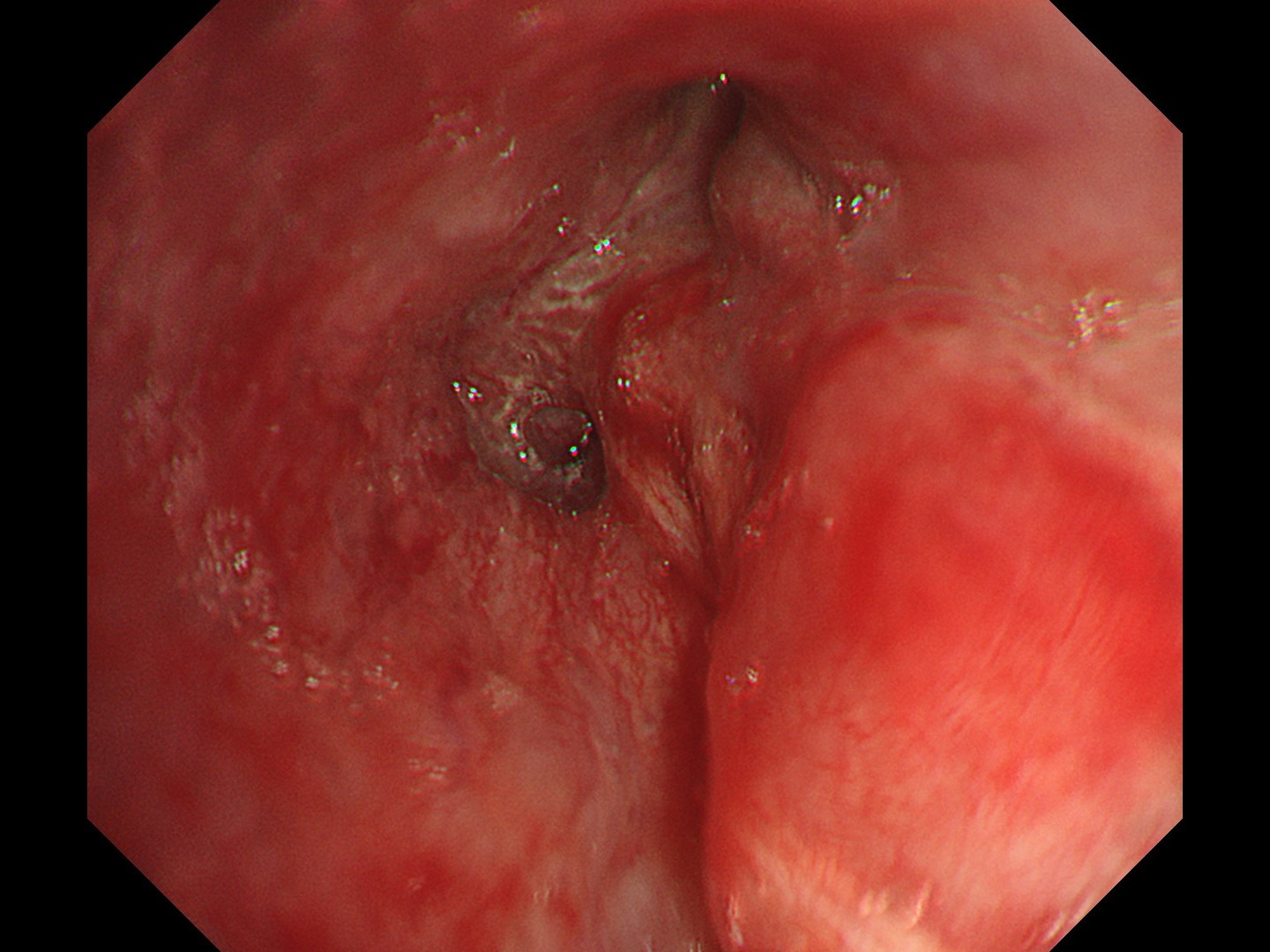
1. Tracheal bifurcation
(WLI)
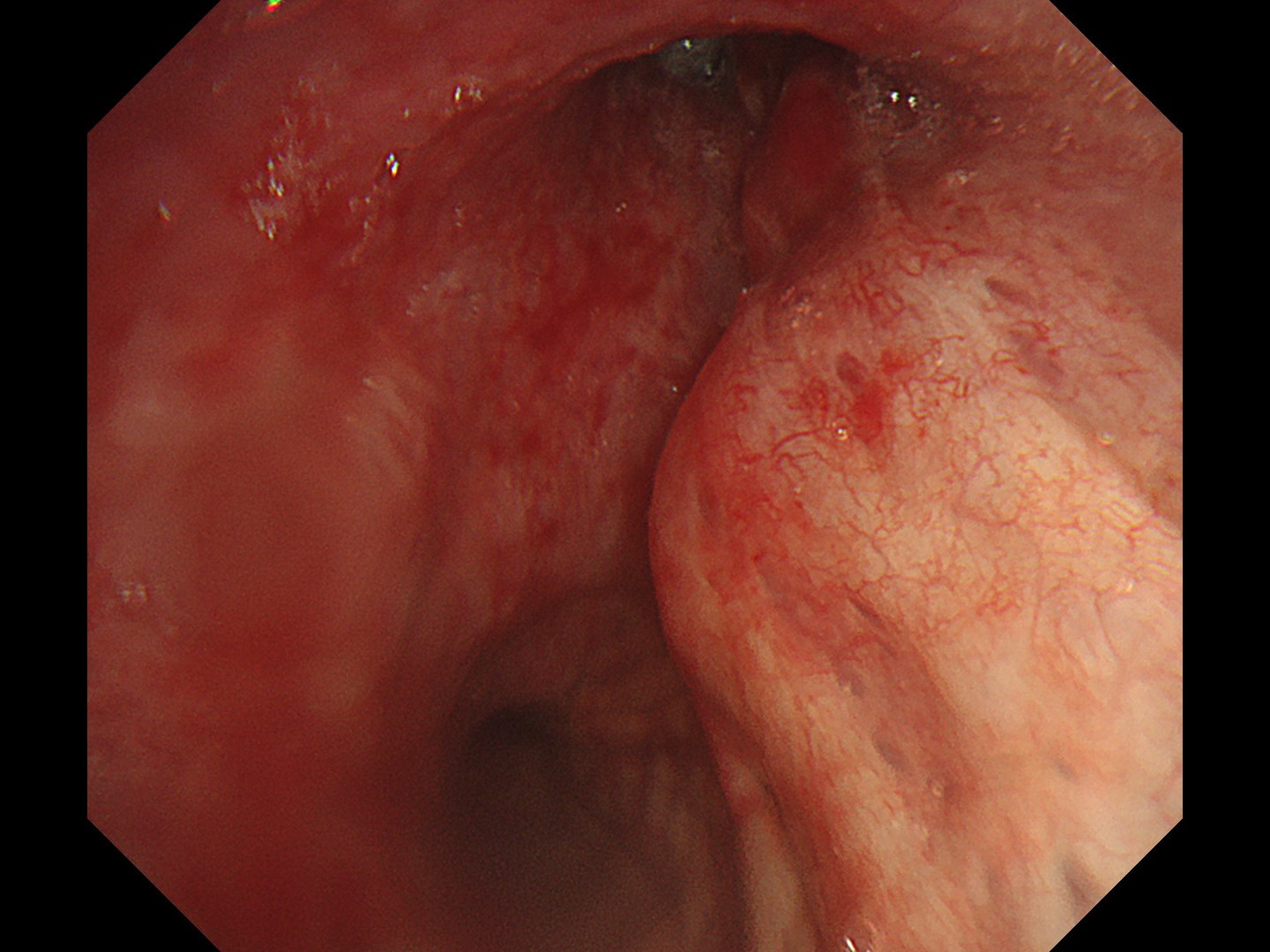
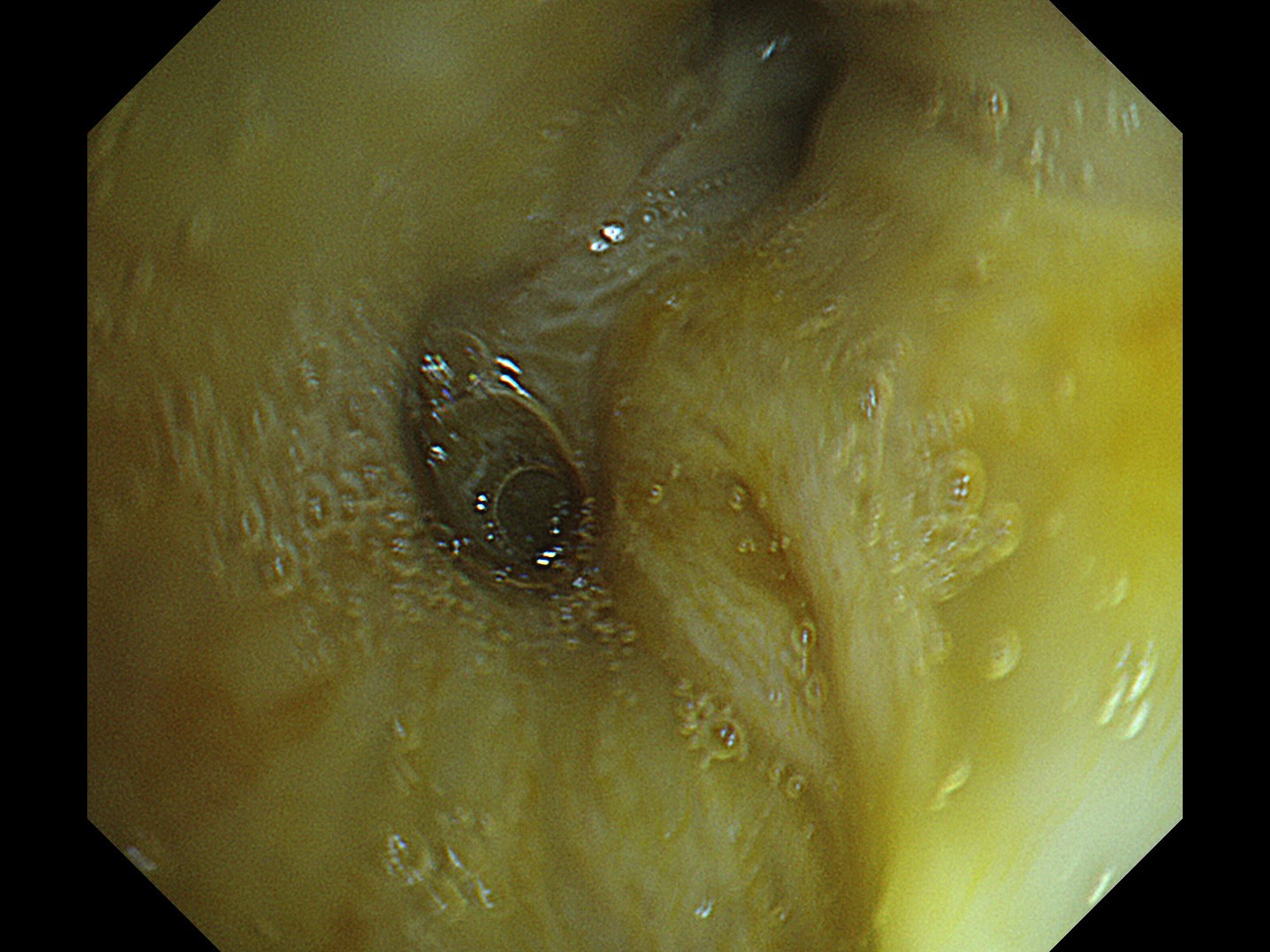
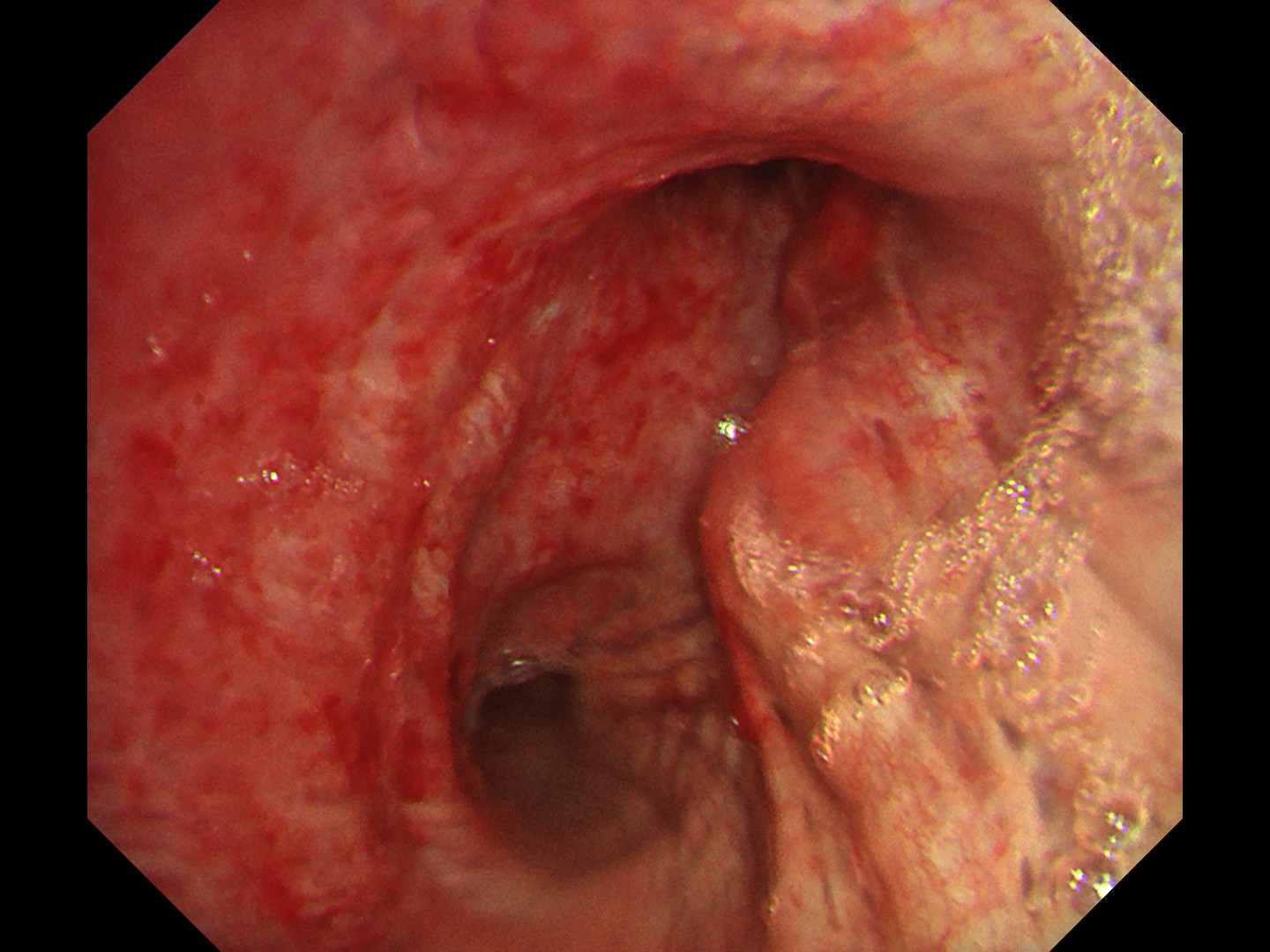
2. Tracheal bifurcation
(TXI™ Technology)
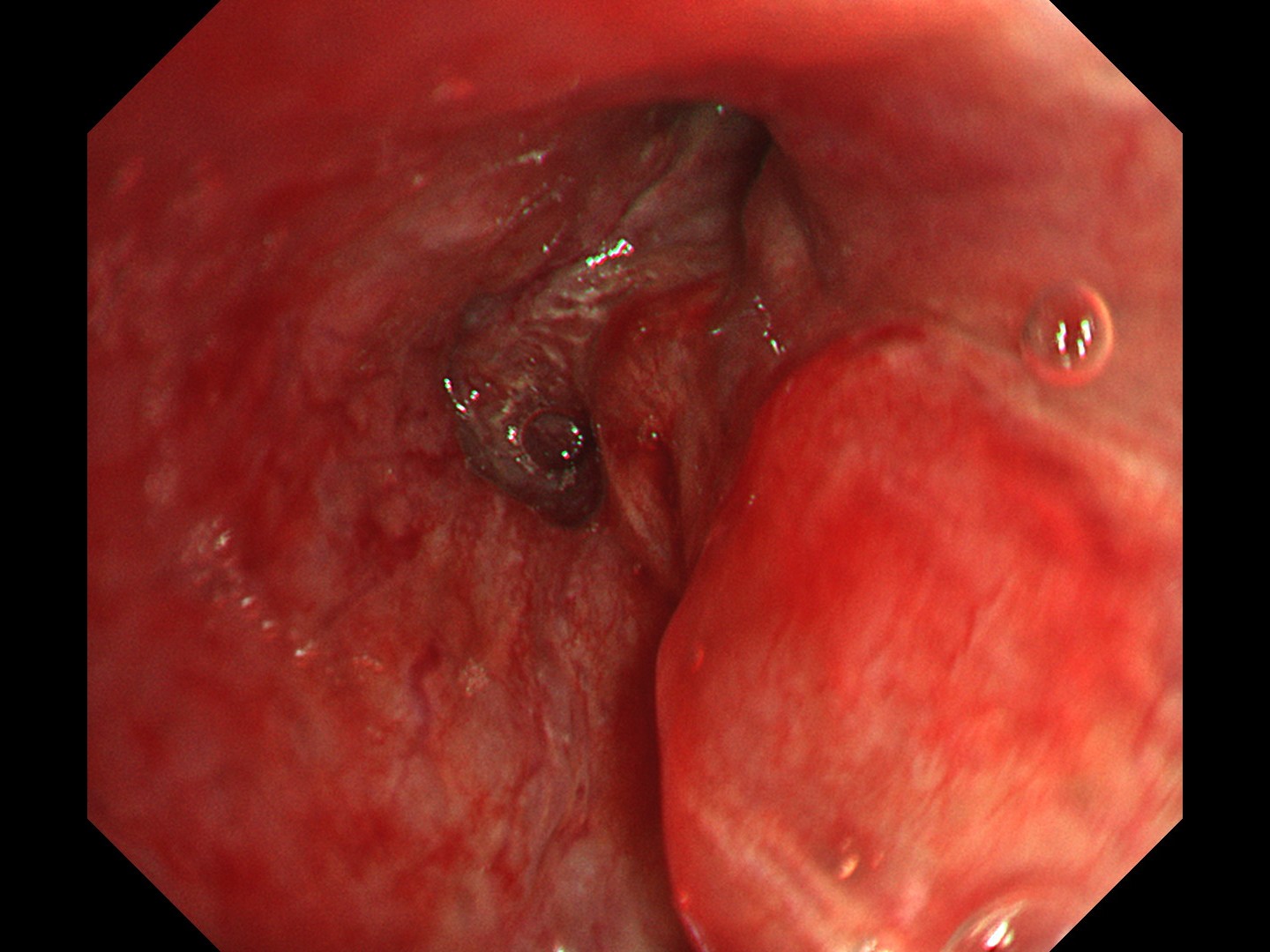
4. Right main bronchus
(TXI™ Technology)
Pathological Findings
Endoscopic biopsy and EBUS-TBNA of mediastinal lymph node revealed:
- Small cell carcinoma (poorly differentiated neuroendocrine carcinoma)
- Diffuse proliferation of atypical cells with high N/C ratio and small, round, naked nuclei; synaptophysin (+), chromogranin A (+), CD56 (+), TTF-1 (+), and LCA (-)
Overall Comment
This was a case of small cell carcinoma originating from the right upper lobe (c-T4N3M1, stage IV), with bronchoscopy findings showing widespread progression of the small cell carcinoma from the subepithelial layer to inside and outside the bronchial wall. TXI™ technology mode enhances the visualization of SCLC that has spread widely beyond the bronchial wall, compared to white light. Additionally, it allows for clear observation of distal areas without causing halation in proximal areas, enabling easier determination of the extent of invasion.
- Content Type