Faculty
Ronald Clements, MD
Chief of Bariatric Surgery
Professor of Surgery
Vanderbilt University Medical Center
Nashville, Tennessee
Brett Cohen, MD, FACS
Medical Director
Memorial Health System for Advanced Laparoscopic and Bariatric Surgical Program
Memorial Regional Hospital
Hollywood, Florida
Rami Lutfi, MD, FACS
Chairman of Surgery
Mercy Hospital and Medical Center
Clinical Assistant Professor of Sugery
University of Illinois at Chicago
Chicago, Illinois
Marcos Michelotti, MD
Assistant Professor of Surgery
Loma Linda University School of Medicine
Loma Linda, California
Marc Singer, MD
Colon/Rectal Surgeon
Clinical Assistant Professor
NorthShore University HealthSystem
Evanston, Illinois
Todd Wilson, MD
Assistant Professor of Surgery
University of Texas Health Science Center
Houston, Texas
The inception of laparoscopy marked a significant turning point in patient care. The transition from open procedures to a minimally invasive approach to surgery resulted in numerous benefits including minimal pain, less need for narcotic analgesics, fewer complications (eg, hernia and infection), less blood loss, shorter (and consequently less expensive) hospital stays, and a faster recovery and return to normal daily activities.1-3 The indications for laparoscopic surgery quickly expanded to increasingly complex procedures—gastrointestinal, gynecologic, and urologic—and more complicated patient populations.1,4,5
Although the integration of laparoscopy improved clinical outcomes and reduced costs, it offered limited visualization and articulation—key elements of open surgery. Mobility and dexterity associated with direct visualization in a 3-dimensional (3D) field were compromised.1 Surgeons found it necessary to adjust to the loss of depth perception inherent to operating in a 2-dimensional (2D) field and deferring to a video screen when operating on patients.1 The shift to laparoscopy required a new set of skills and more specialized training; consequently, this entailed a prolonged learning curve that increased the risk for complications.6-8
With the development of 3D laparoscopic systems, the benefit of depth perception was restored and the advances made through laparoscopy were recognized. However, widespread use of 3D was hindered by a lack of image brightness, inadequate image quality, and excessive fatigue and discomfort caused by the heavy activeshutter 3D glasses.9,10 Although robotic surgery restored high-quality 3D imaging and surgical dexterity, its adoption as a standard approach remained problematic particularly because of its size and associated expense.1,6,8 More importantly, clinical support on the practicality of robotic surgery remained preliminary.9,11
With the recent FDA clearance of the ENDOEYE FLEX 3D, the world’s first and only high-definition (HD), 3D articulating videoscope—surgeons are now able to operate with restored depth perception. The system’s articulating design allows surgeons to obtain critical views at ideal angles without sacrificing a level visual horizon (Figures 1 and 2). Additionally, its modular design enables surgeons to easily switch between 2D and 3D visualization. Preliminary research and clinical experience suggest that by enhancing visualization and precision, the ENDOEYE FLEX 3D system facilitates faster and more precise execution of laparoscopic procedures, while shortening the learning curve for surgical tasks (Figure 3).12,13 Furthermore, integrating the EVIS EXERA III Universal Imaging System, with the ENDOEYE FLEX 3D videoscope into the surgical suite can improve efficiency through the standardization of surgical equipment, training, and service and biomed support.
This monograph discusses the benefits of integrating the ENDOEYE FLEX 3D system to improve efficiency and precision in laparoscopic procedures, level the learning curve, and potentially consolidate surgical technology through a universal platform.

Figure 1.
The ENDOEYE FLEX 3D Articulating Videoscope offers 100-degree angulation that can provide critical views and a level visual horizon.
Figure 2.
The ENDOEYE FLEX 3D Articulating Videoscope provides depth perception using a 3D monitor (simulated 3D image shown).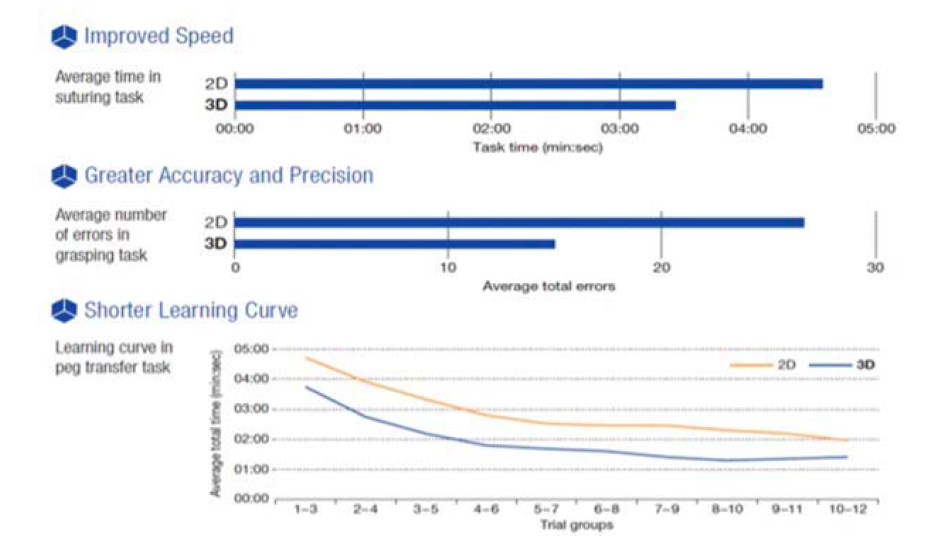
Figure 3.
The ENDOEYE FLEX 3D showed improved speed, accuracy, and precision for surgical tasks while helping to shorten the learning curve, based on testing using a simulated surgical model.Minimally Invasive Surgery With Limited Depth Perception
With the advent of laparoscopy, surgeons are able to perform a variety of procedures through small incisions using trocars, rather than through footlong incisions. Unlike with open surgery, laparoscopic surgeons use auxiliary visual cues to determine depth and where to position surgical instrumentation while referring to a 2D video monitor.7 “Laparoscopy has given surgeons the ability to perform through tiny incisions almost every surgery that once required a large incision,” said Brett Cohen, MD, medical director of the Memorial Healthcare System for Advance Laparoscopic and Bariatric Surgical Program. Laparoscopy has resulted in better outcomes, shorter hospital stays, and faster recovery times, while containing costs.1-3 In fact, laparoscopy became the gold standard for cholecystectomy even before evidence from prospective randomized controlled trials showed its superiority over open cholecystectomy.14,15
Although the approach is less invasive, the reduced depth perception inherent with laparoscopy poses a significant challenge for surgeons.16 Rather than visualizing the peritoneal cavity directly, laparoscopy incorporates the use of a 2D monitor. “In laparoscopy, you have to be a little farther from the area you’re operating on. The caveat is, the farther away you go, when you put the laparoscope in you’re looking at quite a distance and you get a very flat view,” explained Dr. Cohen. “Classic TV screens are 2D. We’re working on a 3D object within the body and a 3D procedure, but we lose our depth of field and have to get used to working in 2 dimensions,” Dr. Cohen said. “It has a lot to do with the feedback that comes through the instruments, and the eye adjusting to working with that depth of field.”
Challenges inherent to evaluating 3D structures in 2D increase the risk for complications related to a surgeon’s skill and experience. This includes risk for complications associated with pneumoperitoneum (eg, decreased cardiac output) and with the procedure itself.14 As the standard approach to cholecystectomy, laparoscopy was associated with an increase in biliary injury, including misidentification of the bile duct and delayed stricture; whereas laparoscopic antireflux surgery led to lower wound, cardiac, and pulmonary complications, the most common intraoperative complications included perforations of neighboring anatomy, and pneumothorax; in laparoscopic inguinal hernia repair, intraoperative complications included injuries to the bladder, the epigastric vessels, and spermatic cord; and ureteric injury occurred in laparoscopic colectomy.14,17
For surgeons experienced in open surgery, laparoscopy involves a paradigm shift that requires an additional set of operative skills, with a prolonged learning curve, to handle surgical instrumentation while referring to a video monitor to judge positioning and depth.7 Recently, a study investigating the effect of 3D visualization on surgical skill and task performance in 3 different types of surgical approaches emphasized the importance of depth perception.18 The researchers assigned 34 surgeons with varying laparoscopic experience—about half were novices—to perform tasks testing their skills assessing spatial relationships, grasping and positioning, precision, dexterity, and hand–eye/hand– hand coordination, in both 3D and 2D.18 The results showed that the loss of 3D imaging and depth perception had a significant effect on the surgeons’ perception of the difficulty of a task, as well as on the time it took to perform it. Simpler tasks required 25% to 30% more time to execute, whereas complex tasks took as much as 75% longer to perform.18 The researchers concluded that the more complicated a task was, the greater the effect of 3D visualization on accelerating that task.18
Studies evaluating the learning curve for laparoscopy indicate that the rate of intraoperative complications appears to diminish with surgeon experience. In a 1995 study of the laparoscopic learning curve, 90% of bile duct injuries in laparoscopic cholecystectomy occurred within a surgeon’s first 30 cases,15 whereas a later study showed that the learning curve for laparoscopic inguinal hernia repair was about 50 cases.19
Training in laparoscopic techniques plays a crucial role in surgeons’ ability to master 2D visualization. Recent innovations recognize the benefit of minimally invasive techniques, as well as the efficiency and safety associated with 3D imaging. “In my opinion, being able to see structures and planes between organs easily and suture more accurately, adds value to the surgeon, and the value will translate to safe and more efficient moves,” said Rami Lutfi, MD, chairman of surgery at Chicago Mercy Hospital and Medical Center.
Integrating 3D Surgical Technology
3D visualization offers a number of benefits: enhanced depth perception yielding more precise spatial views of anatomy; faster and more accurate completion of tasks such as grasping, suturing, and dissecting; and an accelerated learning curve for the acquisition of surgical skills.7
“For me, better depth perception means better structure recognition, better plane recognition, and facilitates certain maneuvers, such as knot tying,” said Marc Singer, MD, a colon and rectal surgeon and clinical assistant professor at NorthShore University HealthSystem. 3D also may help in operations where access is challenging. “Any time we’re working at a great distance from the camera, such as deep in the pelvis, we experience some visual paradoxes that make conventional laparoscopy difficult. In colon and rectal surgery, there are parts of the operation, such as identifying the ureter, where I feel 3D really makes a difference,” Dr. Singer said.
Other 3D surgical technology generally comprises a rigid telescope and a camera head with right- and left-eye sensors; images are fed to the respective right and left sensors. When all components are in alignment, the result is restored depth perception, but this is contingent on stability. If the surgeon, seeking a different angle of view, rotates only the telescope, the images fall out of alignment with the sensors and the 3D screen image is lost. The surgeon can compensate for this by rotating both the camera and telescope to view a point from a different angle, but this causes the images on the screen to rotate as well. To maintain orientation, the surgeon has to rotate his or her head, which can throw off equilibrium and create dizziness.20 Additionally, earlier 3D video systems required surgeons to operate wearing bulky glasses—a potential inconvenience.21
With the introduction of robotic surgery, surgeons were equipped with the technology to tackle these shortcomings. The da Vinci Surgical System (Intuitive Surgical) offers a number of advantages over conventional laparoscopy, including improved ergonomics and reduced tremor interference.8 Additionally, the da Vinci uses the EndoWrist technology, which offers 7 degrees of freedom and 90 degrees of articulation, while restoring dexterity and interpreting the surgeons’ hand motions with great precision and refinement.6,8,16,22 The most useful feature of robotic surgery, however, is the restoration of stereoscopic 3D vision through the use of a double- channeled camera integrated in the surgical console.6 This allows surgeons to regain control over visualization and operate with more precision.
One study showed that surgeons using the 3D mode display on the da Vinci Surgical System completed suturing 65% faster than those who used the 2D mode.16 Additionally, the 3D mode resulted in enhanced speed and accuracy, particularly in knot-tying ability.16 As early as 2001, researchers showed that telemanipulator performance was enhanced by the availability of 3D-National Television Standard Committee despite the surgeons’ familiarity with 2D systems and the fact that the 2D systems operated at an equal or better resolution than the 3D system.23
Although the da Vinci system integrates 3D visualization, it may not be an ideal approach for some clinicians given the associated costs (initial cost: $1.7 million) and the need for additional staffing and training.6,8 Robotic surgery reinforces the importance of 3D visualization, and has provided a stepping-stone toward further advances in restoring surgical control to improve accuracy and precision.
ENDOEYE FLEX 3D: Enhanced Visualization and Articulation
With the availability of the ENDOEYE FLEX 3D laparoscope, surgeons have an effective tool that applies 3D visualization and 100 degrees of articulation to maximize spatial orientation. Using lightweight 3D glasses-a clip-on option is available for surgeons who already wear glasses—surgeons are equipped with a system that restores natural 3D that is transmitted through an HD 3D monitor. “The [ENDOEYE] system we’re using here is much more subtle and refined and you have a little more ability to manipulate it with the flexible technology,” Dr. Wilson said.
High-Definition Imaging
The ENDOEYE FLEX 3D system uses a dual-lens system with distally located image sensors in which the right and left images are captured by separate lenses and processed by 2 CV-190 video processors that are integrated by the Olympus 3DV-190 to produce brighter, more light-sensitive images (Figure 4). The dual-lens, distal tip design increases the angle between left and right lenses, enhancing the perception of depth. The ENDOEYE FLEX 3D restores 3D visualization and provides greater depth perception and spatial view of anatomy compared with the rigid laparoscope. The quality of depth perception is contingent on the angle between the object and each eye. Some systems use a single-lens pupil system, in which a single image is split by a prism and delivered to 2 sensors, which decreases the angle. The ENDOEYE FLEX 3D videoscope’s depth of field ranges from 18 to 100 mm, eliminating the need for manual focus adjustment. “The dimensionality is very impressive,” noted Ronald Clements, MD, chief of bariatric surgery and a professor of surgery at Vanderbilt University Medical Center.
Dr. Cohen has been using the ENDOEYE FLEX 3D since Pembroke Memorial Hospital became the first in the United States to adopt Olympus’s fully integrated 3D system in late 2013. “This 3D equipment has given us back [the 3D] dimension,” he said. “With this dynamic 3D visualization, the view is exceptional. It magnifies and clarifies the image incredibly. The first time I used it, I told the [technician] who operates our system, ‘this is the biggest advent in laparoscopy since the laparoscope.’”
Using 3D visualization, surgeons have more control of the instruments when
handling layers of tissue, and can perform challenging tasks, such as dissection, grasping, and suturing, faster and with enhanced accuracy and precision.12 Recent data using a simulated surgical model indicated that surgeons were able to grasp 25% faster and with 44% fewer errors using 3D imaging. Results also showed that surgeons could dissect tissue 10% faster and suture 35% faster.12 “The goal in the OR [operating room] is not to get through a system as quickly as possible, but as safely as possible. That said, being able to see the operation more clearly allows you to do things faster,” Dr. Cohen said. “For example, if you’re doing a gallbladder operation, you need to differentiate the main duct of the gallbladder from the main duct of the liver. If you can see structures with crystal clarity, magnified 10 to 15 times, it’s a lot easier and safer.”
‘I think articulation is very important for procedures where you need to look into deeper and curved areas, like with hiatal hernia repair, when you need to look around the spleen and around the liver, and when you need to dissect anatomical structures close to each other.’
ーMarcos Michelotti, MD
Unlimited Articulation
Despite the availability of other 3D laparoscopes before the ENDOEYE FLEX 3D, lack of articulation may have been one of the drawbacks to them becoming standard in laparoscopy.
Unlike the conventional laparoscope, the ENDOEYE FLEX 3D allows surgeons to view the entire peritoneal cavity by angulating in 4 directions—up, down, right, and left—up to 100 degrees and providing critical views of anatomy with a level visual horizon. “Olympus put the camera at the very tip of the rod, with a junction about 2 or 3 cm from the tip that allows it to articulate 100 degrees in every direction. You can look down, up, left, right, go to a structure and look around the corner, or look right down on it,” Dr. Cohen said.
Dr. Cohen likened this phenomenon to standing on one edge of a plane and trying to see clearly what is happening at the edge farthest away. “But [with ENDOEYE], you start at the far edge of the plane and have your view go right over the top of the object and look down on it. This truly mimics open surgery,” he said. “With this system, you can do everything with one hand—one knob allows you to look left, right, up, down. You can lock it in place. You don’t have to use 2 hands to manipulate it, so the design is really quite ingenious.”
Marcos Michelotti, MD, assistant professor of surgery at Loma Linda University School of Medicine, recognizes that the articulating design enables surgeons to have more control in maneuvering within the peritoneal cavity. “[The design’s] flexibility makes procedures significantly less cumbersome, and makes the camera job a lot easier to accomplish,” he explained.
Because the system is capable of recreating the same critical view as a standard 2D 30-degree telescope, surgeons can manage image integrity and orientation when shifting to view an object from a different angle. “The articulating scope can be used straight or angled, and it gives you perspectives you just cannot get with a rigid laparoscope. It allows you to look down on tissue as we do with open surgery, and to look under structures and around corners,” said Dr. Singer.
For very straightforward cases, such as appendectomy, a straight laparoscope may be sufficient, but for more dynamic and complex procedures, such as colectomy, Dr. Singer believes the articulating laparoscope facilitates tremendous perspective. “I think an articulating laparoscope should become the standard,” he said. “Rigid laparoscopy limits surgeons and the perspective, while the articulating scope really offers more flexibility because it can be used as a straight scope or an angled scope.”
“Articulation adds value anytime you need to see over, around, or behind something,” Dr. Clements said. “It helps me in hiatal hernia repairs to get up into the mediastinum and be out of the way of my instruments by having the camera above the plane of where the instruments are looking down on it.” Dr. Michelotti agreed: “I think articulation is very important for procedures where you need to look into deeper and curved areas, like with hiatal hernia repair, when you need to look around the spleen and around the liver, and when you need to dissect anatomical structures close to each other.”
Dr. Cohen finds the articulating laparoscope especially beneficial in certain types of procedures, and in certain types of patients. “In a Nissen fundoplication, part of the operation includes freeing up the esophagus as it cuts through the diaphragm muscle into the belly, so we dissect high up in the mediastinum above the diaphragm. Being able to have the scope closer to the belly button and still use the articulating tip to look all around the esophagus and in the mediastinum with a clear, unobstructed view—we’ve never been able to do that before,” he said.
The articulating laparoscope also is helpful in procedures on obese patients. “Bariatric patients have a lot of fatty tissue. Being able to bring the scope all the way up to the angle of His of the stomach and then flex the scope down to look at where the stomach attaches to the diaphragm—that’s something else we haven’t been able to do. Being able to look around the corner is new, and very advantageous,” Dr. Cohen said.
Alternating Dimensions and Advanced Visualization
In cases where 2D would be preferable (eg, when accessing the abdominal cavity under direct vision through a trocar), the ENDOEYE FLEX 3D system’s visualization mode can be easily switched from 3D. Dr. Lutfi has found this feature useful when accessing the layers of the abdominal wall. “I can put a straight zero-degree scope straight down through the abdominal,” he said. I go in through the optiview and go down through the abdominal wall layers under direct vision of the straight zero-degree scope almost touching the tissue— that’s 2D. Once I get inside the abdominal cavity and insufflate with gas, I switch to 3D.” Similarly, Dr. Clements has switched from 2D to 3D when inserting the visual entry trocar during bariatric surgery. “A short focal length, a centimeter or less, will require you to switch to 2D,” he said.
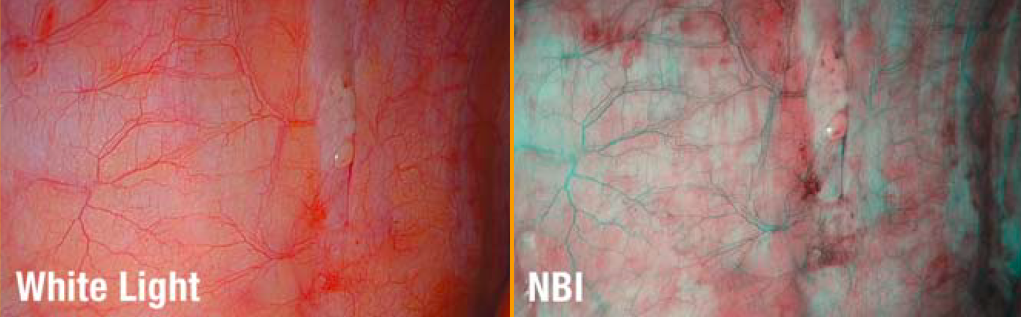
The system also includes narrow band imaging (NBI) technology, to enhance the visualization of vascular structures, such as capillaries, veins, and arteries, during laparoscopic and endoscopic procedures (Figure 5). Dr. Cohen finds this feature useful in distinguishing one tissue from another in Nissen fundoplications for reflux. “In this surgery, you have to wrap part of the stomach around the junction of the esophagus and the stomach, and it has to be in a very specific spot—the GE [gastroesophageal] junction. In order to differentiate esoph- ageal tissue from stomach tissue,” he said, “we use the NBI wavelength because it helps us identify the line very easily.”
Clinical Implications
A number of advanced laparoscopic surgeons are reporting that, in their experience, the ENDOEYE system has shown a number of benefits specific to particular laparoscopic surgeries, as demonstrated by a series of in-house research studies conducted by a number of advanced laparoscopic surgeons.
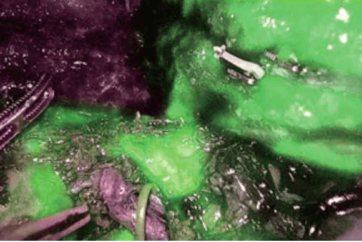
In bariatric procedures, surgeons evaluated the positive benefits of the deflectable videoscope, the universal platform, and reported positive benefits including the restoration of depth perception. They found that the bird’s-eye view made it easier to check the angle of His, create the gastric pouch, identify the ligament of Treiz, and create the gastrojejunal anastomosis.23 Physicians also reported that the universal platform afforded the advantage of allowing them to check for bleeding and/or leaks on the staple line from the inside and that the restoration of depth perception added value in terms of dissection while creating the gastric pouch, particularly for the ability to view the back of the stomach.24 Additionally, suturing was eased by 3D visualization.24
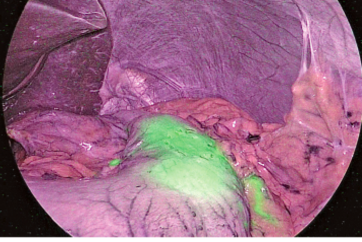
In sigmoidectomy, surgeons found the deflectable tip gave them a potentially safer view for dissecting the mesenterium; in contrast working with conventional equipment in such a small area, the camera and energy device are close together, which often results in fogging of the camera’s tip.25 Observing structures in 3D also helped surgeons define the dissection plane, making dissection easier and faster.25 During the lateral dissection portion of the procedure, the articulating tip allowed surgeons to view critical structures from the optimal angle, even for the splenic flexure, which can be difficult to visualize using a rigid laparoscope. In theory, this could reduce the risk for splenic injury. As with mesenteric dissection, 3D visualization made it easier to define the dissection plane for greater precision and safety.25
With rectal mobilization, the angulation allowed surgeons to observe the sigmoid and rectum from multiple angles, enhancing the safety and precision of dissection, whereas 3D visualization allowed for a better view of the typically difficult-to-access pelvic floor.25 The ENDOEYE system also made it easier to insert the anvil into the circular stapler, thus assisting anastomosis.25
In hysterectomy, the ability to view structures from a variety of angles was tremendously beneficial. The articulating design helped surgeons evaluate adhesions from the back and sides to make sure they steered clear of the bowel while taking the adhesions down.26 When ligating uterine arteries, being able to obtain an optimal front view made it easier to ensure the energy source was in the right place, reducing the risk for bleeding. In colpotomy, the articulating design gave surgeons a 360-degree view to avoid damaging surrounding organs with the bipolar hook used to separate the vagina from the uterus.26
The utility of 3D visualization was equally apparent in identifying the anatomy (eg, preserving the uterine artery and ureter during dissection of the layer of broad ligament from the uterine cervix). It also facilitated the division of theadnexa of uterus and ligament, helping surgeons identify the surgical plane and ascertain how deep they are in the anatomy.26 Furthermore, 3D visualization greatly assisted in suturing, helping surgeons to see which way the needle is pointing.26
In prostatectomy, the ENDOFLEX system made it easier to identify the plane between the urethra and dorsal vein complex, which could reduce risk for injury to the latter.27 It also appeared to make it easier to dissect prostatic pedicles while preserving the neurovascular bundle.27 The system also helped surgeons to suture as precisely as needed to create the urethrovesical anastomosis.27
The perception of depth lends itself to any type of laparoscopic procedure. “You can gain benefit from 3D in any operation,” Dr. Clements said. “I find that even in something as common as a laparoscopic cholecystectomy you gain benefits because you can see the triangle of Calot better than you can see it in 2D.” Similarly, Dr. Cohen added, “Just because a procedure is common doesn’t mean it’s simple. [3D] really helps you in a gallbladder operation, where you can’t always identify the duct or the artery—this gives you a better view than you’ve ever had before.”
Some surgeons feel that the greatest value of 3D will be seen in the most complicated types of procedures, making it easier to carry out some of the more demanding tasks of laparoscopic surgery. “I think we will get the most benefit from working in 3D when we’re doing fine dissection and intracorporeal suturing, and when we’re working in deep cavities— such as the pelvis for a low anterior resection or the hiatus in obesity surgery,” Dr. Lutfi said. “In cases such as large para- esophageal hernia repair, depth perception is critical for fine dissection up in the chest and suturing next to nearby critical structures; you want to see clearly where your scissor is cutting and your needle is landing.”
‘You definitely notice the difference right away, but it doesn’t feel unusual, and there really is no learning curve. It is as if you were walking around with one eye closed, and suddenly you open it. You don’t have to adjust to that.’
—Brett Cohen, MD, FACS
Leveling the Learning Curve
Surgery today is a far different specialty with more challenging patient populations and complex procedures; thus, training plays a crucial role in ensuring the optimization of patient care. With innovation comes the need for skills assessment and opportunity to hone in on nuances and variations that accompany new instrumentation and technique. Ideally, training should require a short learning curve. With laparoscopy, however, studies have shown that there is a prolonged learning curve for surgeons to familiarize themselves with the minimally invasive 2D approach.28
In 2013, Mattar et al conducted a multidomain global assessment of general surgery graduate trainees entering accredited surgical subspecialty specialties in North America to investigate their level of readiness by surveying their program directors. The survey included 46 quantitative questions distributed across 5 domains and at least 1 reflective qualitative question or domain. An analysis of laparoscopic skills showed that nearly 33% of the trainees could not perform a laparoscopic cholecystectomy. Additionally, 26% were unable to recognize anatomical planes, 30% were unable to manipulate tissue without causing trauma, and 56% were unable to suture.29
For most surgeons, particularly residents, the challenge is being able to translate 2D visualization into tangible imaging to carry out the different surgical processes—dissecting, grasping, and suturing. “It sounds crazy, but with laparoscopic surgery we spend years teaching ourselves how to interpret a 2D image and convert that into 3D,” said Dr. Wilson, who is in charge of laparoscopic and minimally invasive skills training for his institution’s residency program. “I do a lot of research on this very thing: How do we teach laparoscopic surgery to residents?” he continued. “Of course, it depends on the individual. In our current practices it takes every bit of a physician’s surgical training, which is what they’ve already done through medical school, then 5 years of general surgery training. The majority of residents don’t feel comfortable with advanced cases without doing a fellowship in minimally invasive surgery, and part of it is because of that [interpretation of the 2D image],” he said. “[With the ENDOEYE system] you don’t have to learn to convert the image, so it’s inherent that that should translate into greater precision, greater speed, and should ultimately help us do a job we want to do better.”
Surgeons have found the adjustment to 3D requires minimal time. “You definitely notice the difference right away, but it doesn’t feel unusual, and there really is no learning curve,” Dr. Singer said. “It is as if you were walking around with one eye closed, and suddenly you open it. You don’t have to adjust to that,” Dr. Cohen added.
Dr. Clements found the adjustment was fairly instanta- neous. “It was so easy, so intuitive. I wear safety glasses in the OR anyway, so instead of the safety glasses I just put on my polarizing glasses and that was it.” Dr. Lutfi agreed with his colleagues but acknowledged some initial frustration associated with the novelty of the laparoscopy. “I have seen a few surgeons get a little frustrated with the change in the way they look at things, but most [clinicians] are very impressed and are immediately able to adjust to it,” he said.
Dr. Michelotti suggested that surgeons using the ENDOEYE system position the monitor close for the best effect. “The closer you have the monitor, the more of your visual field it occupies. With 3D, I think it’s crucial to have the monitor as close as possible so that you can appreciate the 3D depth perception in most of your visual field,” he said. Additionally, Dr. Michelotti observed that the images move much faster than they do with a standard laparoscope. “It takes a little time to get used to the controls of the camera,” he said. “You need to make sure you don’t overcompensate.”
Because the articulating laparoscope involves transitioning from the angled scope to the use of the flexible tip, less experienced surgeons may initially struggle with the ENDOEYE system. “I do a lot of single-incision surgery with a flexible-tip laparoscope, so I’m already familiar with [this feature],” Dr. Lufti said. “Some of my residents struggle even with the 30-degree scope because they’re not used to it, as few of our faculty surgeons never made the switch to the angled scope. Going from the angled scope to the flexible tip is a natural evolution but also a cultural change, and some people feel that it’s cumbersome. Once you adjust, however, it becomes comfortable. Residents in fact struggle going back to 2D laparoscopy after leaving their laparoscopic rotation with me.”
Despite their established proficiency with standard 2D laparoscopy, experienced surgeons also may benefit from the greater ease that 3D affords. Studies conducted in recent years evaluating the effect of 3D laparoscopy on surgeons at various levels of experience—from medical students to advanced surgeons—using simulated surgical models found that most generally performed faster and safer when they were able to visualize tasks with restored depth perception.7 One study including both students and advanced surgeons found that the use of a 3D system resulted in fewer mistakes and faster execution of tasks for all participants, and that the surgeons specifically saved time carrying out more difficult tasks.30
Recently, Dr. Singer and his colleagues conducted a formal study with a simulated surgical model comparing the performance of 12 residents as well as 12 attending surgeons in their timing on a variety of tasks such as bead transfer, suturing, and tying.13 “[The 3D system] improved the time to complete each one of those tasks. So we feel it has the potential to facilitate not just training tasks, but also clinical use,” he said. “We have yet to show that, but in our lab we were really impressed with the impact of 3D on everyone for completing very specific tasks that rely on very specific movements.”
When it came to grasping, surgeons were able to complete the task 25% faster and with 80% fewer errors using 3D rather than 2D technology. The pace of suturing, dissecting, and eye-letting were accelerated by 35%, 10%, and 15%, respectively, with the restoration of depth perception. In less-experienced surgeons, 3D technology significantly improved the learning curve for both grasping and peg transfer.13
If ENDOEYE FLEX 3D proves to speed procedures and saves time in the OR, this will have many implications for cost savings and safety. In the hands of experienced laparoscopic surgeons who honed their craft before HD and 3D options were available, the time savings may be negligible. But it may be tremendously useful in helping new surgeons tackle the laparoscopic learning curve.
“I don’t think using the ENDOEYE would have much impact for someone who has done thousands of cases and [has] overcome the limitations of 2D laparoscopy,” Dr. Clements said. “But it has really had an impact on the residents and first assistants who help me do the cases. It cuts down on the delay of them accomplishing a task like picking up a suture, which they can do much faster in 3D.”
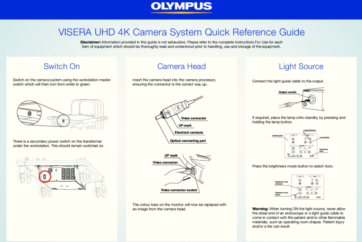
Standardizing Surgical Technology To Reduce Costs
As health care continues to focus on the need to contain costs while optimizing patient care, opportunities to consolidate technology are essential. Because the ENDOEYE FLEX 3D can be added to the Olympus EVIS EXERA III Universal Imaging System, surgery suites are able to standardize equipment, thus reducing the need for excess equipment in the confined space (Figure 6). Additionally, the ENDOEYE FLEX 3D is part of a universal platform that supports more than 100 different endoscopes. “That is a huge advantage of this system. Olympus, as far as I am aware, is the only system that allows you to plug all of your devices into one main component,” Dr. Cohen said. “If I was using [a competing system’s] laparoscope and I wanted to use an endoscope at the same time, I would need a separate tower made by another company. With the ENDOEYE system and Olympus equipment, all I need to do is either unplug my laparoscope or plug the endoscope into the same imaging tower and have both images up at the same time.” This approach reduces the capital investment, associated with asset management, its maintenance, and training.

Figure 6.
The ENDOEYE FLEX 3D is part of a universal platform to standardize equipment in the surgery suite. It can be added to the Olympus EVIS EXERA III Universal Imaging System, which supports more than 100 different endoscopes.‘3D helps us appreciate depth, suture more accurately, see structures easily and see the planes between organs better. That depth perception will translate into a safer and more efficient procedure, which is why people will eventually adopt it.’
—Rami Lutfi, MD, FACS
Conclusion
Similar to how HD replaced standard definition, and 3-chip cameras replaced 1-chip cameras, the ENDOEYE FLEX 3D has the potential to become the gold standard for laparoscopy. As an articulating laparoscope with 3D visualization, the ENDOEYE FLEX 3D restores the ability to access peritoneal cavity directly while adhering to a minimally invasive approach.
Dr. Lutfi believes that safety and efficiency will play a role in reinforcing the importance of 3D laparoscopy and which system is integrated as the standard. “3D helps us appreciate depth, suture more accurately, see structures easily and see the planes between organs better,” he said. “That depth perception will translate into a safer and more efficient procedure, which is why people will eventually adopt it.” Patients, too, might be interested to know that that their surgeons are using more advanced equipment that helps them do their job better, even if [patients] don’t completely understand how it works. “Patients come to us for robotic surgery without really knowing what the robot is or what advantages it provides,” Dr. Lutfi said. “But I think being able to tell the patient we have something that improves minimally invasive surgery and gives us better visualization and more accuracy will certainly help us market the practice.”
The preliminary data and experiences of those who have used the ENDOEYE FLEX 3D system using a surgical model suggest it restores depth perception and enhances anatomical visualization; adds speed and precision to grasping, suturing, and dissecting; and levels the learning curve for surgeons-in-training as well as more experienced surgeons.
Those theories are being put to the test. “We need to keep an open mind and evaluate this technology thoroughly— and not make fast decisions about whether or not to adopt it,” Dr. Lutfi said. He and his team are currently assembling a randomized controlled trial to evaluate speed, efficiency, errors of performance, suture handling, and soft tissue dis- section in residents and in mid-expertise attending surgeons comparing 2D and 3D. “This will help us really answer those questions with certainty so that we have data to back up our decisions,” he said.
References
- Ramirez PT, Soliman PT, Schmeler KM, dos Reis R, Frumovitz M. Laparoscopic and robotic techniques for radical hysterectomy in patients with early-stage cervical cancer. Gynecol Oncol. 110(suppl 2):S21-S24.
- Randall J, Lord B, Fulham J, Soin B. Parastomal hernias as the predominant stoma complication after laparoscopic colorectal surgery. Surg Laparosc Endosc Percutan Tech. 2012;22(5):420-423.
- Shabanzadeh DM, Sorensen LT. Laparoscopic surgery compared with open surgery decreases surgical site infection in obese patients. Ann Surg. 2012;256(6):934-945.
- Kennedy GD, Heise C, Rajamanickam V, Harms B, Foley EF. Laparoscopy decreases postoperative complication rates after abdominal colectomy: results from the national surgical quality improvement program. Ann Surg. 2009;249(4):596-601.
- Baumert H, Ballaro A, Dugardin F, Kaisary AV. Laparoscopic versus open simple prostatectomy: a comparative study. J Urol. 2006;175(5):1691-1694.
- Sohn W, Lee HJ, Ahlering TE. Robotic surgery: review of prostate and bladder cancer. Cancer J. 2013;19(2):133-139.
- Tanagho YS, Andriole GL, Paradis AG, et al. 2D versus 3D visualization: impact on laparoscopic proficiency using the fundamentals of laparoscopic surgery skill set. J Laparosendosc Adv Surg Tech A. 2012;22(9):865-870.
- Sinha R, Sundaram M, Raje S, Rao G, Sinha M, Sinha R. 3D laparoscopy: technique and initial experience in 451 cases. Gynecol Surg. 2013;10:123-128.
- Izquierdo L, et al. 3D advances in laparoscopic vision. Eur Urol Rev. 2012;7(2):137-139.
- Yamauchi Y, Shinohara K. Effect of binocular stereopsis on surgical manipulation performance and fatigue when using a stereoscopic endoscope. Stud Health Technol Inform. 2005;111:611-614.
- Yim GW, Kim YT. Robotic surgery in gynecologic cancer. Curr Opin Obstet Gynecol. 2012;24(1):14-23.
- 12.Olympus. Data on File; 2013.
- Singer M, Endres J, Yetasook A, et al. Evaluation of 3-D laparoscopy to complete surgical skills task. Presented at: the 2013 Annual Meeting of the Society of American Gastrointestinal Endoscopic Surgeons (SAGES); April 17-20, 2013; Baltimore, MD. Poster P520.
- Perugini RA, Callery MP. Complications of laparoscopic surgery. In: Holzheimer RG, Mannick JA, editors. Surgical treatment: evidence-based and problem-oriented. Munich: Zuckschwerdt;2001. http://www.ncbi.nlm.nih.gov/books/NBK6923/. Accessed March 24, 2014.
- Moore MJ, Bennett CL. The learning curve for laparoscopic cholecystectomy. The Southern Surgeons Club. Am J Surg 1995;170(1):55-59.
- Badani KK, Bhandari A, Tewari A, Menon M. Comparison of two- dimensional and three-dimensional suturing; is there a difference in a robotic surgery setting? J Endourol 2005;19(10):1212-1215.
- Neri V, Ambrosi A, Di Lauro G, Fersini A, Valentino TP. Difficult cholecystectomies: validity of the laparoscopic approach. JSLS. 2003;7(4):329-333.
- Wagner OJ, Hagen M, Kurmann A, Horgan S, Candinas D, Vorburger SA. Three-dimensional vision enhances task perfor- mance independently of the surgical method. Surg Endosc. 2012;26(10):2961-2968.
- Voitk AJ. The learning curve in laparoscopic inguinal hernia repair for the community general surgeon. Can J Surg 1998;41(6): 446-450.
- Kong SH, Oh BM, Yoon H, et al. Comparison of two- and three- dimensional camera systems in laparoscopic performance: a novel 3D system with one camera. Surg Endosc. 2010;24(5):1132-1143.
- Buchs NC, Morel P. Three-dimensional laparoscopy: a new tool in the surgeon’s armamentarium. Surg Technol Int. 2013;23:19-22.
- Shafer A, Boggess JF. Robotic-assisted endometrial cancer staging and radical hysterectomy with the da Vinci surgical system. Gynecol Oncol. 2008;111(2 suppl):S18-S23.
- Falk V, Mintz D, Grunenfelder J, Fann JI, Brudon TA. Influence of three-dimensional vision on surgical telemanipulator performance. Surg Endosc. 2001;15(11):1282-1288.
- Bariatric procedures. Olympus. Data on File; 2013.
- Left colectomy (sigmoidectomy).Olympus. Data on File; 2013.
- Laparoscopic hysterectomy. Olympus. Data on File; 2013.
- Prostatectomy. Olympus. Data on File; 2013.
- McLachlan G. From 2D to 3D: the future of surgery? Lancet. 2011;378(9800):1368.
- Mattar SG, Alseidi AA, Jones DB, et al. General surgery residency inadequately prepares trainees for fellowship: results of a survey of fellowship program directors. Ann Surg. 2013;258(3):440-449.
- Storz P, Buess GF, Kunert W, Kirschniak A. 3D HD versus 2D HD: surgical task efficiency in standardized phantom tasks. Surg Endosc. 2012;26(5):1454-1460.
Disclosures: Drs. Clements, Cohen, and Michelotti reported no relevant financial disclosures. Dr. Lutfi reported that he is a consultant for Allergan, Inc, Ethicon Endo-Surgery, and Gore. Dr. Singer reported that he is a consultant for OLYMPUS and is on the speakers’ bureau for Cubist Pharmaceuticals. Dr. Wilson reported that he is a consultant for OLYMPUS and has received honoraria from Bard.
Disclaimer: This monograph is designed to be a summary of information. While it is detailed, it is not an exhaustive clinical review. McMahon Publishing, OLYMPUS, and the authors neither affirm nor deny the accuracy of the information contained herein. No liability will be assumed for the use of this monograph, and the absence of typographical errors is not guaranteed. Readers are strongly urged to consult any relevant primary literature.
Copyright © 2014, McMahon Publishing, 545 West 45th Street, New York, NY 10036. Printed in the USA. All rights reserved, including the right of reproduction, in whole or in part, in any form.
- Keyword
- Content Type