Impact of Intra‐Operative Endoscopy in Evaluation of Digestive Anastomosis
A. Facts
- In surgeries requiring resection and anastomosis of the intestine a good outcome depends on the successful healing of the anastomosis. Flexible endoscopy plays a fundamental role in the clinical monitoring of surgical digestive anastomosis1.
- The site of the anastomosis is one of the major problems in the digestive surgery. Higher incidence of anastomotic failure is associated with low colorectal2 3 and esophagus-jejunal4 5 anastomosis.
- No differences in anastomotic colorectal leak are reported between laparoscopic and open surgery6 , even if a lower incidence in the laparoscopic one is reported in a recent review (3.0-17 % vs 0-23.0 %)7.
- The successful healing of an anastomosis is affected by a variety of factors. Without adequate vascular supply (blood flow), the bowel ends become unviable with inevitable anastomotic dehiscence8.
B. Endoscopic Evaluation
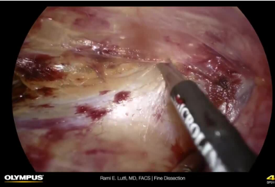
- At the time of performing an anastomosis, surgeons work to ensure anastomotic success by making the two ends of the bowel as tension‐free as possible. This is done by adequate mobilization of the bowel and by joining ends of the bowel only if they appear pink and health ensuring they are properly aligned without any twist.
- Once the anastomosis is complete, intra‐operative endoscopy can be utilized for evaluation of patency and integrity of GI tract anastomosis during the surgical procedure9.
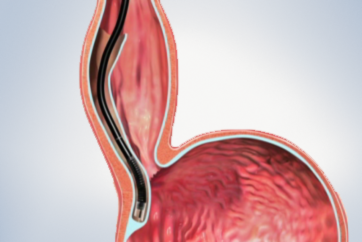
- When the resection and anastomosis is complete the morphology of the normal tract is altered. An accurate endoscopic technique to essential to describe the morphology of the new intestinal tract10.
- Visualization of the bowel externally might be inadequate to assess the risk of dehiscence, since external surface of the bowel and may not be representative of what is happening internally (in the mucosa and submucosa)8.
C. Intra-Operative Endoscopy (IOE) in Upper GI Tract Surgery
1. Laparoscopic Roux‐en‐ Y Gastric Bypass (LRYGBP)
- The commonest site for a leak after a LRYGBP is the gastrojejunal anastomosis (GJA) site with reported incidences from 0 to 5.2 %11 12.
- The detection of early postoperative leaks traditionally was based on upper GI series. Intraoperative assessment of the GJA, however, in a study performed in 245 patients (Madan et al.) showed that an upper GI series has a sensitivity of 75 % and a positive predictive value of 67 % in the detection of anastomotic leaks13.
- The main advantage of intra‐operative endoscopy is that it can be used14 15 16:
1. to detect leaks but also to treat them in the operating room
2. to ensure that the anastomosis isn’t too tight
3. to treat leaks from the GJA and from the gastric pouch, application of fibrin sealant, bovine pericardial strips, and omental patches has been used with variable success - One study compared IOE to the methylene blue test and found the low pressure infusion of methylene blue to be less sensitive to leak detection than air insufflation by endoscopy. This study showed that a 10% incidence of leaks was reduced to 3.8% owing to suture strengthening after intra‐operative gastroscopy (IOG)17.
- Champion et al. concluded in their study that with the aid of IOG postoperative leakage can be reduced from 3.8 to 0.36 %18.
- Intra‐operative endoscopy has been shown to reduce postoperative morbidity. One study has reported a 0% postoperative anastomotic leakage rate in more than 250 patients using IOG19.
- Sekhar et al. found no postoperative leaks in 340 patients who underwent LRYGB, because 56 intraoperative leaks were detected and corrected by IOG20.
- Alaedeen et al. demonstrated, in a study assessing 400 patients undergoing LRGYB, that IOG reduced postoperative leak rates from 4 to 0.5 % and mortality from 1 to 0 %21.
- GI bleeding, another important complication after gastric bypass surgery, has an incidence varying from 0.5 % for open to 4.4 % for the laparoscopic approaches respectively. Intraluminal bleeding can occur from the staple lines and can be missed during the procedure unless an IOG is carried out22 23.
2. Technique for IOG During Laparoscopic Gastric Bypass
- The upper esophageal sphincter is intubated under vision, a jaw thrust may helpful.
- The proximal pouch is inspected; the endoscope is then gently guided through the anastomosis into the Roux limb.
- A bowel clamp is placed on the intestinal limb distal to the GJA.
- The table is leveled and operative field containing the anastomosis is filled with sterile normal saline to cover the proximal pouch and anastomosis.
- The area is then irrigated until it is cleared from blood and operative debris.
- The gastroscope is then withdrawn into the proximal pouch, and the anastomosis reinspected with continuous insufflation.
- Before withdrawal the air that has been introduced is aspirated completely.
- In case of persistent air leak, the endoscope is left in situ till the repair of gastrojejunostomy suture line.
- The procedure is repeated.
3. Pit falls during an intra? Operative endoscopy is shown below:
- Care during intubation of the esophagus, Intubation under clear visualization to avoid pharyngeal tears.
- The gastroscope controls must be in the unlocked position when inspecting the proximal gastric pouch to prevent pouch tear.
- Air embolism can occur in all ages, due to interruption of the mucosal barrier during the procedure. It is mandatory to carefully perform endoscopic maneuvers and air insufflation in order to avoid this key complication24.
D. Intra‐Operative Endoscopy in Colorectal Surgery
- The most serious complications of laparoscopic colorectal surgery are anastomotic complications such as leakage and bleeding. Surgeons have tried testing the anastomosis, especially in the distal colon and rectum by using air25 or by using methylene blue enema26.
- Intra‐operative colonoscopy allows detection of the bleeding source and of leaks. In a recent study carried out in 60 patients, intra‐operative air testing, with IOE, of colorectal anastomosis was considered an effective method for prevention of anastomotic dehiscence, incidence was 50% lower in comparison with the control group27
References
- Cotton P, Williams CB (1996) Practical gastrointestinal endoscopy. Blackwell Science, Oxford
- Warschkow R, Steffen T, Thierbach J et al (2011) Risk factors for anastomotic leakage after rectal cancer resection and reconstruction with colorectostomy. Surg Oncol 18(10):2772-2782
- Boccola MA, Buettner PG, Rozen WM et al (2011)Risk factors and outcomes for anastomotic leakage in colorectal surgery: a singleinstitution analysis of 1576 patients. World J Surg 35(1):186-195
- Deguchi Y, Fukagawa T, Morita S et al (2012) Identifi cation of risk factors for esophagojejunal anastomotic leakage after gastric surgery. World J Surg 36(7):1617-1622
- Markar SR, Arya S, Karthikesalingam A et al (2013) Technical factors that affect anastomotic integrity following esophagectomy: systematic review and metaanalysis. Ann Surg Oncol 20(13):4274-81
- El‐Gazzaz G, Geisler D, Hull T et al (2010) Surgery: risk of clinical leak after laparoscopic versus open bowel anastomosis. Surg Endosc 24(8):1898-1903
- Hotta T, Yamaue H (2011) Laparoscopic surgery for rectal cancer: review of published literature 2000- 2009. Surg Today 41(12):1583-1591
- Telem D, Chin E, Nguyen S et al (2010) Risk factors for anastomotic leak following colorectal surgery. A case?control study. Arch Surg 145:371-375
- Espiner HJ, Salmon PR, Teague RH et al (1973) Operative colonoscopy. Br Med J 24:453-454
- Hassan C, Bretthauer M, Kaminski MF et al (2013) Bowel preparation for colonoscopy: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy 45:142-150
- The ASMBS Clinical Issues Committee (2009) ASMBS guideline on the prevention and detection of GI leak after gastric bypass including the role of imaging and surgical exploration. Surg Obes Rel Dis 5:293-296
- Alasfar F, Chand B (2010) Intraoperative endoscopy for laparoscopic Roux‐en‐Y gastric bypass: leak test and beyond. Surg Laparosc Endosc Percutan Tech 20:424-427
- Madan AK, Stocklein HH, Ternovits CA et al (2007) Predictive value of upper gastrointestinal studies versus clinical signs for gastrointestinal leaks after laparoscopic gastric bypass. Surg Endosc 21:194-196
- Sekhar N, Tourquati A, Lutfi R et al (2006) Endoscopic evaluation of the gastrojejunostomy in laparoscopic gastric bypass. Surg Endosc 20:199-201
- Panieri E, Dent DM (2003) Implications of anastomotic leakage after total gastrectomy for gastric carcinoma. S Afr J Surg 41:66-69
- Lamb PJ, Griffi n SM, Chandrashekar MV et al (2004) Prospective study of routine contrast radiology after total gastrectomy. Br J Surg 91:1015-1019
- Ramanathan R, Ikramuddin S, Gourash W et al (2000) The value of intraoperative endoscopy during laparoscopic roux‐en‐Y gastric bypass. Surg Endosc 14:212
- Champion JK, Hunt T, Delisle N (2002) Role of routine intraoperative endoscopy in laparoscopic bariatric surgery. Surg Endosc 16:1663-1665
- Alasfar F, Chand B (2010) Intraoperative endoscopy for laparoscopic Roux‐en‐Y gastric bypass: leak test and beyond. Surg Laparosc Endosc Percutan Tech 20:424-427
- Sekhar N, Tourquati A, Lutfi R et al (2006) Endoscopic evaluation of the gastrojejunostomy in laparoscopic gastric bypass. Surg Endosc 20:199-201
- Alaedeen D, Madan AK, Ro CY et al (2009) Intraoperative endoscopy and leaks after laparoscopic Roux‐en‐Y gastric bypass. Am Surg 75(6):485-488
- Champion JK, Hunt T, Delisle N (2002) Role of routine intraoperative endoscopy in laparoscopic bariatric surgery. Surg Endosc 16:1663-1665
- Wittgrove AC, Clark GW, Tremblay LJ (1994) Laparoscopic gastric bypass, Roux‐en‐Y: preliminary report of 5 cases. Obes Surg 4:353-357
- Akhtar N, Jafri W, Mozaffar T (2001) Cerebral artery air embolism following an esophagogastroscopy: a case report. Neurology 56:136-137
- Griffi th CD, Hardcastle JD (1990) Intraoperative testing of anastomotic integrity after stapled anterior resection for cancer. J R Coll Surg Edinb 35:106-108
- Smith S, McGeehin W, Kozol RA et al (2007) The efficacy of intraoperative methylene blue enemas to assess the integrity of a colonic anastomosis. BMC Surg 1:15-20
- Ivanov D, Cvijanović R, Gvozdenović L (2011) Intraoperative air testing of colorectal anastomoses. Srp Arh Celok Lek 139(5 6):333-338
- Keyword
- Content Type