Prof. Artur Szlubowski
MD, PhD

Maciej Gnass
MD, PhD
Introduction
The discussion on which needle to use for biopsy of parenchymal organs in different clinical cases is still open and there are no unequivocal recommendations. The 23gauge (G) needle was the first to be used in pulmonary diagnostics by K.P. Wang for the diagnosis of tumors in extra-bronchial locations, nota bene he diagnosed small-cell lung cancer this way. It was not until 1989 that he used a special flexible needle for transbronchial biopsy dedicated to bronchoscopy for the diagnosis of sarcoidosis. The technique of conventional transbronchial aspiration biopsy (TBNA) was popularized at the end of the 20th century especially in Japan and Western European countries, while in Poland it has started to be used only at the beginning of the 21st century.
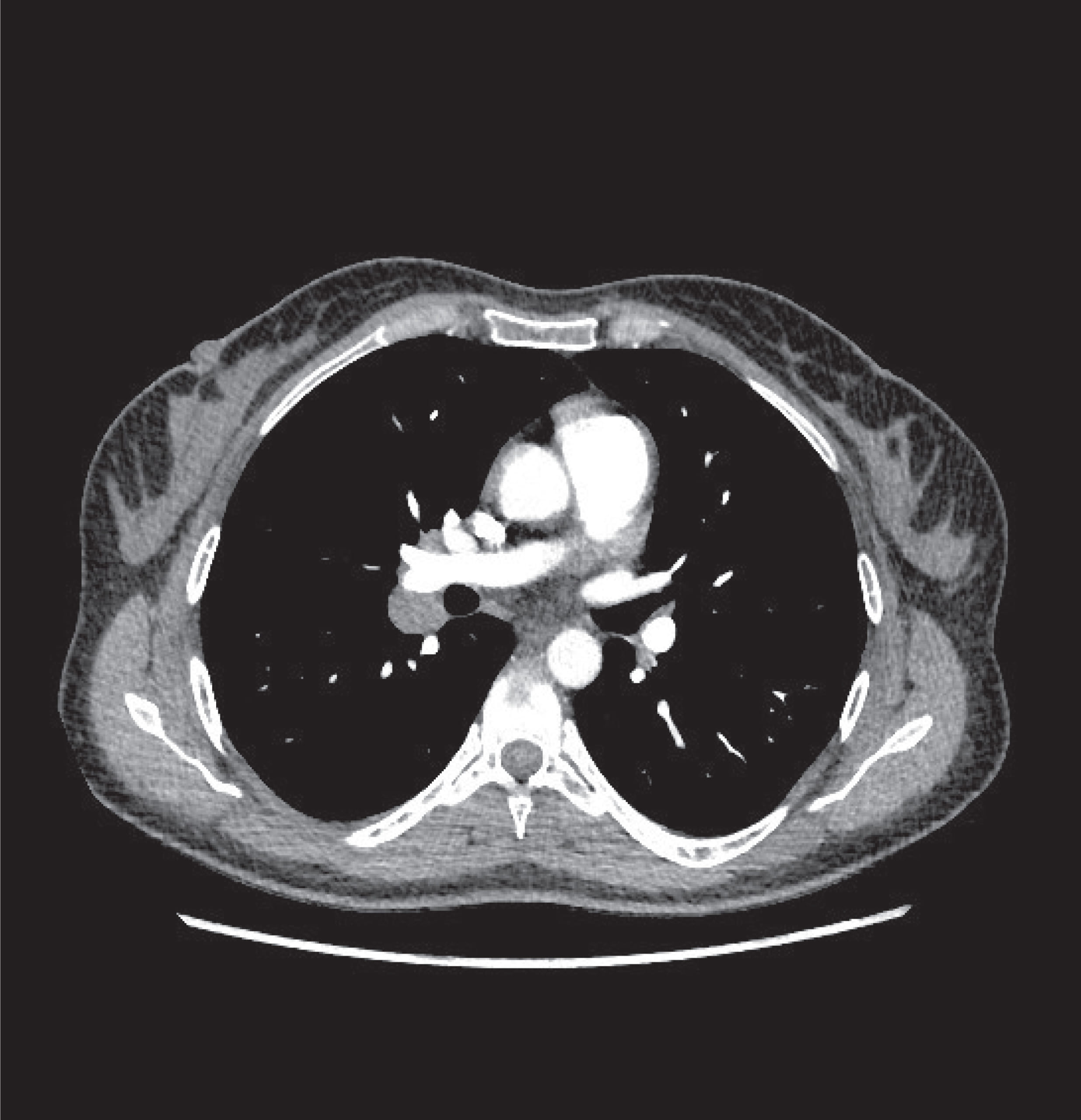
The „semi-blind” biopsy technique itself does not require long training and is not difficult for the bronchoscopist, but the results (especially the false-negative rate) are strongly influenced by the experience and skills of the person performing the examination. This concerns both the interpretation of images obtained from chest CT, based on which the biopsy is planned, and the spatial imagination, and above all the manual skills of the bronchoscopist. The failure to achieve a high diagnostic success rate, which ranges from 35-80%, has not resulted in a significant breakthrough and the technique itself has not been widely accepted by the pulmonological community to this day. However, our long-term experience shows that it is the routine use of conventional TBNA with 13-15mm 22G/21G needles that allows to create a simple automatism of „feeling” the bronchial wall during biopsy.
ViziShot 1 22G/21G
When in 2002 Krasnik M. et al. published the first reports on a new technique of transbronchial biopsy using a videobronchoscope ultrasound with a built-in linear transducer – it was a real breakthrough. In Poland we applied the EBUS-TBNA technique for the first time in 2006, using for the next decade a 40mm ViziShot 22G needle (NA-201SX-4022 Olympus Medical Systems Corporation, Tokyo, Japan). More than 90% of the several hundred publications worldwide, on the efficacy of EBUS-TBNA biopsies is based precisely on the experience of using 22G needles. Interestingly, over the last 15 years, new generations of ultrasound processors have already been introduced several times, the third generation of the BF-UC190F ultrasound bronchoscope (Olympus Medical Systems Corporation, Tokyo, Japan), and the first generation ViziShot needles are compatible with all types of instruments and are still in use. These needles have high reliability, good biopsy repeatability, medium flexibility, allowing the tip of the BF-UC160F-OL8 and BF-UC180F series bronchoscopes (Olympus Medical Systems Corporation, Tokyo, Japan) to bend up to 57°. In the same time, 40mm 21G needles (NA-201SX-4021) were introduced, which, due to their larger diameter, are dedicated more to the diagnosis of advanced lesions, e.g. nodal packets, in order to collect more material for cytological examination, rather than for precise staging and biopsy of several nodal stations. These needles are not as widely recognized and used by the bronchoscopists due to their high stiffness, as they allow the tip of the bronchoscope to be safely angulated to only 45°. Thus, biopsy of some nodal stations, especially bilateral paratracheal ones (2L, 4L, 2R, 4R), may pose a considerable challenge, especially that in most centers, balloons facilitating ultrasound visualization of lesions adjacent to the trachea, are not routinely used. Due to its larger diameter, the material retrieved is more abundant, but also unfortunately more often bloody, so the biopsy is much more suitable for cytoblocks than cytological smears.
Both needles are being attached to the endoscope using a special connector and a simple locking device, which make it easy to insert the needle several times during the procedure. However, the connection of the inserted needle with the vacuum syringe causes some instability in the system, which is controlled by holding both the needle and the bronchoscope with your hand, to keep them in line with the biopsy channel at all times. Moreover, inaccurate placement of the needle lock on the connector most often leads to damage of the biopsy channel.
The sheaths of both types of needles are transparent, which in some situations makes it difficult to visualize them after withdrawal from the biopsy channel. Poor visualization of the sheath and a strong angulation of the scope to obtain better adhesion to the bronchial wall during biopsy (especially after loading 21G needles), have often led to damage of the scope. Both needles, especially the 22G are characterized by a medium sharpness of the tip, which on the one hand is a disadvantage when passing through a rigid bronchial wall, but also an advantage as the needle penetration is better controlled by the bronchoscopist.
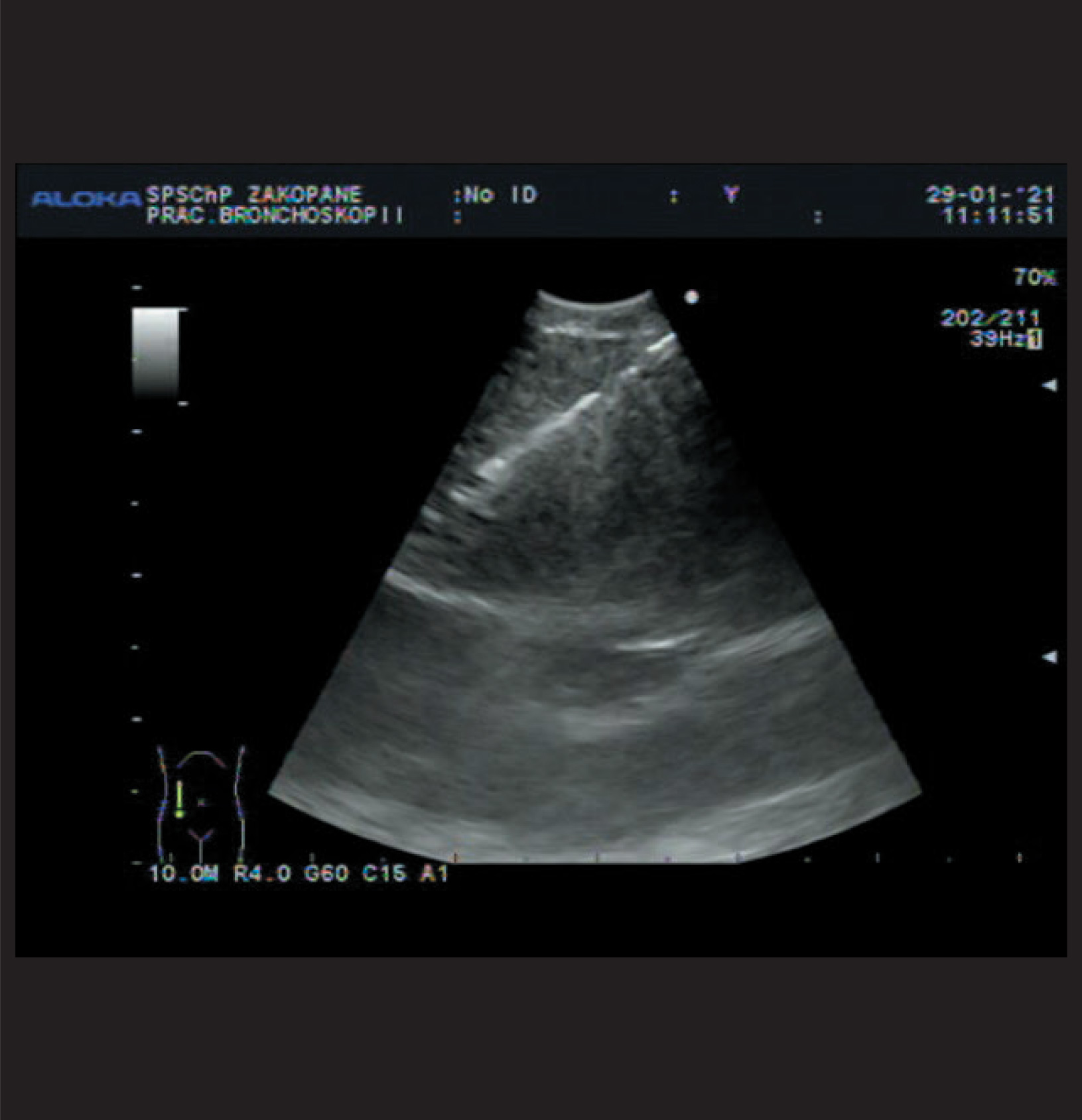
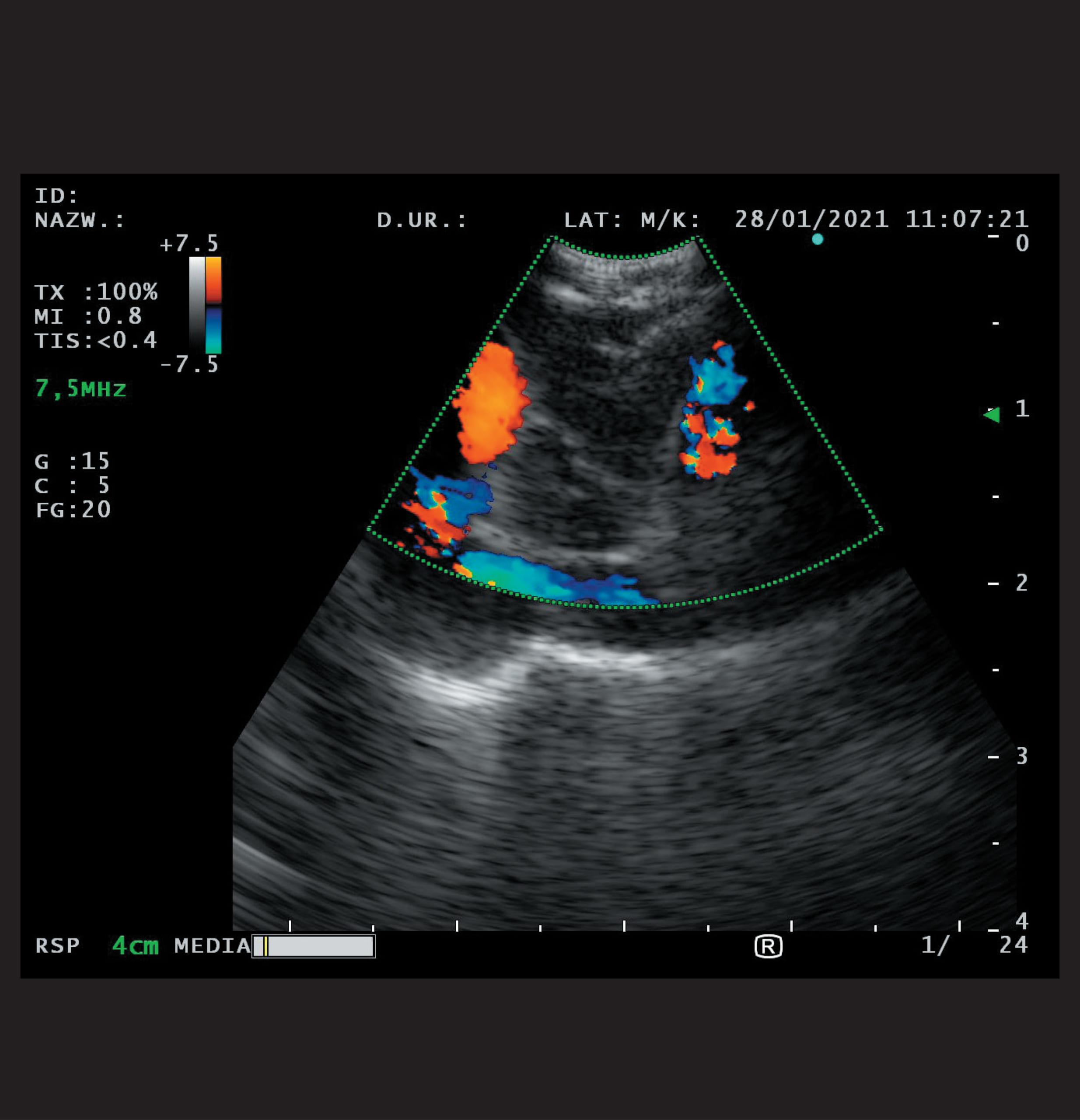
Undoubtedly, familiarity with the conventional TBNA technique and an adequate feeling of resistance during biopsy is very useful here. In both needles the stylets are well fitted to the needle diameter and after using them (in case of inability to inject material with a syringe) very little material remains inside the needle, which is often seen, because the last portion of material injected under syringe pressure onto the slide, is usually small. It is extremely rare that after the first biopsies the needle is clogged with biopsy material – usually a blood clot – and the needle cannot be „unclogged” with the stylet. The visibility of both needles in ultrasound image is good, in all available ultrasound processors, i.e.: EU-C60, EU-ME 1/2, Aloka Alfa 7. The 2016 ACCP (American College of Chest Physicians) guidelines with recommendation strength 1C recommend the use of both needle types in EBUS-TBNA technique, but do not refer to the use of 25G and 19G needles.
ViziShot 2 Flex 19G
In 2015 the first reports started to be published on flexible nitinol 19G needles (Flex 19G, Olympus Respiratory America, Redmond, WA, USA), which are currently already approved as histology ones.
Our experience, and that of several other authors, on the use of 19G needles has been very good, especially with regard to collecting more material for the diagnosis of advanced lung cancer, including immunohistochemical and predictive studies or for the diagnosis of sarcoidosis or even lymphoma. However, Tremblay et al. showed no difference in biopsy efficacy when compared directly with 22G/21G needles in staging lung cancer, similarly Chaddha et al. when obtaining material from advanced lesions.
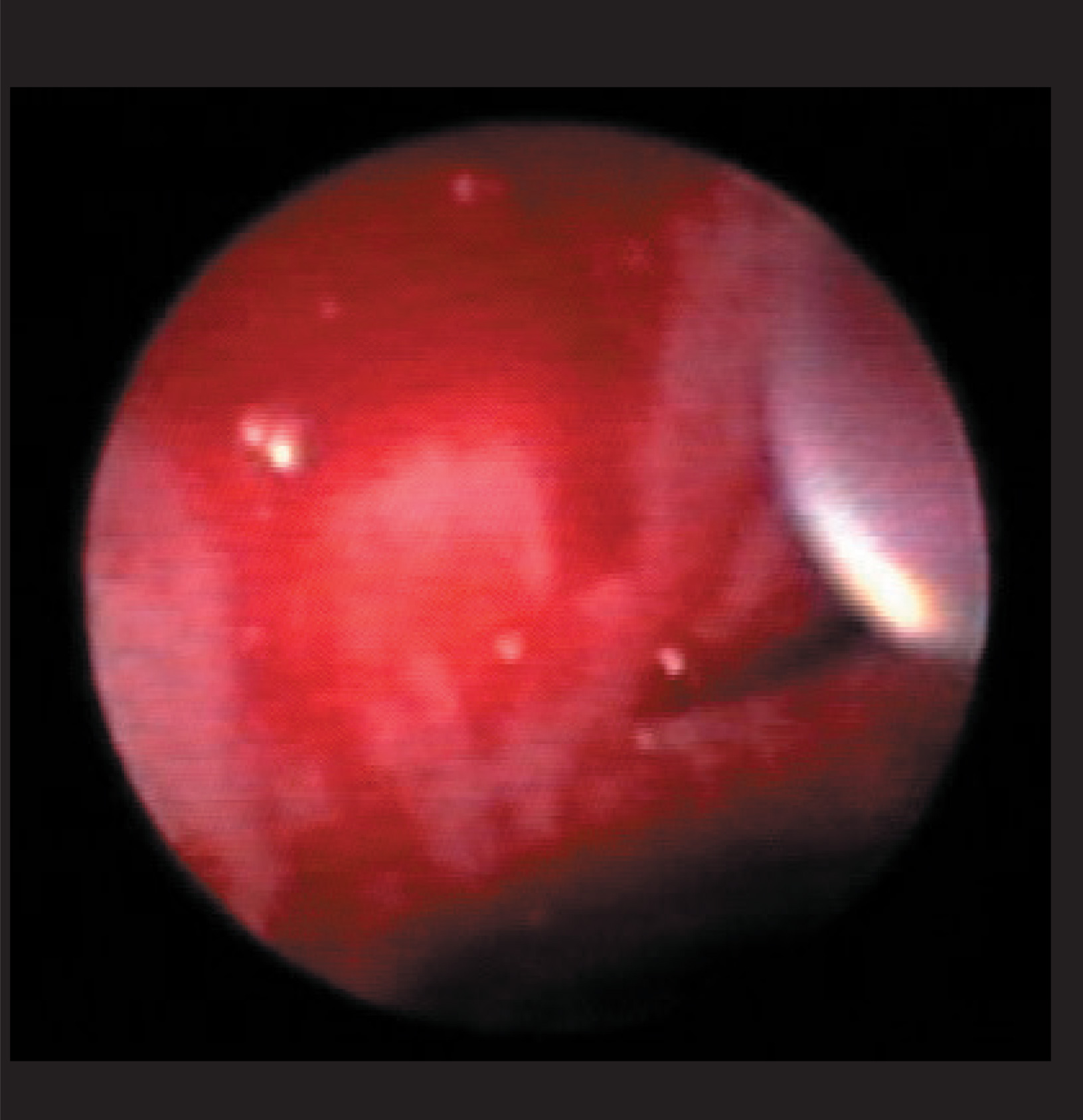
The 19G needle’s significant flexibility allows the device to be angulated up to 78° and to reach difficult locations such as the paratracheal region, both sides. The slightly poorer visibility in the ultrasound image, due to the spiral cut of the needle tip, is compensated for by the excellent stability of the needle once it is inside the lesion itself. The tip of the needle shows good sharpness, which allows for characteristic, reproducible overcoming of the resistance of the hard wall of the bronchus and very good penetration of the tumor or lymph node. Moreover, performing even 2-3 biopsies,always starting with the cytoblock, due to the large amount of, unfortunately usually bleeding contents, is in most cases sufficient to collect an adequate amount of material.
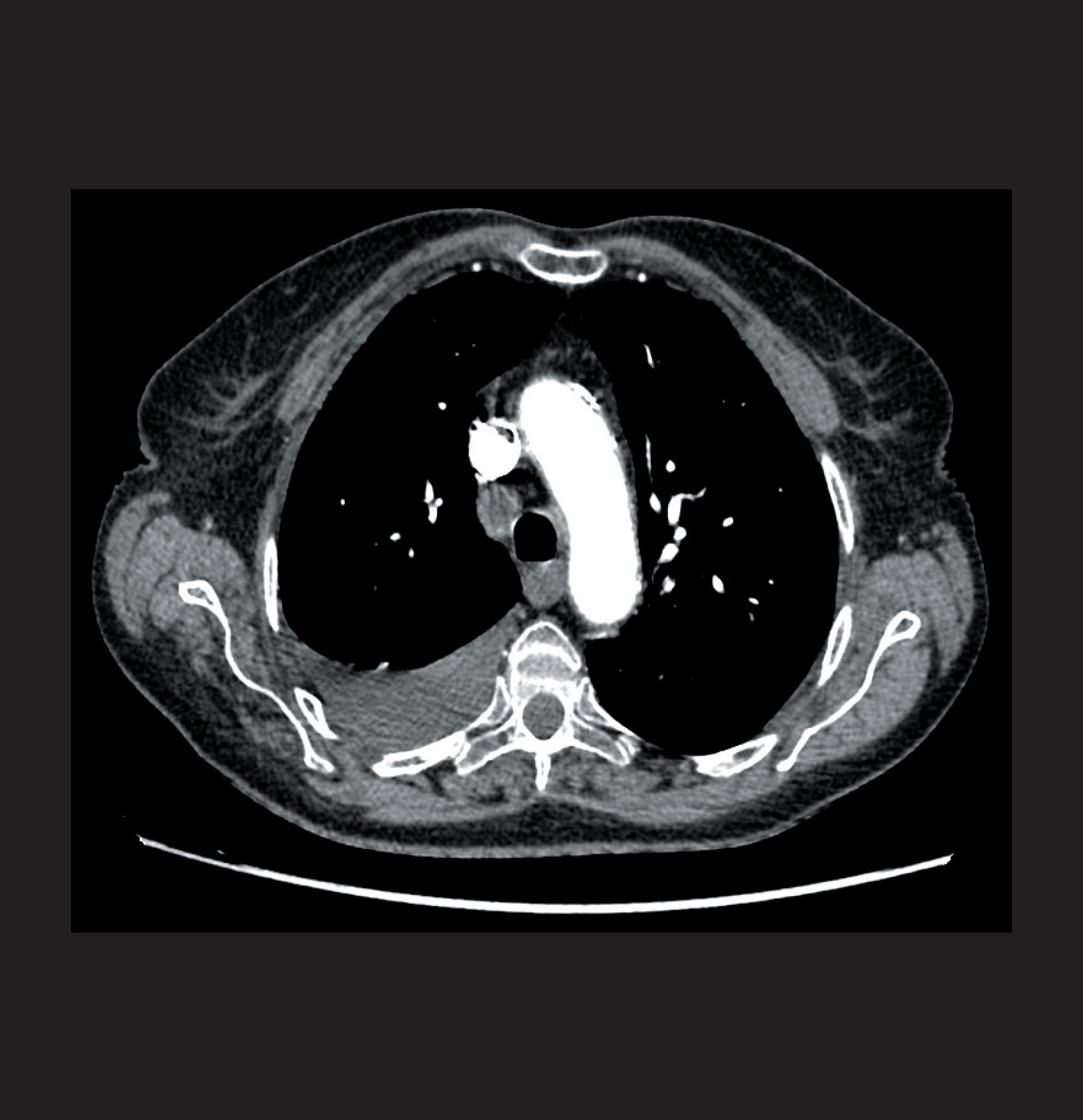
To obtain a similar amount of material with the 22G/21G needle, at least twice as many passages need to be made. Dooms et al. noted that the 19G needle penetrates a larger area of the tumor or lymph node, which may translate into greater detection of mutations in predictive tests, especially those performed by Next Generation Sequencing (NGS). However, we noted the possibility of more hemorrhagic complications after biopsy with a 19G needle, especially of the lymph nodes of both hilar lymph nodes, located just off the branches of the pulmonary artery. When biopsying lung tumors, especially transesophageally, using the EUS-b-FNA technique in the hilar and especially mediastinal locations, there is also a greater possibility of inducing pneumothorax, due to the larger diameter of the needle. However, the greatest limitation to the routine use of this needle is its approximately twice the price, compared to cytological needles. Therefore, it seems that thinner cytologic needles should be used for staging or restaging of lung cancer when there is a need to puncture several mediastinal and hilar nodal stations, sometimes uninvolved lymph nodes <8.5mm. The new generation of 19G needles (NA-U403SX-4019) is equipped, like the other needles of the ViziShot 2 series, with a new more stable fixing system for the bronchoscope.
ViziShot 2 22G/21G
A second, improved generation of both 22G/21G ViziShot 2 needles (NA-U401SX-4021, NA-U401SX-4022) and brand new, thinner 25G needles (Olympus Medical Systems Corporation, Tokyo, Japan) have been present on the market in the same time, for several years. The needles of both generations are compatible with the bronchoscopes with min. 2.0mm working channel.
ViziShot 2 needles in both sizes 22G/21G, although they are the same diameter and show comparable visibility on ultrasound imaging, differ in several aspects compared to their predecessors. They have a stable fixation, adapted to the shape of the bronchoscope handle. The protruding part of the connector should be positioned in such a way that it does not interfere with the needle attachment – its incorrect position may lead to inaccurate needle fixation, which will damage the biopsy channel of the bronchoscope.
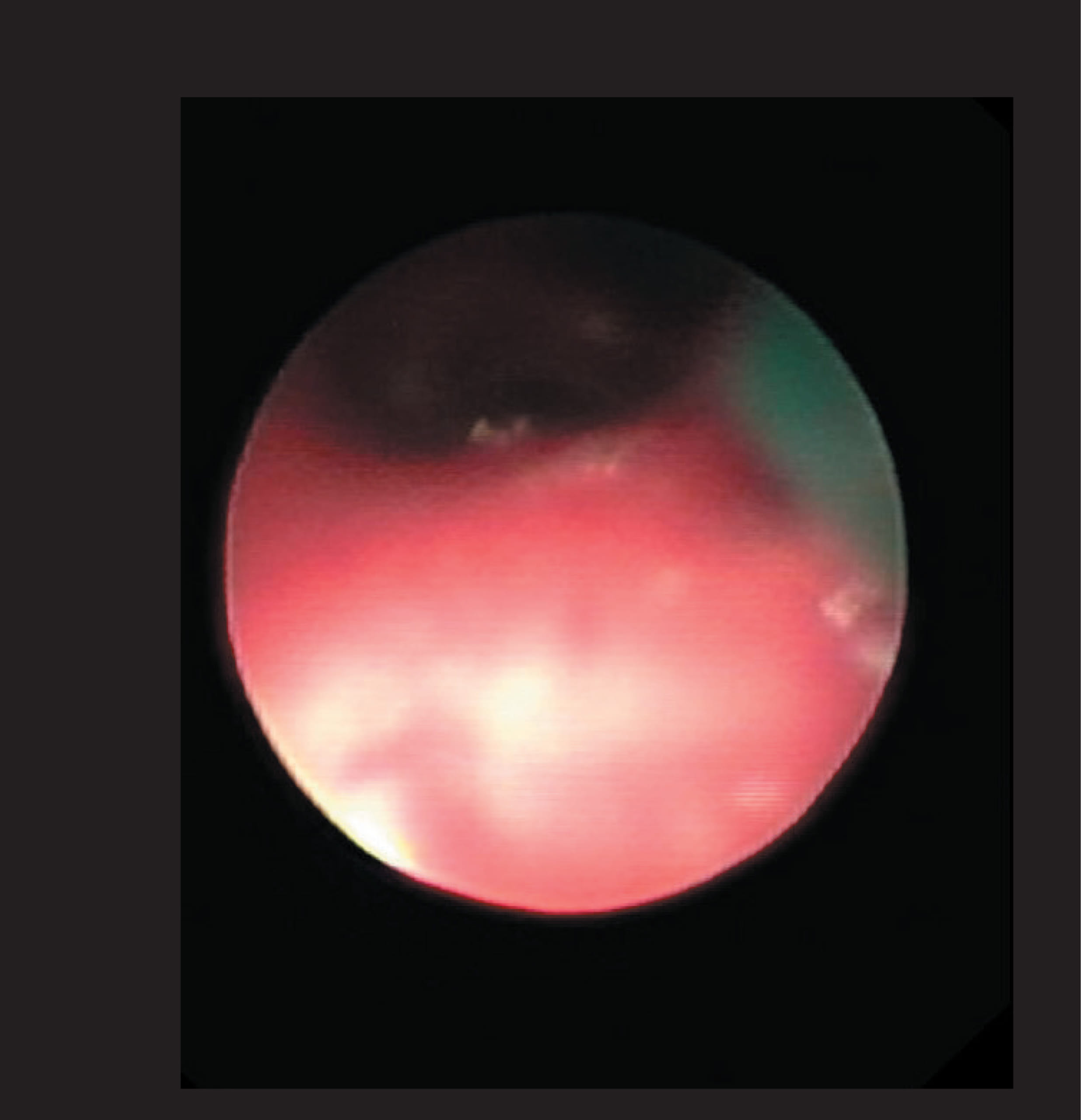
The distal reinforced section of the ViziShot 2 needle, approx. 10cm long, covered with green, plastic sheath, has significantly increased its flexibility, especially of the 21G needle, which allows for easier of its tip up to 70°. Better visible green needle sheath precisely defines the place of biopsy and protects against possible puncture of the biopsy channel. ViziShot 2 needles are sharper, which makes biopsy easier, especially for less experienced bronchoscopists. However, these needles, especially the 22G model, can become bent and dangerously deformed, probably due to the use of a softer steel alloy. The weakest point, especially of the new 22G needle, is that the stylet is too thin in relation to its inner diameter, which often causes a problem in removing the biopsy material from the needle. The new 22G/21G needles, which are more comfortable to use, are also versatile, as they can be used to collect more material in the diagnosis of advanced lung cancer and other mediastinal adenopathies, including sarcoidosis, but also for precise staging of lung cancer. They also show good biopsy reproducibility, as there is usually no clogging of the needle despite several passages.
ViziShot 2 25G
The newest product are thin 25G needles (NA-U401SX-4025N), which have the same mounting system to the bronchoscope as the other needles from the ViziShot 2 family. The transparent sheath refers to the first-generation needles. They are characterized by very good sharpness and slightly weaker visibility in ultrasound imaging. The greatest advantage of these needles is their flexibility and ability to restore the original shape of the needle after each biopsy. The nitinol trocar, although thin and flexible, was very well fitted to the needle channel, allowing repeated biopsies. The amount of material obtained is adequate to the thickness of the needle, allowing for non-bleeded smears. This is particularly important in obtaining diagnostic cytological material even from several biopsied sites, which makes the 25G needle particularly useful in staging, restaging or evaluation of lung cancer recurrence. Our experience also shows the good efficacy of 25G needles in the diagnosis of sarcoidosis, especially when performing cytological smears.
Thanks to the excellent flexibility of the needle, the degree of angulation of the bronchoscope can reach even 90°, thus biopsy of difficult-to-reach nodal stations, e.g. paratracheal, pulmonary ligament (st. 9) or even aorto-pulmonary window (st. 5), as well as tumors of the mediastinal region, tracheal angle or left adrenal gland is easier to perform. Good reproducibility of biopsies also allows collection of material for cytoblocks.
Conclusions
In summary, the ViziShot 2 family of needles is a good continuation of the previous generation. They show a good safety profile and high diagnostic efficacy. Thanks to their diversity, it is possible to choose a specific needle type depending on the clinical indication as well as the preference of the EBUS-TBNA performer.
Authors
Professor Artur Szlubowski, MD, PhD, Independent Endoscopy Unit, John Paul II Specialist Hospital in Cracow, Poland; Endoscopy Unit, Public Specialized Hospital of Lung Diseases in Zakopane, Poland.
Maciej Gnass, MD, PhD, Independent Endoscopy Unit, John Paul II Specialist Hospital in Cracow, Poland; Endoscopy Unit, Public Specialized Hospital of Lung Diseases in Zakopane, Poland.
- Keyword
- Content Type