Robert Staroń, MD, PhD,
Consultant Gastroenterologist
Department of Gastroenterology
and Hepatology with Internal
Disease Unit Clinical Voivodship
Hospital No. 1Rzeszów, Poland

Łukasz Krupa, MD, PhD,
Consultant Gastroenterologist MRCP UK
Department of Gastroenterology and Hepatology with Internal Disease Unit Clinical Voivodship Hospital No. 1Rzeszów, Poland
Introduction
In our center we have been performing interventional (endosonography) EUS procedures since 2015. Among others, we perform approximately 60 EUS-guided drainages of symptomatic fluid collections (walled-off necrosis (WON) or pseudocysts) annually.
Pancreatic Fluid Collections
Pancreatic fluid collections (PFCs) are common complications of acute pancreatitis, and most of them improve with conservative management. Conservative management usually entails antibiotics and nutritional support. Asymptomatic pseudocysts and WON also do not require any intervention as they may resolve on their own. They require drainage if they become symptomatic. Symptoms include infection, abdominal pain, fevers, early satiety, nausea and vomiting. Draining symptomatic collections can be accomplished surgically, percutaneously or endoscopically. The endoscopic approach is minimally invasive and results in lower hospital length of stay and a lower rate of pancreatic fistulae. This approach has become a standard of care in our hospital.
Need for an Appropriate Stent
We have gained practical experience in various types of stents: plastic, bi-flanged FCSEMS (fully covered self-expanding metal stents) and LAMS (lumen-apposing metal stents) including “all-in-one” devices. In Poland, unfortunately the procedure is not adequately reimbursed. “All-in-one” devices with LAMS are very good, safe, simple to use and quick in deployment, but unfortunately the cost of such devices is very high.
Seeking cost-effective solutions without compromising patient care, we implemented a pragmatic approach.
Application of Plumber Stent
For the treatment of simple pseudocysts we use one or two plastic pigtail stents, which is sufficient in most of the cases. In cases of WON or infected pseudocysts we perform drainage using the self-expanding metallic stents FCSEMS HANAROSTENT® Plumber™. In our experience this is a more efficient treatment option for such cases when compared with plastic stents. It is usually possible to determine the content of the collection on the basis of an endosonographic image. To date we have placed 70 of these stents and find them to be a good and safe choice as a treatment option.
The use of the stent requires additional endoscopic accessories such as guidewire and cystotome. Despite that, this is a significantly more cost-effective option compared to an “all-in-one” device, where none of the additional accessories are required. We don’t routinely use an EUS needle or a dilatation balloon for the procedure.
Procedure
The procedure takes approximately 20 minutes and we perform it in the ERCP position. The procedure is done under fluoroscopy and EUS guidance. The pseudocyst or walled-off necrosis is located under endosonographic guidance using a therapeutic linear echoendoscope.
The echoendoscope is placed near the gastric or duodenal wall and cystotomy is performed in two steps with a 5-10 Fr cystotome under EUS/fluoroscopic guidance. If necessary it is possible to inject contrast into the collection through the cystotome.
As a next step we insert a 0.035 Fr guidewire into the cyst through the lumen of the cystotome (EUS and fluoroscopic guidance). The cystotome is removed and the stent is inserted over the wire into the cyst through the therapeutic channel of the scope. During the stent deployment we find it very important to have access to fluoroscopic, endosonographic and endoscopic guidance simultaneously.
The first flange of the stent is opened inside of the cyst or WON under endosonographic and fluoroscopic guidance. During this step, an attempt to obtain endoscopic views in our experience may lead to loss of position. However, should this happen, the advantage of the stent is the option of placing the stent back into the sheath, which allows position change and redeployment of the stent once it is stable.
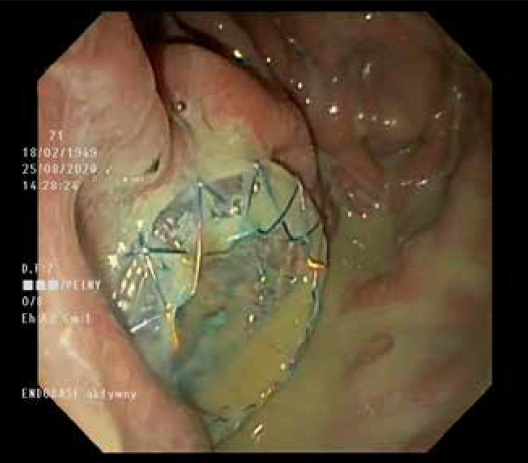
Once we make sure that the first flange is fully opened in the cyst with an EUS/fluoroscopy image, we stop deploying and switch to the endoscopic view. The yellow marker is visualized (Figure 1) and the second flange is opened under endoscopic view. The yellow marker should be kept steady approximately 5 mm from the stomach/ duodenal wall. The delivery device and the guidewire are carefully removed.
Evaluation of Plumber Stent
We find the stent to be a reliable accessory which is user-friendly. It has two round fully covered flanges which maintain the stent position well and hold the two layers together. We did not experience any problems with spontaneous stent migration or dislocation during endoscopic re-interventions such as repeated sessions of necrosectomy. The stent is made of nitinol and fully covered with silicone membrane, hence we do not report problems with tissue overgrowth or ingrowth leading to difficulties with stent removal. It is our practice to remove it after 4-5 weeks, which is easily done using a gastroscope and grasping forceps. This period of time is usually sufficient for the process of cyst emptying. The stent has a lasso on the proximal end which makes the removal easier. The delivery device is easy and clear to use and the markers are well visible endoscopically.
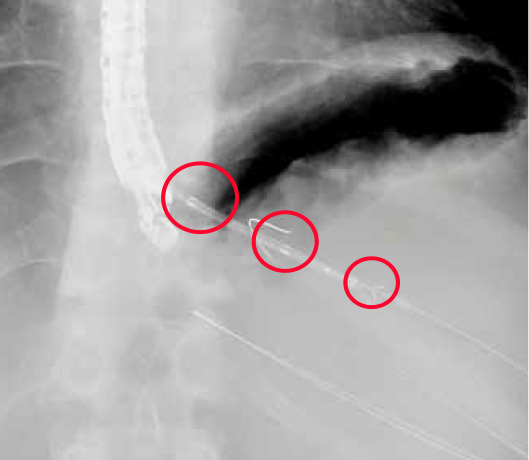
The stent is very well seen under endosonography and fluoroscopic guidance. It has three radiopaque markers at each end and in the middle (Figure 2). This allows precise assessment of the stent position and deployment status before and after the stent deployment (Figure 3). The stent starts opening gradually after being deployed (Figure 4). We do not perform stent dilatation routinely; it usually opens up entirely within 24 hours, which allows gradual and slow emptying of the cyst content. On the second day after the deployment it is possible to pass a gastroscope through the stent into the cyst/ WON if endoscopic debridement or necrosectomy is required.
Complications of Treatment with HANAROSTENT® Plumber™
Every procedure has complications.
During our experience using the stents we had two cases of bleeding. In the first case the bleeding occurred during the procedure and was stopped endoscopically. In the second case the bleeding happened two weeks post-procedure and required surgical intervention and blood transfusion. In three cases we had stent occlusion, which resulted in sepsis and hospital readmission. In all of the cases stent revision using a gastroscope was performed. The stents were unblocked and the patients recovered.
Conclusion
In summary HANAROSTENT® Plumber™ is an important endoscopic accessory for the endoscopic management of symptomatic pancreatic fluid collections. The device is intuitive and reliable. It is clearly seen throughout the entire deployment process in three modalities: endoscopic, fluoroscopic and endosonographic.
As medical knowledge is constantly growing, technical modifications or changes of the product design, product specifications, accessories and service offerings may be required.
- Keyword
- Content Type