Introduction
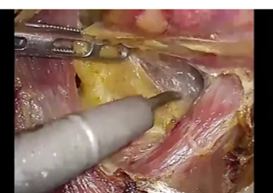
Since 1997, laparoscopic distal gastrectomy with D2 lymph node dissection, which has been around for a number of decades, has been considered the standard for treating gastric cancer. Dissection, performed with dissection forceps, occurs between the tissues and principal vessels and the pancreas, and after a space is created for insertion of the ultrasonic coagulating shears, lymph node dissection is accomplished by repeated coagulation and incision. The procedure is complex and a major reason for the long operation time.
THUNDERBEAT represents a recent technological advancement. The instrument has a blade that is ideally shaped for dissection; thus, the tissue dissection can now be performed without the use of dissecting forceps. In addition, THUNDERBEAT is capable of simultaneous output of bipolar energy and ultrasonic energy, thereby providing both precise hemostasis and extremely rapid tissue dissection. The planned lymph node dissection can be accomplished precisely, safely, and quickly.
Described herein is laparoscopic treatment of a gastric cancer for which distal gastrectomy with D2 lymphadenectomy is indicated. An overview is given along with intraoperative photographs of an actual procedure.
Instruments used




Forceps



Water supply/aspiration tube

Trocar



Clip

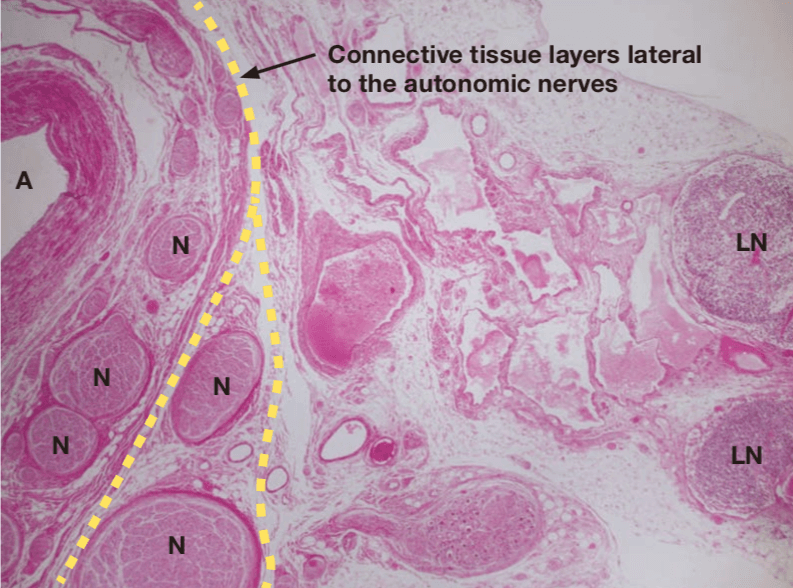
The concept of lymph node dissection
Autonomic nerves run along the arteries, and the lymphatic structures requiring dissection lie lateral to these arteries and nerves. Layers of connective tissue lie between the lymphatic structures and the arteries and nerves, and these layers can be separated. During standard preventive dissection, there should be sufficient dissection of the layer that houses the neural tissues if it is determined that this measure is required.
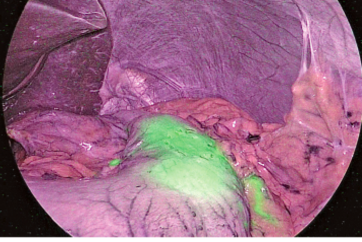
The connective tissue layer can be stretched by appropriate countertraction, and during laparoscopic surgery in particular, it can be recognized by its bubble wrap appearance, which results from gas from the abdominal insufflation naturally entering the space.
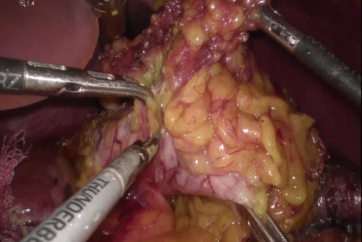
Lymph node dissection along the superior pancreatic margin
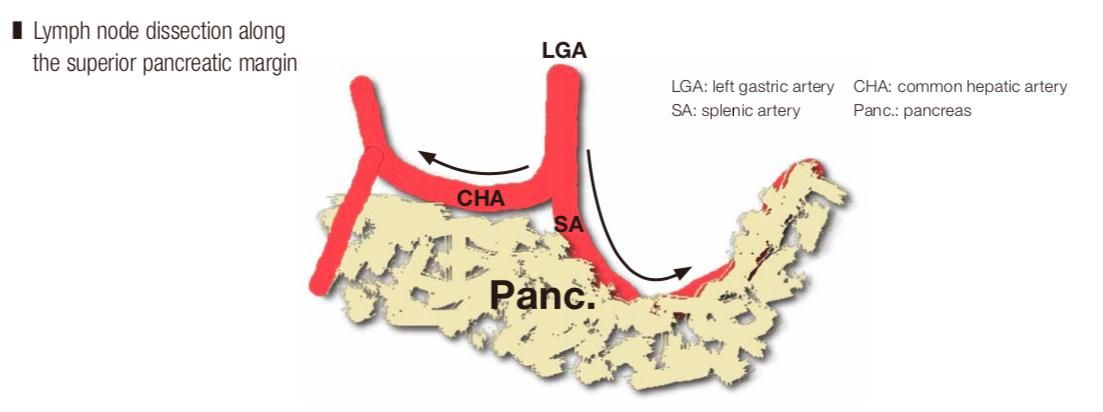
The densest and thickest neural tissues are located at the root and close to the middle of the trunk of these arteries; therefore, it is easy to confirm the artery roots during dissection of the aforementioned layers. At the superior margin of the pancreas, one can enter coarse connective tissue layers lateral to the nerves on the left and right sides of the left gastric artery. Thereafter, the layers are separated in a U-shape along the neural plexus around the hepatic artery on the patient’s right side and in a V-shape that encloses the lymphatic structures in the layer between the anterior surface of the celiac ganglion and the posterior surface of the pancreas on the patient’s left side (UV cut). Finally, the No. 8 and No. 11p lymph nodes, which are connected to the paraaortic lymph nodes, are mobilized, and after as much traction as possible is applied for the purpose of elevation, dissection is advanced as deeply as possible, and paraceliac lymph node dissection is completed.
Dissection of No. 6 lymph nodes
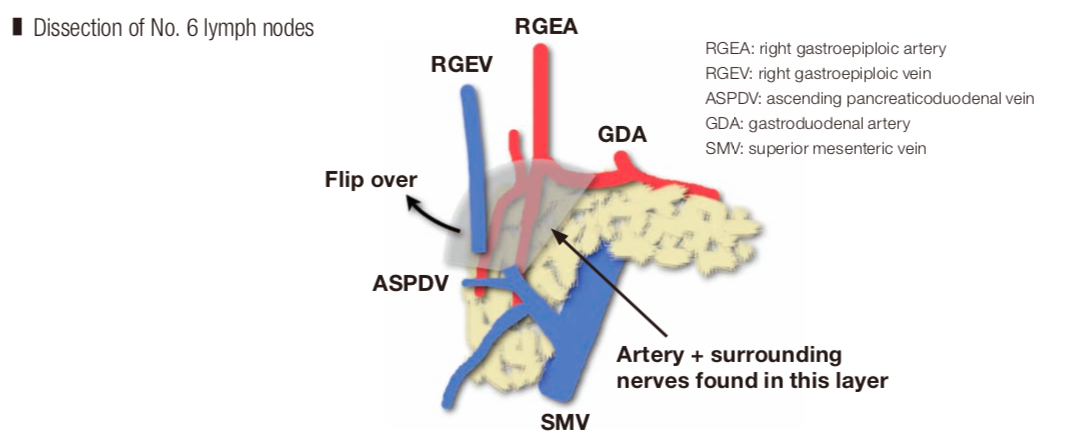
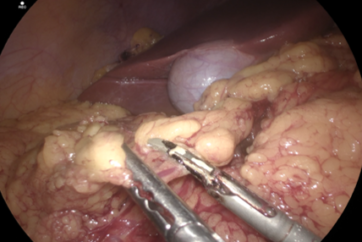
Dissection of the No. 6 lymph nodes means we must consider how to approach the anterior surface of the pancreas. This has become feasible in recent years. A layer of nerves lateral to the artery is present on the anterior surface of the head of the pancreas, and the nerves form a network on the anterior surface of the pancreatic parenchyma. Dissection is also performed along this layer. The lymphatic structures are covered by a protective membrane, making en bloc resection possible, avoiding injury.
*Taken from Laparoscopic D2 gastrectomy using THUNDERBEAT.
Compiled under the supervision of Dr. Seiichiro Kanaya, Department of Gastrointestinal Surgery, Osaka Red Cross Hospital
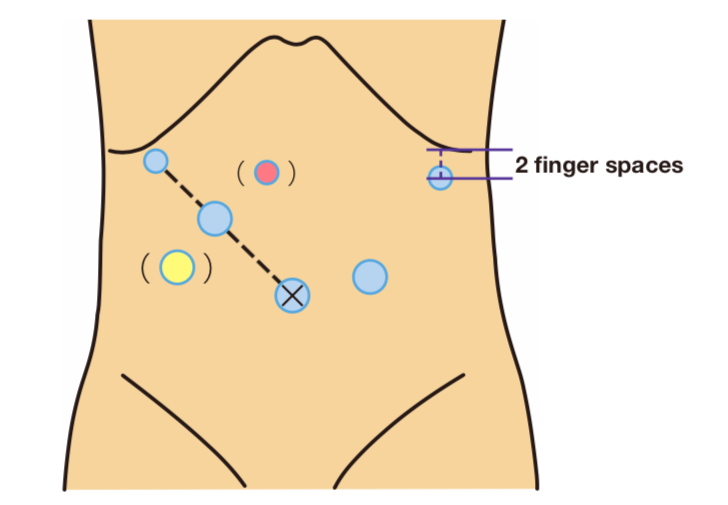
Positioning the patient and the trocars
The patient is placed in the lithotomy-Trendelenburg position with the right arm along the right side. The surgeon stands on the patient’s right side, the assistant stands on the patient’s left side and the camera operator stands between the patient’s legs. However, the surgeon and assistant switch places during inferior pyloric lymph node dissection. The camera trocar is inserted into a longitudinal incision made in the lower half of the umbilicus. However, if the patient has a very small body and the distance from the xiphoid process to the umbilicus is very short, insertion is sometimes performed below the umbilicus. The surgeon inserts a trocar at the highest point of the diaphragmatic dome directly below the liver and uses the left-side trocar (5 mm) to perform laparoscopic examination from below the right costal arch. In some cases, the trocar is inserted directly above the floor of the gallbladder. If the trocar follows a dorsal path, when the No. 11p lymph nodes are dissected, caution is required because it is difficult to grasp the lymphatic tissue and apply traction. The surgeon holds trocars (12 mm) in the right hand and inserts them at a distance of four finger spaces or more between them along the line connecting the trocar to the camera, which is being used with the left hand. If sufficient distance cannot be obtained, insertion is sometimes performed somewhat caudally (● ). If the right-hand trocar is inserted too far caudally, it may not be possible to secure a sufficient angle between THUNDERBEAT and the superior pancreatic margin during dissection of the No. 11p lymph nodes, and at such times, a single port with a 5-mm trocar should be added cranially (●). The assistant places the right hand below the costal arch at the anterior axillary line. Previously, insertion was performed directly below the costal arch, but insertion of the trocar two fingers caudally during dissection of the No. 6 lymph nodes establishes the correct angle between THUNDERBEAT and the anterior surface of the head of the pancreas, and ultimately, the trocar is inserted somewhat caudally. The assistant, using the left hand, inserts the trocar (12 mm) above the site of stapler insertion, somewhat caudal to the midclavicular line.
- Keyword
- Content Type