Special Maneuvers
In this chapter we describe special maneuvers that have proved helpful in the past. We recommend that you retain them in your endoscopy armamentarium in order to deal with situations demanding special tricks.
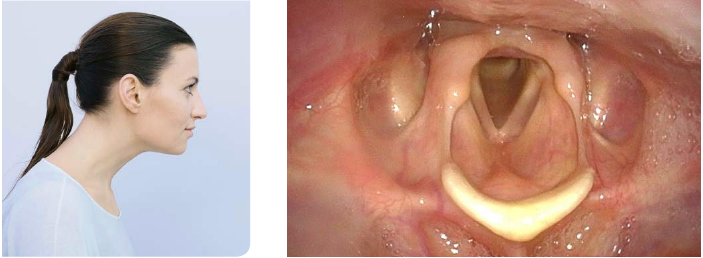
Problem: Suspected Hypomobility
Solution:
- Use flexible laryngoscopy for testing the respiratory mobility of the arytenoids and the vocal folds.
- Video documentation with frame-per-frame off-line analysis is highly recommended.
- Perform various maneuvers:
- Repeated phonation of “eee”, quickly and slowly, in staccato mode
- Repeated sniffing with sharp inspiratory nasal sniffs
- Repeated “eee”-sniff (diadochokinesis) maneuvers
- Throat-clearing and coughing
- Laughing
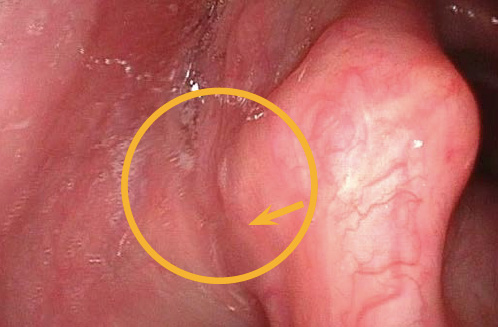
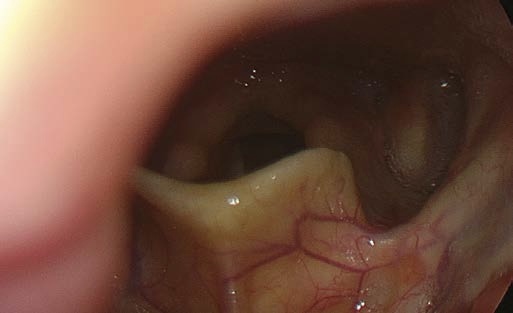
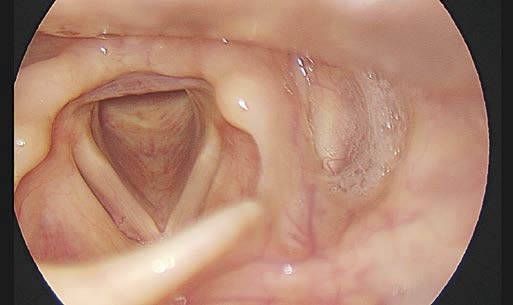
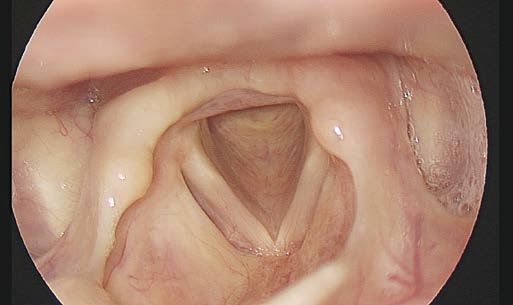
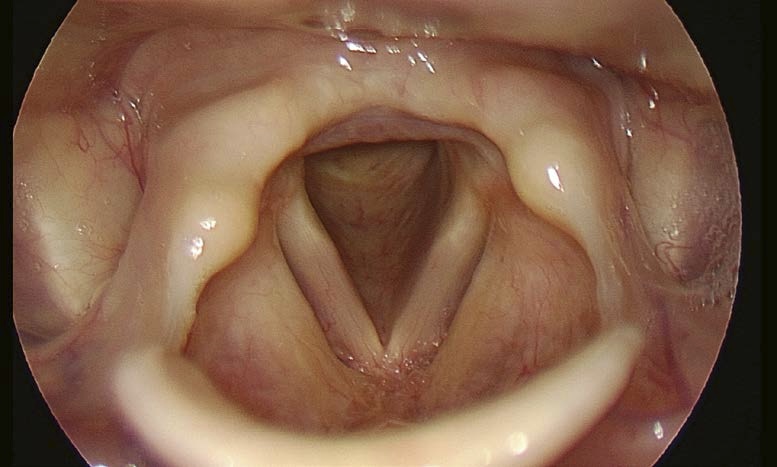
- Look for the active lateralization of muscular process during vigorous abductory maneuver, e.g. forceful sniffing (A, B)
- Nota bene: The original definition of the “jostle sign” refers to a passive motion of the arytenoid by the other arytenoid. In our procedure of forceful sniffing, look for the active movement of the muscular process by activation of the posterior cricoarytenoid muscle. Sometimes it looks like a knee kicking under a blanket.

Note:
Respiratory mobility of the arytenoids and vocal folds should always be tested thoroughly and with several maneuvers.
Problem: Close-Up View of Vocal Folds Needed (Flexible Endoscopy)
Because of small morphologic changes of the vocal fold you want to get a very close-up view of the vocal folds.

Solution:
- To get a very close-up view of the vocal folds or of the subglottis / trachea during flexible endoscopy perform the dipping maneuver with a long lasting inspiration through the nose

Problem: Size of Reinke’s Edema Unclear
- On occasion, localized Reinke’s edema or pedunculated lesions at the free edge of the vocal fold are found on the superior surface of the vocal fold and will not be detectable in shallow respiration.

Solution:
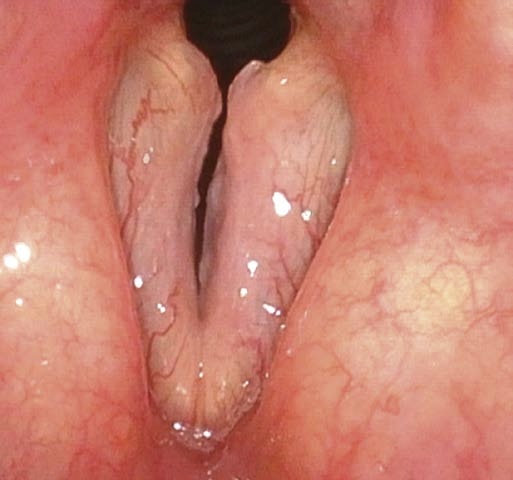
- Whether using rigid or flexible endoscopy, try asking the patient to perform a forced, rapid inspiration. This leads to suction of the medial part of the vocal folds into the glottis and thus the edema or pedunculated lesions at the free edge will become “aerodynamically medialized” and detectable.
- Forced and rapid inspiration (see also inspiratory phonation) may also help to clear mucus from the free edge of the vocal fold while avoiding the throat-clearing with associated blurring of the lens.

Problem: Ventricular Folds Covering Vocal Folds or Pliability and Free Edge of Vocal Fold Unclear
(1) The vocal folds cannot be seen during phonation because they are concealed by the ventricular folds.
or
(2) You need a general impression about the mucosal pliability at the free vocal fold edge.
or
(3) You want to rule out additional masses on the superior surface of the vocal folds.
Solution:
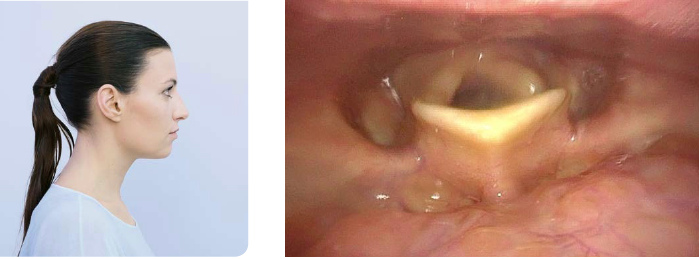
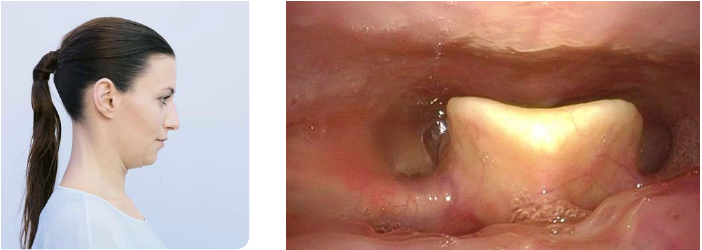
During inspiratory phonation (both in rigid and flexible laryngoscopy), the following phenomena can be seen:
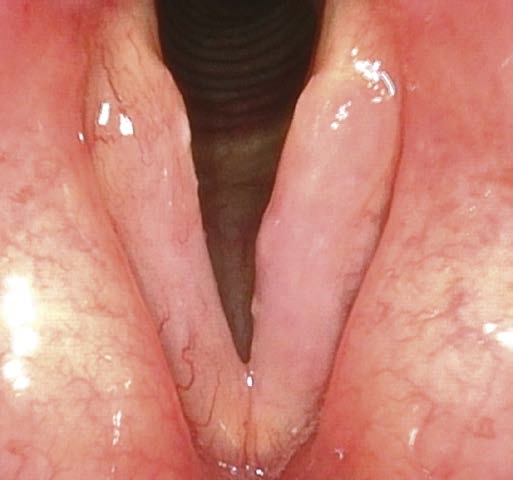
(1) Inspiratory phonation adducts the vocal folds and abducts ventricular folds. With the ventricular folds moving laterally, the entire superior vocal fold surface and parts of the ventricle can be seen.
(2) The free edge of the vocal folds is sucked into the glottis and shows where the mucosa of the free edge is normally pliable.
(3) Reinke’s edema or other mass lesions on the superior surface of the vocal folds can be detected.
Note:
Forced and rapid inspiration and inspiratory phonation should always be part of the examination of benign mass lesions located on the vocal folds.
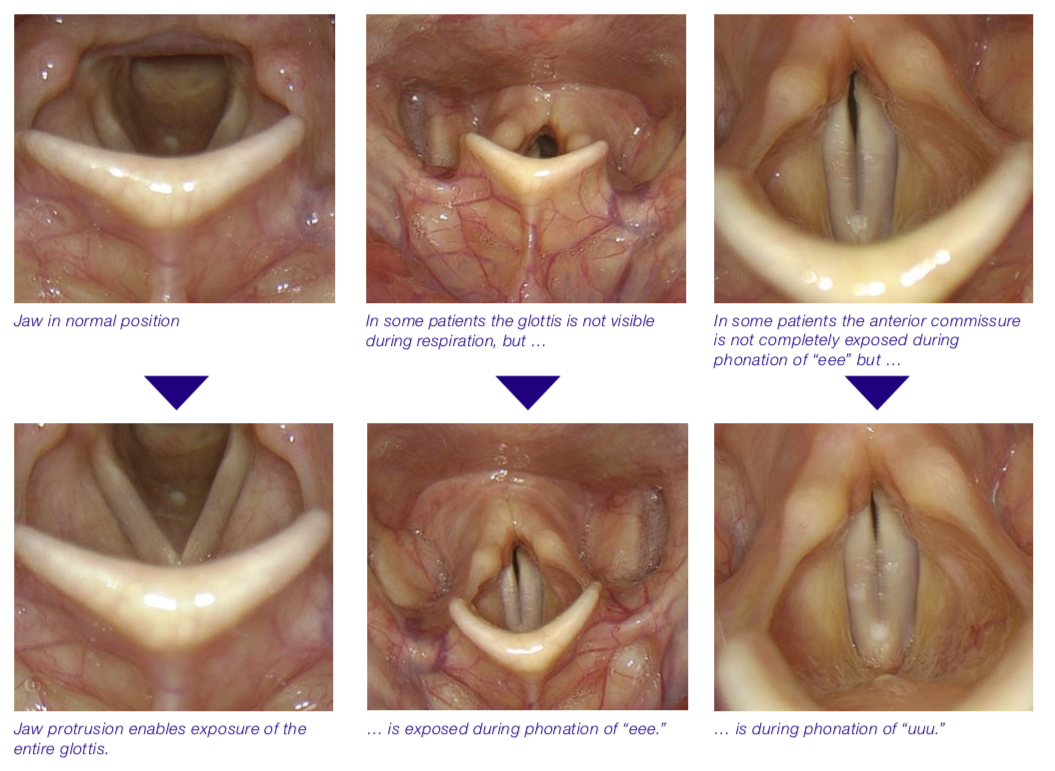
Problem: Ventricular Folds Covering Vocal Folds (See Above)
Ventricular folds are in a hyperadducted position and therefore cover the vocal folds.
Solution:
- When the ventricular folds are covering the vocal folds during phonation, change from “eee” to “uuu” (especially in rigid laryngoscopy).
- Phonation of “eee” usually pulls the tongue base and epiglottis forward. Phonation of “uuu” additionally leads to abduction of the ventricular folds. The ventricular folds will move more laterally, the epiglottis sits slightly more upright, and the vocal folds can be seen. Even with rigid endoscopy “uuu” is possible. Make sure that your patient really tries hard to phonate “uuu”.
- Inspiratory phonation also adducts the true vocal folds and abducts false vocal folds (see above).
Problem: SLN Function Unknown or Free-Edge Problem
(1) You need detailed information about the superior branch of the recurrent superior laryngeal nerve function.
or
(2) You are not sure whether the margin of the vocal fold is smooth and straight.
Solution:
- Falsetto phonation (both rigid and flexible laryngoscopy) leads to lengthening of vocal folds and gives information about CT muscle and superior laryngeal nerve function.
- If very small epithelial lesions of the free margin exist, they will show as contour irregularity (particularly, when using stroboscopy).


Note:
Falsetto phonation should always be part of the examination of benign mass lesions of the vocal folds.
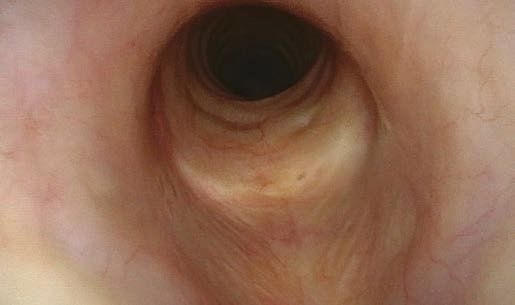
Problem: Need to Inspect the Trachea
Suspected changes in the trachea (flexible endoscopy)
Solution:
Chin-tuck maneuver, combined with dipping maneuver

Problem: Need to Inspect Piriform Sinus and Postcricoid Region
You should inspect the piriform sinus and postcricoid region
Solution:
Ask the patient to perform a Valsalva maneuver (trumpet maneuver) while the endoscope is in place and the nostrils and mouth are completely closed.


Problem: The Epiglottis Is Covering the Vocal Folds
You cannot see the vocal folds because the epiglottis is covering them.
Solution:
- Adjust the patient’s head and neck position to obtain a better view of the glottis (applies to rigid laryngoscopy).
- Ask the patient to actively cause the mandible to protrude.
- Phonation of “uuu” instead of “eee” (see above).

Special Positioning of Endoscope or Patient
Sometimes specific laryngeal structures – mostly the vocal folds – cannot be seen with the normal position of the patient and the normal position of the endoscope. Especially in rigid endoscopy, changes of the position of the patient or the examiner or special maneuvers with the tip of the endoscope may help to achieve a better visualization of the vocal folds.
Below you will find some examples of insufficient exposure of the glottis.
Problem: The Uvula Disturbs
The uvula may intrude and disturb adequate illumination during rigid endoscopy.
When the endoscope lens is placed very close to a surface, the image will show a local washed-out whitish patch due to the camera’s averaging light management software.

Solution:
When “fighting” with the uvula, try dropping the endoscope tip and advancing it a bit more inferiorly.

Problem: No Sufficient Exposure of the Larynx in Rigid Endoscopy
Here we show examples of suboptimal positions for the endoscope tip.


Solution:
Improvement of positioning the rigid endoscope tip.
See intraoral position of tip of rigid endoscope (see description above).
Problem: The Epiglottis Disturbs
The epiglottis may cover the glottic area while performing flexible endoscopy.
Solution:
- Advance flexible endoscope until it passes the level of the epiglottic rim.
- Phonation of “uuu” will shift the epiglottis into a more upright, vertical and anterior position.
- Ask patient to change the position of their head to sniffing position with cervical spine and jaw moved forwards (see below: Change of patient’s head position)


Problem: Need to Visualize Medial Surface of Vocal Fold
The medial surface of the vocal fold cannot be visualized on flexible endoscopy.
Solution:
- Which nasal cavity is being used for the transnasal endoscopy? Try changing sides – right or left
- When deciding which nasal cavity side is most suitable for passing the flexible endoscope, consideration should be given not only to the size of the nasal cavities but also to the question of which vocal fold is of special interest. Select the right nasal cavity when you want a really good view of the left vocal fold and vice versa.


Rigid Endoscopy – General Aspects of Positioning
The position of the tip of the endoscope depends on patient’s and examiner’s posture.
The position of the endoscope can be changed by different postures of the patient.
Note the change of angle between endoscope and neck with different postures.
For maximal anterior and posterior laryngeal exposures the positions of patient and examiner have to be changed accordingly.
Elbows-on-Knees Position – 90° Rigid Endoscope
The 90° endoscope is typically held horizontally.



Elbows-on-Knees Position – 70° Rigid Endoscope
The 70° endoscope is typically held steeper than the 90° endoscope.



Positioning of Patient and Examiner in Rigid Laryngoscopy
Problem: Need to Visualize the Anterior Commissure or the Laryngeal Surface of the Epiglottis
Anterior commissure not visible


Solution:
Position according to Türck:
- Patient sitting, examiner standing
- Good for better view of anterior commissure
- Use this position for the examination of the laryngeal surface of the epiglottis, too.


Patient sitting, examiner standing (or sitting): In rigid endoscopy, the anterior commissure and the petiole can be visualized (position according to Türck).
Problem: Suspected Posterior Glottic Stenosis (PGS)
Posterior larynx not visible
Solution:
Position according to Killian:
– Patient standing, examiner sitting
– Good for better view of posterior larynx
– Use this position for ruling out posterior glottic stenosis (PGS) and scarring







Note:
In flexible endoscopy these structures can be seen more easily – but only when the tip of the endoscope is close enough!
Problem: Needing a Close-Up View of Vocal Folds or Anterior Commissure
How to obtain good quality close-up images of the glottis and anterior commissure using rigid endoscopy


Solution:
- Position the tip of the rigid endoscope just above the laryngeal inlet.
- Placing the distal shaft of the endoscope on the tongue base and pressing it downwards enables you to get a closer view of the glottis.
- This works particularly well when using the 70° endoscope, with which you can obtain a very close view of the glottis and (sometimes) a close view of the anterior commissure.
- Try the elbows-on-knees position



Problem: Need to Inspect Morgagni’s Ventricle
How best to inspect Morgagni’s ventricle (rigid endoscopy)
Solution:
- Select a 70° rigid endoscope and have the patient sit in the elbows-on-knees position.
- Anesthetize the pharynx and larynx thoroughly.
- Dip the tip of the endoscope into the larynx by pressing the shaft onto the tongue base, advance it into the supraglottis and then rotate the tip towards the ROI.

Problem: Need to Inspect the Piriform Sinus
How best to inspect the piriform sinus (rigid endoscopy)
Solution:
You can change the axis of laryngeal visualization by employing different oropharyngeal positions for the endoscope in addition to simply rotating its tip.






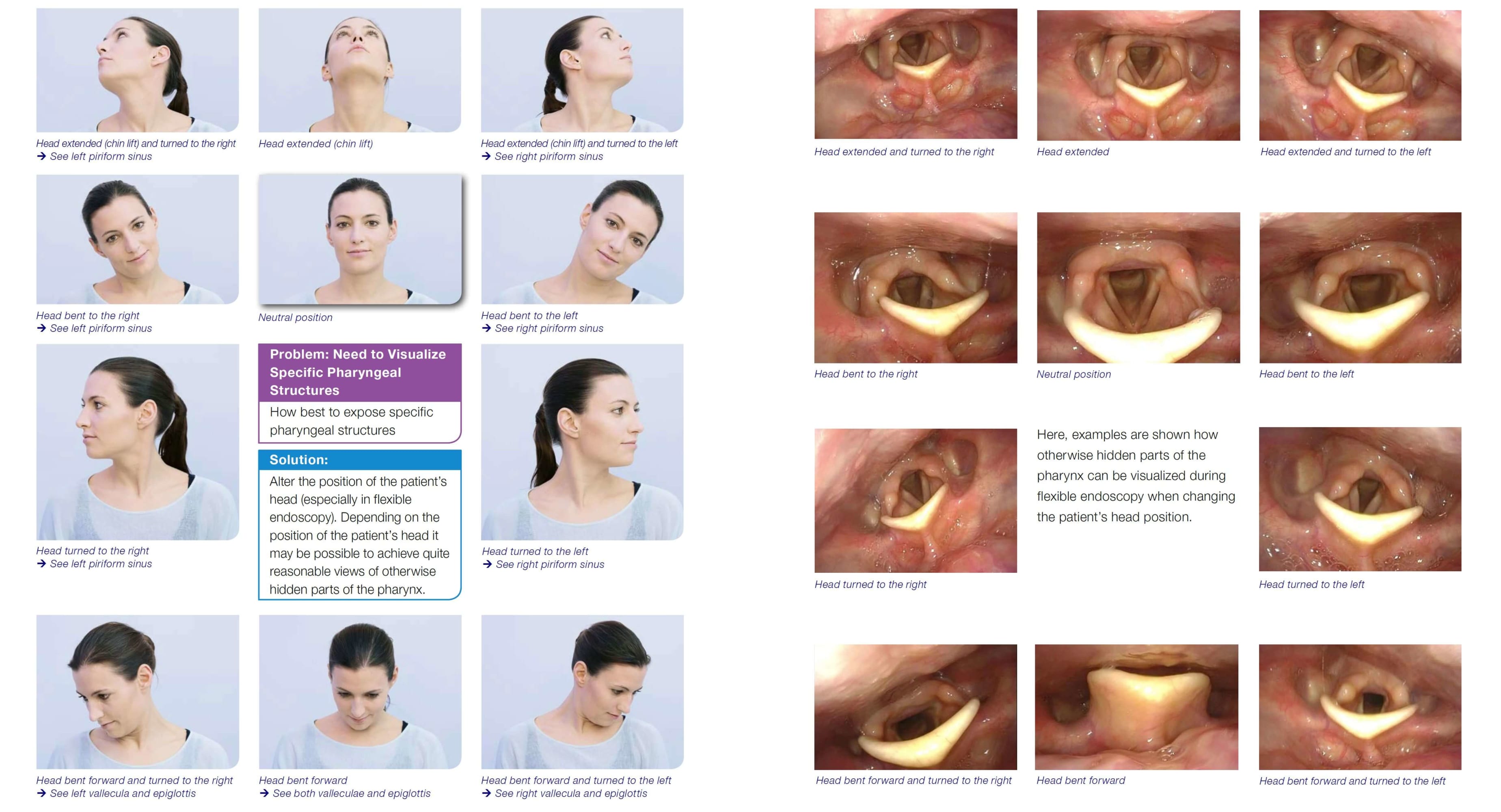
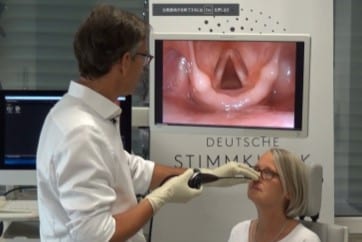
Change of the patient’s head position






Problem: Need to Visualize Specific Pharyngeal Structures
How best to expose specific pharyngeal structures
Solution:
Alter the position of the patient’s head (especially in flexible endoscopy). Depending on the position of the patient’s head it may be possible to achieve quite reasonable views of otherwise hidden parts of the pharynx.





Here, examples are shown how otherwise hidden parts of the pharynx can be visualized during flexible endoscopy when changing the patient’s head position.











- Content Type