Special Maneuvers for Flexible Endoscopy
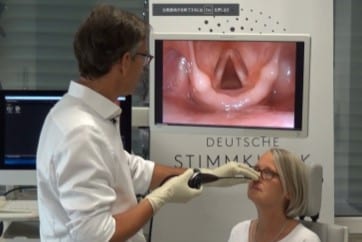
Endolaryngeal Dipping Maneuver
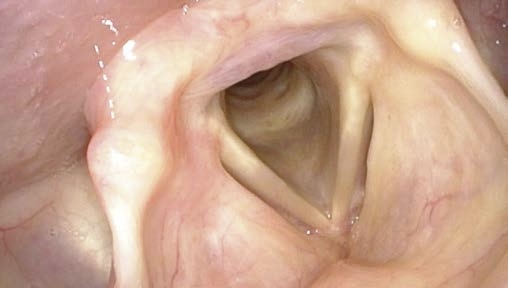
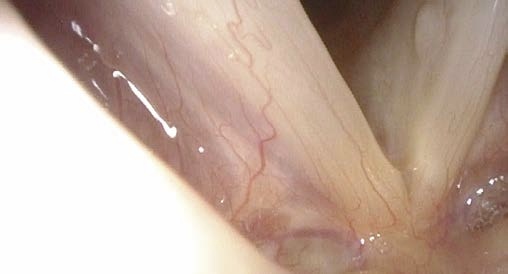
Fine structures of the vocal folds can be evaluated best when the tip of the endoscope is advanced very close to the intralaryngeal target, almost touching the vocal folds.
To avoid triggering gagging and cough reflexes, be careful not to touch any laryngeal structures.
Experience shows that this close-up maneuver is most easily performed during long nasal inspiration.
We recommend that the patient practices the breathing maneuvers prior to performing the so-called dipping maneuver.
With this practice run, the patient learns to tolerate the endoscope and the endoscopist becomes acquainted with the patient’s individual reactions.
In order to achieve a longer inspiratory phase it can be helpful to increase the inspiratory resistance by closing the nasal alar not being examined with an endoscope using a finger of your distal hand.
Alternatively, the patient can help by closing the unoccupied nasal ala himself / herself.
Sometimes it is advisable to change the light source setting from automatic gain control (AGC) to manual gain control, or to use blue stroboscopy light to avoid overmodulation / “washout” under zoom conditions.
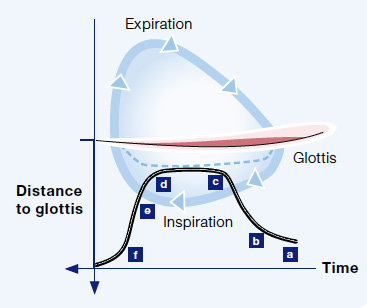
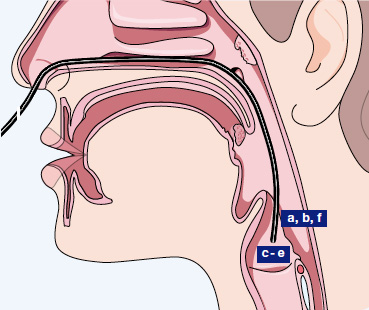
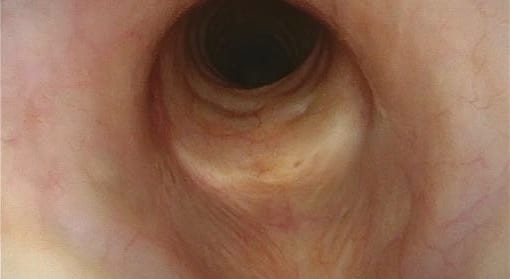
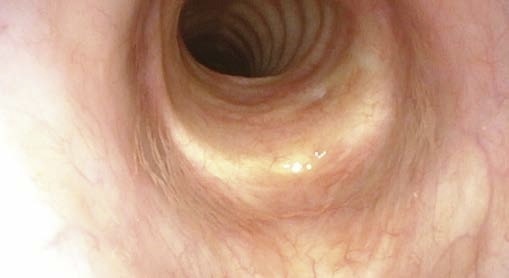
a Supralaryngeal
b Begin of diving
c Close to vocal fold
d Close to vocal fold
e Begin of withdrawing the endoscope
f Supralaryngeal
Nasal inspiration is now intentionally prolonged due to the small lumen and high nasal airway resistance.





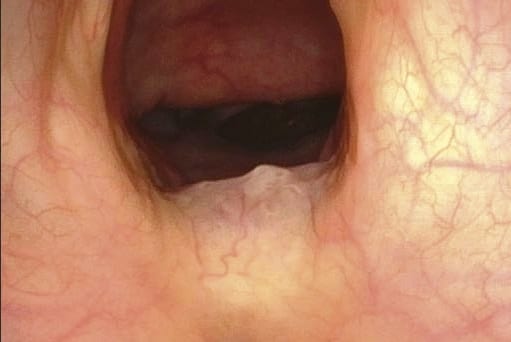
Transstomal Flexible Endoscopy of Subglottis and Trachea
In patients with tracheostoma, transstomal flexible endoscopy is performed to visualize the trachea as well as the subglottis and glottis from an inferior approach.
The lower trachea can be examined with or without cannula.
Cannula-induced erosions, lacerations or ulcers of the tracheal mucosa are best seen without cannula, with the endoscope inside the cannula while pulling the cannula out simultaneously with the endoscope, or while reinserting it.
For visualizing the subglottis and glottis, the tip of the endoscope has to be angled at approx. 90° upwards or more because of the tracheal-laryngeal curvature.
Stabilize your distal hand next to the tracheostoma, avoid sudden movements, and avoid touching the trachea with the endoscope.
Be prepared for the patient to cough! Ask the patient to shield the stoma with a gauze square.
Do not insert a flexible endoscope through a speaking valve. The endoscope tip might be damaged when pulled out.







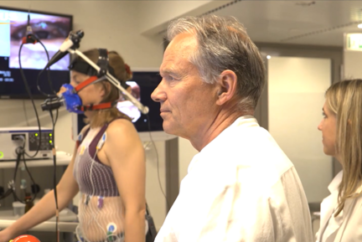
Transnasal Flexible Endoscopic Examination of Swallowing (FEES)
The oropharyngoesophageal swallowing assessment is a complex procedure. Here we can only address a few aspects.
FEES stands for fiberendoscopic examination of swallowing.
Prior to any examination of swallowing, take the patient’s history: Which problems occur while swallowing and what consistency of food / fluids does the patient feel is easiest to swallow? Which is the most problematic?
Try the easier consistencies first.
Evaluate the morphology and mobility of laryngeal and pharyngeal structures using normal flexible endoscopy prior to starting the FEES.
Assess voice and test voluntary coughing before and after examination of swallowing.
The patient should sit upright (as upright as possible even when FEES is being performed at the bedside).

Preparation for FEES
Water coloration
- Green or blue food colorant provide the best contrast
- Use enough color dye to ensure vivid contrast of the mixture
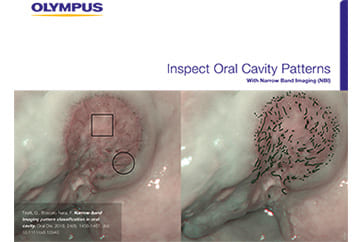
- Special tip: use green colorant and NBI for High Sensitivity FEES
- Protect the patient’s clothes
- Also take care not to stain your own clothes and your fingers Thickening of water:
- Decide which consistency you want to test
- Sometimes it makes sense to test with biscuit or other crumbly foodstuffs Use a straw, spoon, or special feeding cup

Look For
- Intraoral control of bolus
- Drooling
- Leakage
- Retention
- Pooling
- Laryngeal penetration
- Aspiration
- Silent aspiration
- Pre-, intra-, and postdeglutitive aspiration
- Regurgitation






Transnasal Flexible Esophagoscopy (TNE)
After performing flexible pharyngolaryngoscopy, it is possible to additionally perform a transnasal esophagoscopy of the upper esophagus to get an impression of its morphology and function.
From our experience, anesthetization of the pharynx is not necessary.
TNE can be most easily performed when the patient (while holding a deep breath) keeps on swallowing while the endoscope advances. It is recommended to ask the patient to drink a glass of water with a straw.
Advance the endoscope actively towards the postcricoid region. Do not push the flexible endoscope into the esophagus, let it be pulled down while the patient is in the act of swallowing.
Take advantage of the fact that during the pharyngoesophageal phase of swallowing, the larynx is elevated and the upper esophageal sphincter opens. Within a split second, the sphincter closes while the larynx is still elevated. Thus, the sphincter grabs the endoscope tip and pulls it downwards when the larynx descends again.
As an alternative, you can position the tip of the endoscope in the piriform sinus and let the patient swallow.
The advancement of the endoscope from the pharynx to esophagus is very similar to the insertion of a nasogastral feeding tube.
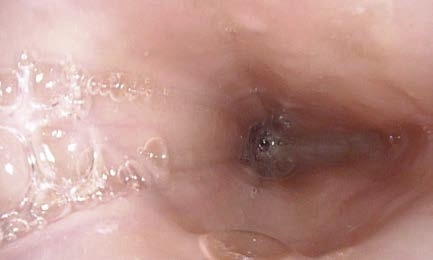
While the patient is repeatedly swallowing, visualization of the upper sphincter is not possible because of bubbling bolus and secretions.
The inner esophagus is physiologically open, i.e. a lumen can be seen continuously. It is filled with air and aerosols are usually seen as tiny floating particles.
Peristaltic movements are very slow and can be seen as superior-to-inferior constricting motions.



TNE: How to Instruct Your Patient
Sequence of Endoscope Handling Movements and Instructions for the Patient:
- “Breathe in and then hold your breath”
→ Thus the patient is prepared for a series of swallowing exercises - “Try to swallow 10 sips of water in a rapid sequence”
→ During swallowing, guide the endoscope above the esophageal opening / the postcricoid region. The upper esophageal sphincter “catches” the endoscope and pulls it inwards, thus it is pulled into the esophagus. You will suddenly see a lumen filled with bubbly fluids. - “Breathe again and do not swallow”
→ After the bolus is transported caudally, the widened lumen is clearly visible until the next swallow sets in. - “Swallow again”
→ After peristaltic constriction during swallowing, the esophagus widens again and downstream peristaltic movements can be seen.
→ If you want, you can now inspect the lumen with NBI illumination.
→ Slowly pull back the endoscope and observe the mucosa.
After passing the postcricoid region you will end up in the hypopharynx.

- Content Type