Related information

Tips on reducing artifacts
If you want to minimize artifacts in ultrasound imaging, you need to understand the characteristics of ultrasound waves. When the ultrasound wave enters an object perpendicularly, a clear image with a high S/N ratio can be obtained. The focal length of each transducer has been set to deliver this image with the highest-possible resolution. Generally, the optimal focal length of an ultrasound scope’s transducer is 2 to 3 cm. Another property of ultrasound wave is that the higher the frequency, the more detailed the image. However, higher frequencies are accompanied by greater attenuation (making it hard to visualize objects that are further away). Low frequency waves, on the other hand, can penetrate deeper, but the image will be grainier.
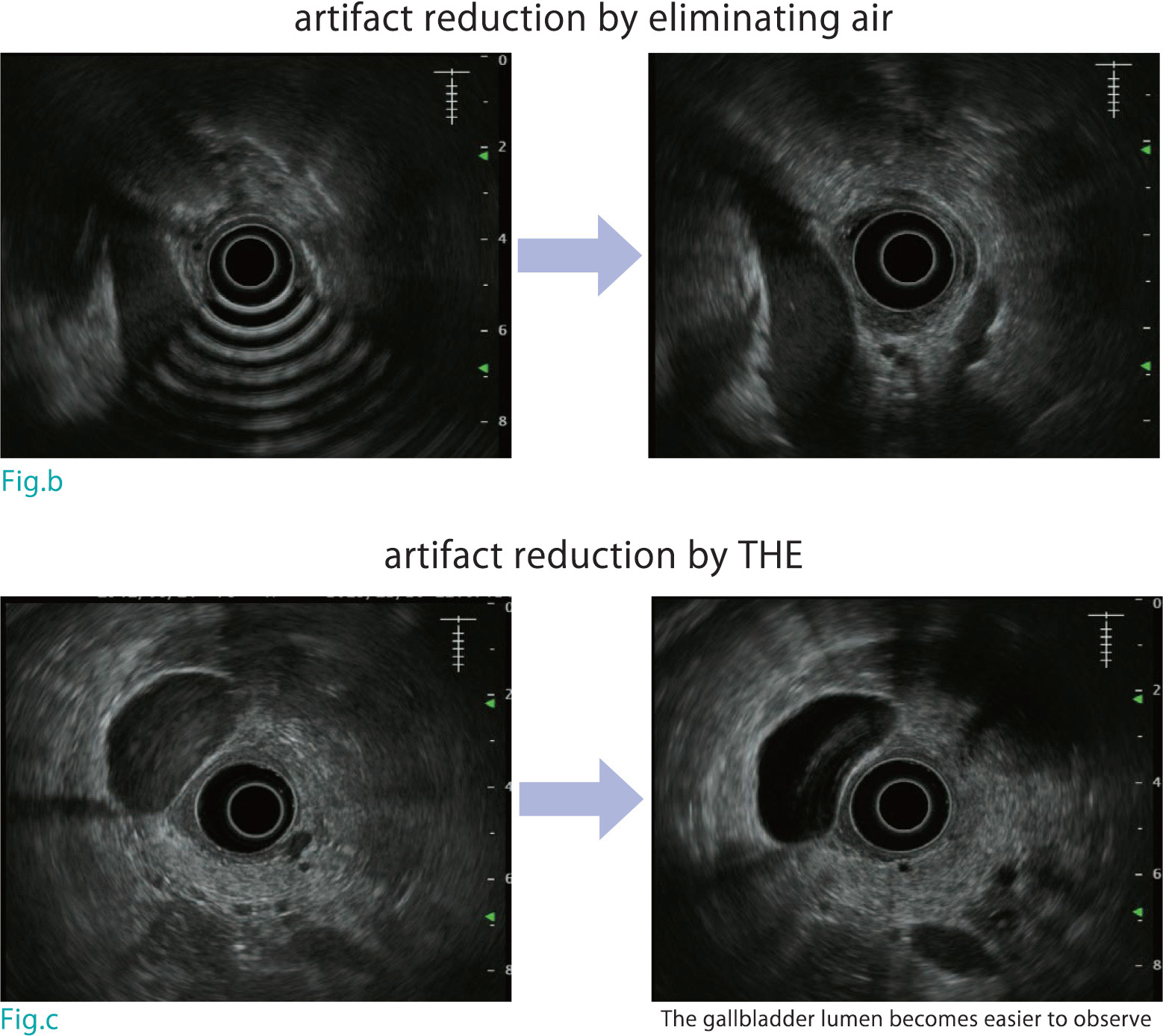
The first, and most common, type of artifact is caused by air and is generated when the ultrasound wave is reflected on the boundary surface between air and water. Getting rid of this type of artifact is a perennial challenge for EUS operators. Insert the scope until it reaches the intended position while trying to insufflate the lumen as little as possible. However getting past the pylorus without insufflation can be difficult, To ‘It all depends on finding the right balance. Insufflate a little and advance the scope; then pull the scope slightly while ensuring that the distal end of the transducer remains in the duodenal bulb. When the objective lens is back in the antrum, suction the stomach (Fig. a). Alternatively, advance the scope as far as the IDA in the “short-scope” position; then suction air or instill lukewarm water to displace the air. In other words, to reduce artifacts, you’ve got to get rid of the air (Fig. b). If, after trying these techniques, you still have a problem with air artifacts, you can eliminate air between the transducer and target site by inflating the balloon and changing the patient position.
The second type of artifact is produced when the ultrasound wave is reflected by the wall of the lumen (grating lobe artifact). This may make it difficult to observe cystic and tubular structures. To reduce this artifact, tissue harmonic echo (THE) is effective (see chapter Functions) (Fig. c).
The third type of artifact (multiple echo) is caused by reverberation of ultrasound waves between the transducer and balloon. Since this artifact cannot be reduced by THE, it is a good idea to change the size of the balloon if the artifact is making it difficult to observe the lesion.

Pros and cons of radial EUS
Radial EUS and convex EUS are often compared. But both have pros and cons.
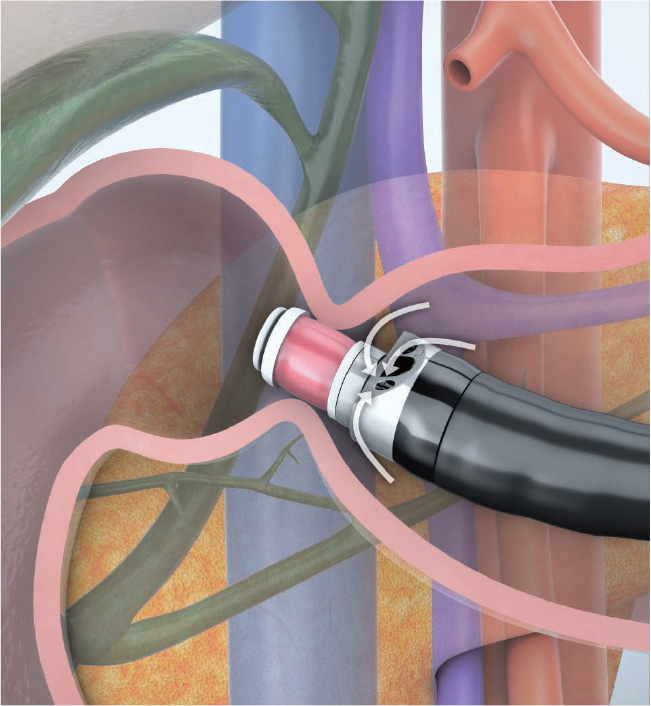
Radial EUS is distinguished by its capability to deliver 360-degree ultrasound images with respect to the scope axis. This makes it possible to scan across a wide range of regions, including the bile duct and the pancreas outside the gastrointestinal tract, without too much scope maneuvering. It is often better to use radial EUS when scanning the gallbladder, bile duct, distal edge of the pancreatic tail, and main pancreatic duct because it is easier to locate a lesion when these regions are imaged in the long axis. This capability has also made radial EUS a popular choice for screening in Japan.
EUS-FNA has been proliferating in recent years. More and more facilities in Japan are now using convex EUS for screening as well. As shown in the randomized controlled trial of radial EUS and convex EUS conducted by Kaneko, et al.*, delineation of the pancreatic head-body transition region and the hepatic hilar region using radial EUS may be inferior to that using convex EUS. Another disadvantage of radial EUS is that EUS-FNA is not possible no matter how excellent delineation is. Before deciding to use radial EUS, be sure that you fully understand both its strong points and its weak points.

Role of preprocedural MRCP
During EUS imaging, it is necessary to refrain from insufflation in order to obtain good ultrasound images. This often makes it difficult to correctly identify the position of the transducer in the endoscopic image. In this case, it is often necessary to estimate the position of the transducer by examining the EUS image.
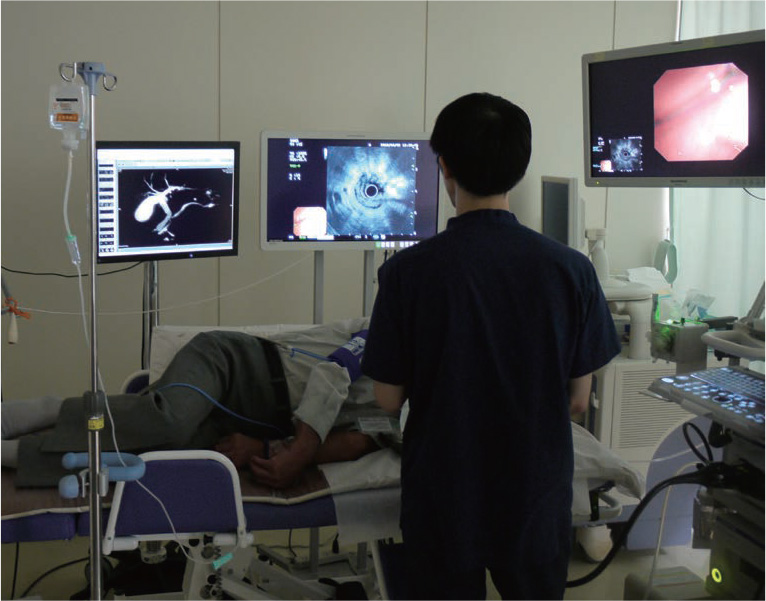
This issue is one of the biggest reasons why beginners find EUS so difficult to learn. To solve this issue, use abdominal MRI (MRCP) prior to EUS to scan the corresponding regions. Display the MRCP images alongside the EUS images in front of the endoscopist so that they can compare them in real time (Fig. a). This makes observation much easier.
For example, by comprehending the relationship between the positions of the gallbladder and liver and the displacement of the common bile duct, you can estimate the position of the transducer from where the gallbladder and common bile duct can most easily be imaged. Furthermore, understanding dilatation and stricture in the common bile duct and the main pancreatic duct may make it easier to compare the long-axis images of radial EUS with the images of MRCP.
Abbreviations used in this handbook
- Content Type