Small Intestine case 3
Dr. Takahiro Ito
Sapporo Higashi Tokushukai Hospital, IBD Center
Introduction
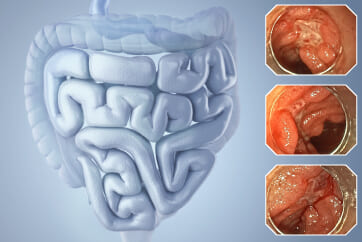
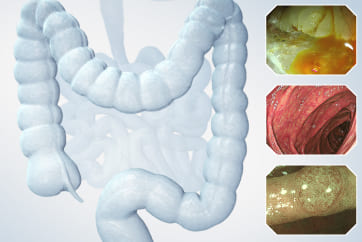
Crohn’s Disease (CD) is a chronic inflammatory bowel disease of unknown origin that causes ulcers and persistent inflammation throughout various sections of the gastrointestinal tract, leading to complications such as stricture, abscesses, and perforation. The small intestine, being narrow, is particularly susceptible to ‘stricture,’ complicating the insertion of endoscopes and thereby hindering diagnosis and diminishing the effectiveness of medical treatments. This is often a primary reason for surgical interventions. Our center proactively performs endoscopic balloon dilation (EBD) to avoid surgery, with small bowel endoscopy playing a critical role.
Furthermore, preventing intestinal complications such as strictures in CD treatment is crucial, and in patients with multiple risk factors, early use of biologic agents is common. However, long-term administration is necessary to maintain clinical and endoscopic remission. Our center proposes discontinuing biologic therapy for patients with very favorable progress under specific conditions. Discontinuation is suggested only if the patient is clinically in remission, shows long-term negative serological inflammation markers, and has confirmed mucosal healing of the digestive tract through endoscopy at least twice over a year. The absence of small intestinal lesions is crucial when discontinuing biologic therapy, highlighting the significant contribution of small bowel endoscopy.
Therefore, we have examined the utility of small bowel endoscopy, particularly in endoscopic treatment including EBD, and its effectiveness in confirming mucosal healing and other endoscopic diagnostics, using the newly released SIF-H190.
Utilization of SIF-H190 at Our Center
From April to November 2021, SIF-H190 was used 59 times (orally 12 times, anally 47 times), with 43 of these instances for EBD purposes. On average, 1.5 EBD procedures were performed per small bowel endoscopy session. The large diameter of the SIF-H190’s forceps channel, increased from 2.8mm in the older SIF-Q260 model to 3.2mm, facilitates easier handling of biopsy forceps and balloon dilators.
Operational Characteristics of SIF-H190 Compared to SIF-Q260
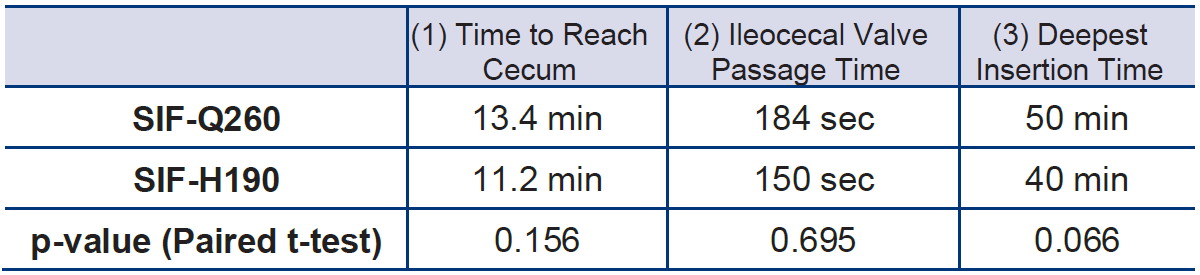
Of the 47 CD patients who underwent anal insertion of the SIF-H190, 19 had previously undergone small bowel endoscopy using the SIF-Q260 with the same endoscopist. The average time to reach the cecum was 13.4 minutes with the SIF-Q260, whereas it was reduced to 11.2 minutes with the SIF-H190, showing a trend toward decreased cecal intubation time (p=0.156, paired t-test). This improvement is attributed to the passive bending feature of the SIF-H190. (Video of colon insertion with SIF-H190: Video 1, SIF-Q260: Video 2).
After reaching the cecum, while attempting to pass through the ileocecal valve and insert into the ileum, it is common for the intestinal tube to slip away, causing the scope’s tip to inadvertently return to the cecum. In such cases, it is advisable to proceed with a downward angle rather than persistently pushing, though this can still be challenging. Previously, when it was difficult to pass the ileocecal valve, our center would leave the tip of the sliding tube in the ascending colon, remove the SIF-Q260, and pass a PCF-PQ260L, equipped with a passive bending feature, through the sliding tube. After navigating through the ileocecal valve and advancing some distance into the ileum, the sliding tube would be advanced further into the ileum before switching back to the SIF-Q260. This technique, not applicable to double-balloon endoscopy, was a useful method. With the advent of the SIF-H190, which also has a passive bending feature, the need for scope exchange has been eliminated, making it easier to pass the ileocecal valve (Video 3). Analysis of the time taken to pass the ileocecal valve in the aforementioned 19 patients showed no significant difference, with an average of 184 seconds for SIF-Q260 compared to 150 seconds for SIF-H190 (p=0.695). Among these, in 11 patients where the insertion depth was the same for both SIF-Q260 and SIF-H190, the time taken to insert from the anus to the deepest point was reduced from an average of 50 minutes with SIF-Q260 to 40 minutes with SIF-H190 (p=0.066), suggesting a total reduction in insertion time (Table 1). In fact, a male patient in his 40s, who had undergone several anal small bowel endoscopies with SIF-Q260 previously, reported significantly less discomfort during the examination with SIF-H190, though he was not informed of the change in equipment.
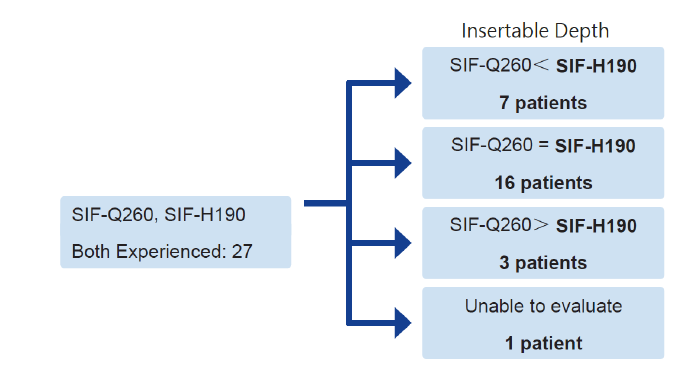
In Crohn’s Disease, a number of patients have extensive lesions extending up to the upper ileum and jejunum, making deep insertion crucial. Among patients who have experienced insertions with both SIF-H190 and SIF-Q260, 7 out of 27 were able to achieve deeper insertions with the SIF-H190 compared to the SIF-Q260, 16 had similar depths of insertion, and 3 actually had lesser depths of insertion with the SIF-H190 (Figure 1). The introduction of the SIF-H190, equipped with passive bending capabilities and a high-transmission insertion section, has made it possible to reach areas of the small intestine that were previously inaccessible (Videos 4 and 5). On the other hand, depending on the adhesions and deformations of the intestines, there are cases where SIF-Q260 may be easier to insert. Moving forward, if necessary, we will continue to use the method described previously, switching between SIF-H190 and SIF-Q260, to achieve deeper insertions.
[Tbl. 1] Comparison of Insertion Times for New and Old Anal Small Bowel Endoscopes (Performed by the Same Endoscopist)
Video 1: Fluoroscopy during the Colon Insertion of SIF-H190
Video 2: Fluoroscopy during the Colon Insertion of SIF-Q260
Video 3: Passive Bending
Video 4: Insertion into the Deep Small Intestine
Video 5: Insertion into the Deep Small Intestine
[Fig. 1] Comparison of Insertion Depths for New and Old Anal Small Bowel Endoscopes (Performed by the Same Endoscopist)
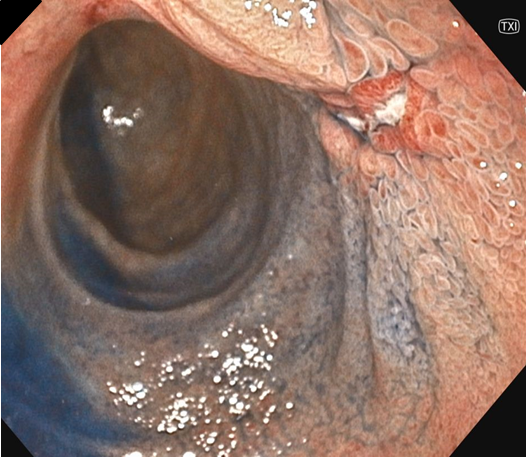
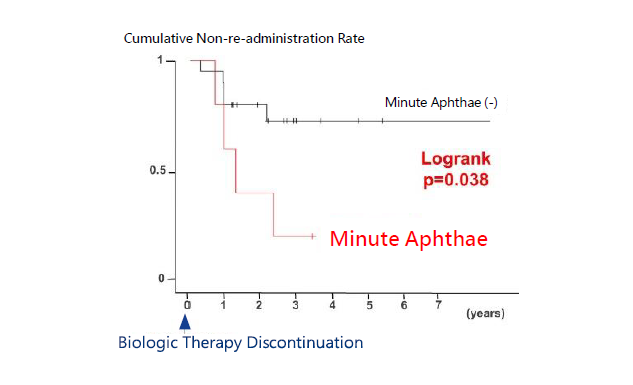
Functionality of EVIS X1 in Assessing Small Intestinal Lesions in Crohn's Disease The Efficacy of "TXI"
At our center, we propose discontinuing biologic therapy for Crohn’s Disease (CD) patients whose treatment progress with biologic agents has been favorable. However, it is essential to confirm the condition of the intestinal mucosa endoscopically during this process. Previously, we reported that the presence of minute aphthae at the time of biologic therapy discontinuation is a risk factor for relapse (Ito et al., 101st Workshop of the Japanese Society of Gastrointestinal Endoscopy, 2021). In other words, if small aphthae remain when biologic therapy is discontinued, there is a significant likelihood of relapse, necessitating the re-administration of biologic agents (Figure 2). Therefore, it is advisable not to discontinue biologic therapy if even the smallest aphthae are present. The detection of such minute aphthae would greatly benefit from high-resolution endoscopic images or image enhancement modes designed to facilitate their identification.
[Fig. 2] The Presence of Minute Aphthae in Crohn's Disease is Associated with the Re-administration of Biologic Agents After Discontinuation
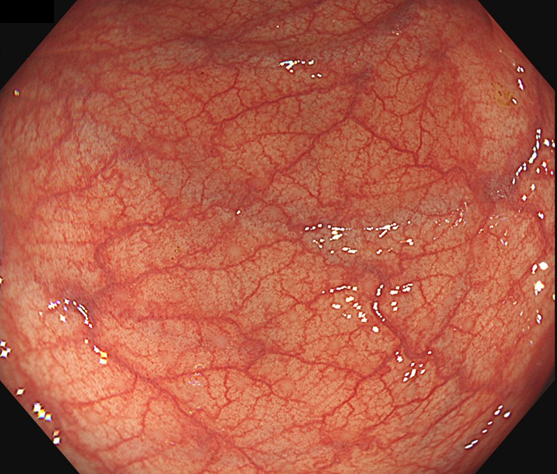
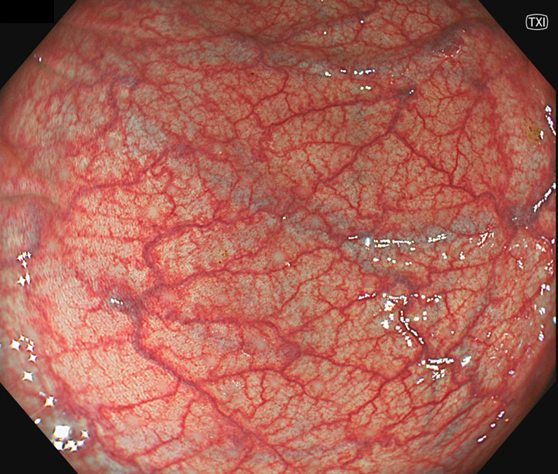
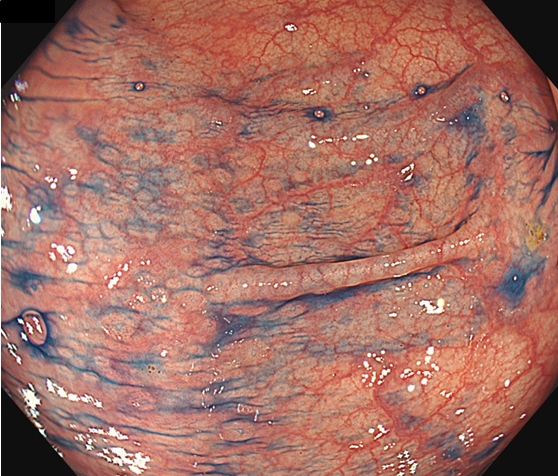
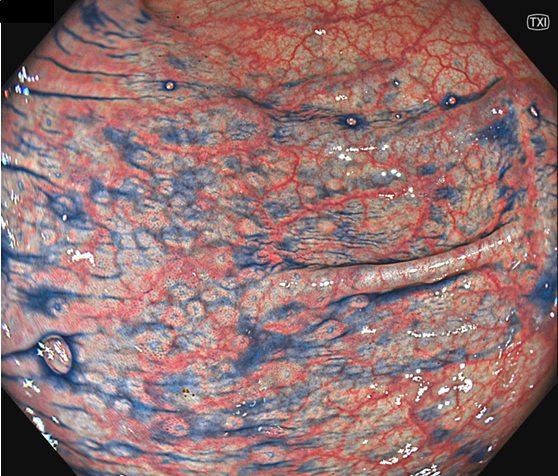
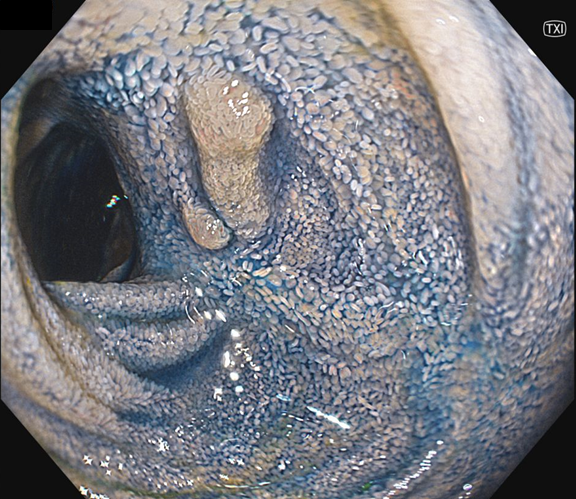
[Fig. 3] Colonic Mucosa of a CD Patient Observed with CF-XZ1200I. TXI Enhances the Detection of Minute Lesions Such as Lymph Follicles, and Dye Spraying Further Improves Clarity
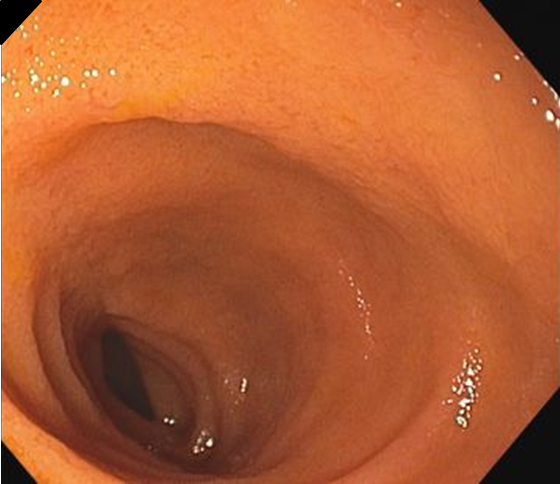
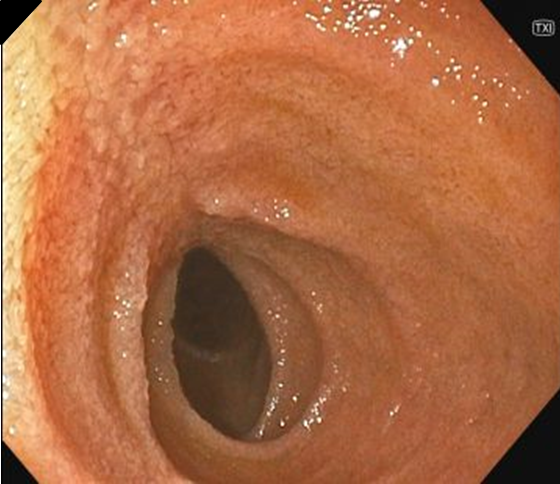
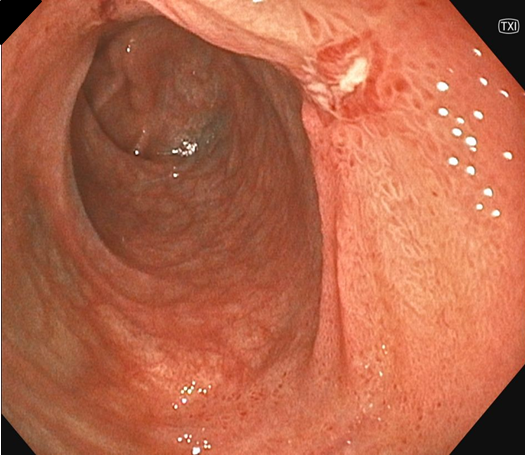
In this instance, the SIF-H190 and CF-XZ1200I were utilized to assess the efficacy of TXI. TXI’s texture and color enhancement capabilities clarified the contours of villi, making it easier to detect lymph follicles and minute aphthae. Furthermore, the application of indigo carmine dye enhanced the contrast between reddish areas and the indigo carmine’s depressions, facilitating the detection of subtle changes (Figures 3 to 6). As a result, this technology is expected to become a powerful tool in determining the effectiveness of treatments for Crohn’s Disease, especially in assessing mucosal healing, and could significantly aid in decisions regarding the cessation of biologic therapy.
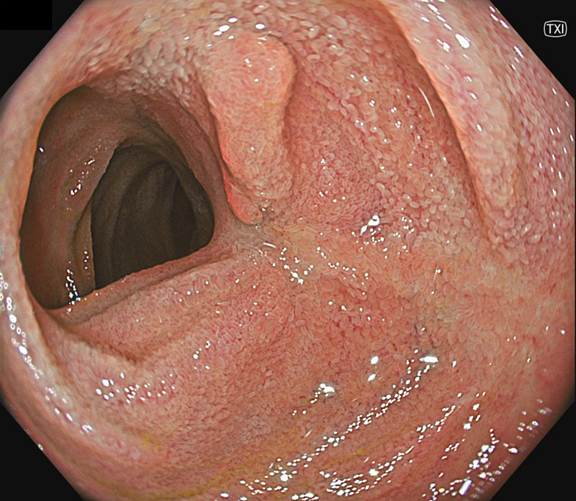
[Fig. 4] Scarring in the Ileum of a CD Patient Without Aphthae Using CF-XZ1200I. Even with TXI Alone, Minute Aphthae Can Be Detected
Video 6: Combined Use of TXI and Dye Spraying
[Fig. 5] Scarring in the Ileum of a CD Patient Without Aphthae Using SIF-H190. Even with TXI Alone, Minute Aphthae Can Be Detected
Video 7: Detailed Observation of Scarring Using TXI
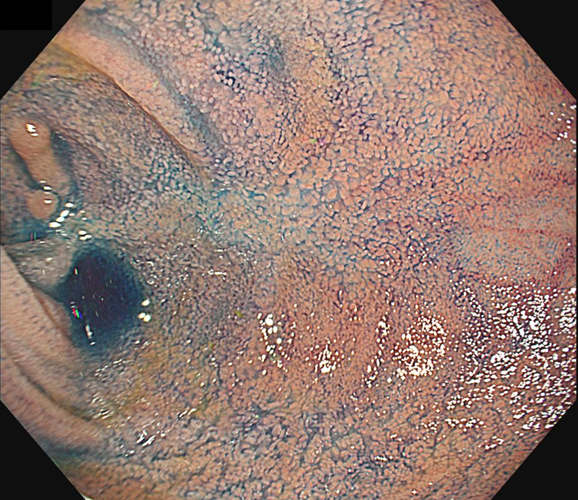
[Fig. 6] Ulcer in the Healing Process of the Ileum in a CD Patient Observed with SIF-H190.
Future Prospects for Endoscopic Treatment of Small Intestinal Lesions in Crohn's Disease
The development and advancement of small bowel endoscopy, small bowel MRI, and capsule endoscopy have made it easier to detect small intestinal lesions that were previously difficult to identify. Consequently, it is anticipated that small bowel endoscopy will play an increasingly important role in observing detailed mucosal lesions, assessing disease activity, differentiating Crohn’s Disease from other conditions, and managing stenotic or bleeding lesions. Many patients have widespread lesions not only in the terminal ileum but also in the jejunum and other parts of the small intestine. Therefore, it is essential to perform deeper insertions for examination and treatment while minimizing time and being mindful of complications. The insertion capability and operability of the SIF-H190, combined with the high-resolution endoscopic images and “TXI” of the EVIS X1 system, are expected to make significant contributions to the diagnosis and treatment of Crohn’s Disease.
- Content Type