Utilizing Radial EBUS in Bronchoscopic Evaluation of Lung Nodules Detected in Lung Cancer Screening Program
Clinical Case Report

Asst. Prof. Sonja Badovinac, MD, PhD
Head of Bronchoscopy and Interventional Pulmonology Unit
University Hospital Center Zagreb
Introduction
The introduction of lung cancer screening programs across Europe has presented a new challenge in determining the etiology of peripheral lung lesions1. Although CT-guided transthoracic biopsy is a standard procedure for such cases, with diagnostic yield of 90%, the significant burden of periprocedural complications highlights the need for a safer and more successful diagnostic alternative2,4. Bronchoscopy with a slim bronchoscope combined with radial endobronchial ultrasound (radial EBUS), offers a viable approach for sampling peripheral lesions significantly reducing the risk of iatrogenic complications such as pneumothorax and bleeding4. Here we present the case of a patient who underwent both procedures.
Case Presentation
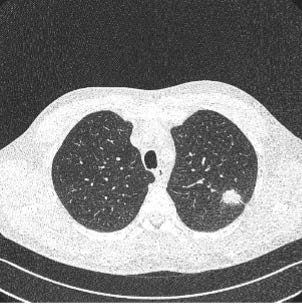
A 63-year-old male was referred to our clinic for a diagnostic workup following a suspicious nodule detected
in the left upper lobe of the lung on low-dose computed tomography (LDCT) as part of the Croatian National Lung Cancer Screening Program (Figure 1). The patient had a significant smoking history with a cumulative exposure of 45 pack-years and occupational exposure to wood dust. He did not have malignant diseases in
his family history and he was without any significant comorbidities. Laboratory investigations did not reveal
any abnormal findings.
Initially the patient was presented for transthoracic biopsy under multislice computed tomography (MSCT).
A positron emission tomography-computed tomography (PET-CT) scan was also recommended.
Two biopsy cores were successfully obtained, however the procedure was complicated by moderate bleeding (Figures 2,3). The patient was subsequently observed in the Day Care Unit and was discharged after several hours without further incident.
Pathologic examination of the biopsy specimens revealed a limited number of atypical cells, which were insufficient for comprehensive pathological analysis. In case of sustained clinical suspicion, a repeated biopsy was advised.
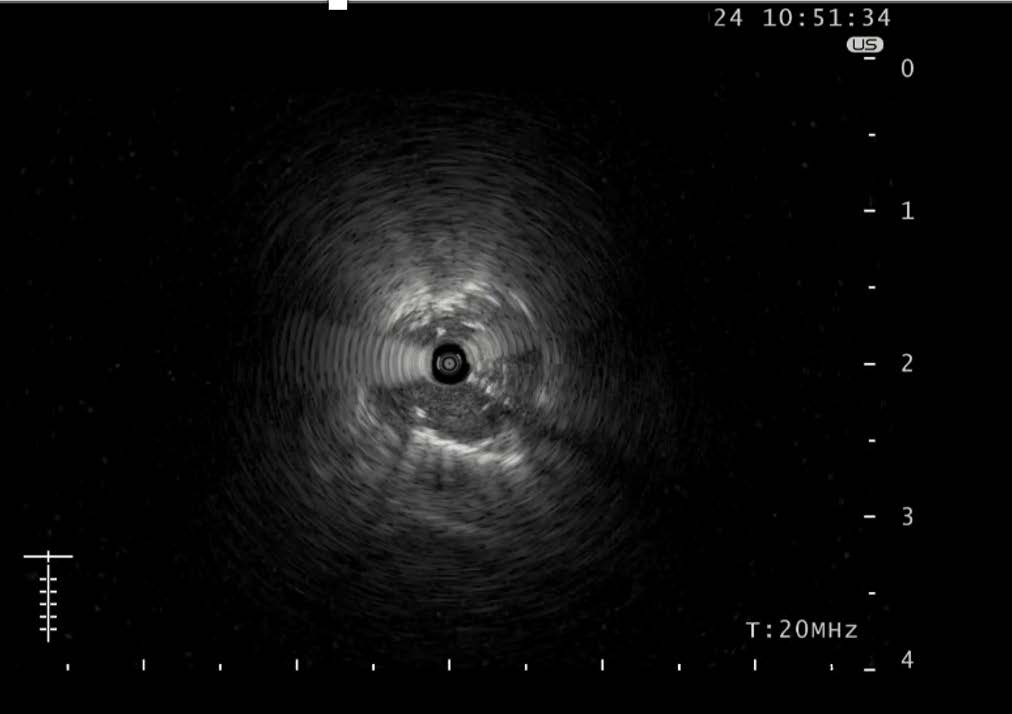
Following the transthoracic CT-guided biopsy the patient was referred for a bronchoscopy and radial EBUS procedure. Bronchoscopy was performed using the BF-P190 bronchoscope, and showed no evidence of endoluminal pathology. Subsequently, an examination using the radial EBUS mini-probe (UM-S20-17S) was conducted. The procedure was performed with the GuideSheath Kit (K-401) and revealed an irregular pathological echo in the LB2 subsegmental bronchus. (Figure 4).
The preplanned sampling strategy involved obtaining tissue samples utilizing all tools available with the GuideSheath Kit which consists of biopsy forceps, a cytology brush and catheter aspiration. Additionally,
to maximize tissue yield for pathological analysis especially given the challenging location of the lesion, transbronchial needle aspiration (TBNA) was additionally performed using the PeriView FLEX 21G needle.
Biopsy samples, three TBNA samples, cytology brush and catheter aspirate were successfully collected.
The procedure was completed without any periprocedural complications.
Pathological analysis of collected specimens confirmed a diagnosis of lung adenocarcinoma. Predictive biomarker testing showed that the tumour was negative for EGFR, ALK, and ROS1 mutations, with a PD-L1 expression of 70%. After PET-CT scan that confirmed operable disease the patient was referred to thoracic surgery.
Conclusion
Peripheral lung nodules pose a significant diagnostic challenge in clinical practice. As lung cancer screening programs become more widely implemented there is increasing demand for accurate characterization of these nodules1. Radial EBUS represents a viable and effective diagnostic method for assessing peripheral lung nodules with a diagnostic yield of approximately 70% and a valuable safety profile in comparison with the
CT-guided transthoracic biopsy4,6. We found the GuideSheath supportive for the positioning of the target lesion during sampling, while the combination of multiple sampling techniques helped to collect sufficient tissue acquisition for comprehensive pathological analysis.
It was also beneficial, in this case to incorporate the PeriView FLEX 21G needle into the armamentarium of sampling tools. This needle is particularly valuable for smaller lesions or in cases with an eccentric ultrasound view during a radial EBUS examination. In this patient, radial EBUS was the diagnostic method that confirmed lung adenocarcinoma and the selected sampling tools successfully provided sufficient tissue for complete pathological analysis including predictive biomarker testing.
References
1 de Koning HJ, van der Aalst CM, de Jong PA, Scholten ET, Nackaerts K, Heuvelmans MA, Lammers JJ, Weenink C, Yousaf-Khan U, Horeweg N, van ‘t Westeinde S, Prokop M, Mali WP, Mohamed Hoesein FAA, van Ooijen PMA, Aerts JGJV, den Bakker MA, Thunnissen E, Verschakelen J, Vliegenthart R, Walter JE, Ten Haaf K, Groen HJM, Oudkerk M. Reduced Lung-Cancer Mortality with Volume CT Screening in a Randomized Trial. N Engl J Med. 2020 Feb 6;382(6):503-513. doi: 10.1056/NEJMoa1911793. Epub 2020 Jan 29. PMID: 31995683.
2 Tsukada H, Satou T, Iwashima A, Souma T. Diagnostic accuracy of CT-guided automated needle biopsy of lung nodules, AJR Am. J. Roentgenol. 175 (2000) 239-243.
3 Heerink WJ, de Bock GH, de Jonge GJ, Groen HJ, Vliegenthart R, Oudkerk M. Complication rates of CT-guided transthoracic lung biopsy: meta-analysis, Eur. Radiol. 27 (2017) 138-148.
4 Ho ATN, Gorthi R, Lee R, Chawla M, Patolia S. Solitary Lung Nodule: CT-Guided Transthoracic Biopsy vs Transbronchial Biopsy With Endobronchial Ultrasound and Flexible Bronchoscope: A Meta-Analysis of Randomized Controlled Trials. Lung. 2023 Feb;201(1):85-93. doi: 10.1007/s00408-023-00596-9. Epub 2023 Jan 25. PMID: 36695890.
5 Nadig TR, Thomas N, Nietert PJ, Lozier J, Tanner NT, Wang Memoli JS, Pastis NJ, Silvestri GA. Guided Bronchoscopy for the Evaluation of Pulmonary Lesions: An Updated Meta-analysis. Chest. 2023 Jun;163(6):1589-1598. doi: 10.1016/j. chest.2022.12.044. Epub 2023 Jan 11. PMID: 36640994; PMCID: PMC10925546.
6 Tian S, Li X, Liu J, Wang X, Chen H, Dai Z, Chen Q, Shi H, Li Y, Huang H, Bai C. Radial endobronchial ultrasound – guided bronchoscopy for the diagnosis of peripheral pulmonary lesions: A systematic review and meta-analysis of prospective trials. Heliyon. 2024 Apr 9;10(8):e29446. doi: 10.1016/j.heliyon.2024. e29446. PMID: 38660275; PMCID: PMC11040069.
7 Zuccatosta L, Latini L, Belleggia B, Gonnelli F, Barbisan F, Goteri G, Gasparini S and Marchetti A (2023) Suitability of transbronchial needle aspiration for genotyping peripheral pulmonary tumors. Front. Med. 9:1087028. doi: 10.3389/fmed.2022.1087028
- Content Type