Dr. Amir Hanna
Interventional Pulmonologist
at Marie Lannelongue Hospital (Paris, France)
Interventional pulmonology is a fast-evolving field. What began with the use of basic instruments to examine airways and perform biopsies has now progressed to advanced techniques like robotic bronchoscopy. This shift mirrors the transformation seen in gastroenterology two to three decades ago, where emerging technologies significantly reduced the reliance on exploratory laparoscopy.
The Real Challenge
The rise in peripheral pulmonary nodule (PPN) diagnosis, driven by advancements in imaging technology and lung cancer screening programs, presents a significant challenge for health-care professionals. These nodules are a common occurrence in daily practice, and their evaluation requires careful consideration of biopsy techniques, each with its own strengths and limitations:
1. Surgical Lung Biopsy: This method offers both diagnostic and therapeutic benefits in a single procedure.
However, the percentage of negative surgical lung biopsies can vary widely. In cases of interstitial lung disease (ILD), the negative rate ranges from 10% to 30%.1 However, for conditions like lung cancer, where surgical biopsies are more targeted, the rate of negative or nondiagnostic biopsies is typically below 10%.1
2. Transthoracic Lung Biopsy: While this technique provides a higher diagnostic yield, it carries an increased risk of complications, such as pneumothorax, bleeding and air embolism, compared to bronchoscopic approaches.2
3. Bronchoscopy Lung Biopsy: Various techniques have been developed to enhance peripheral navigation, including:
∙ Radial EBUS probes
∙ Electromagnetic navigation
∙ Robotic bronchoscopy
∙ Cone beam CT
Each of these four techniques plays a role in improving diagnostic accuracy while balancing cost-effectiveness.
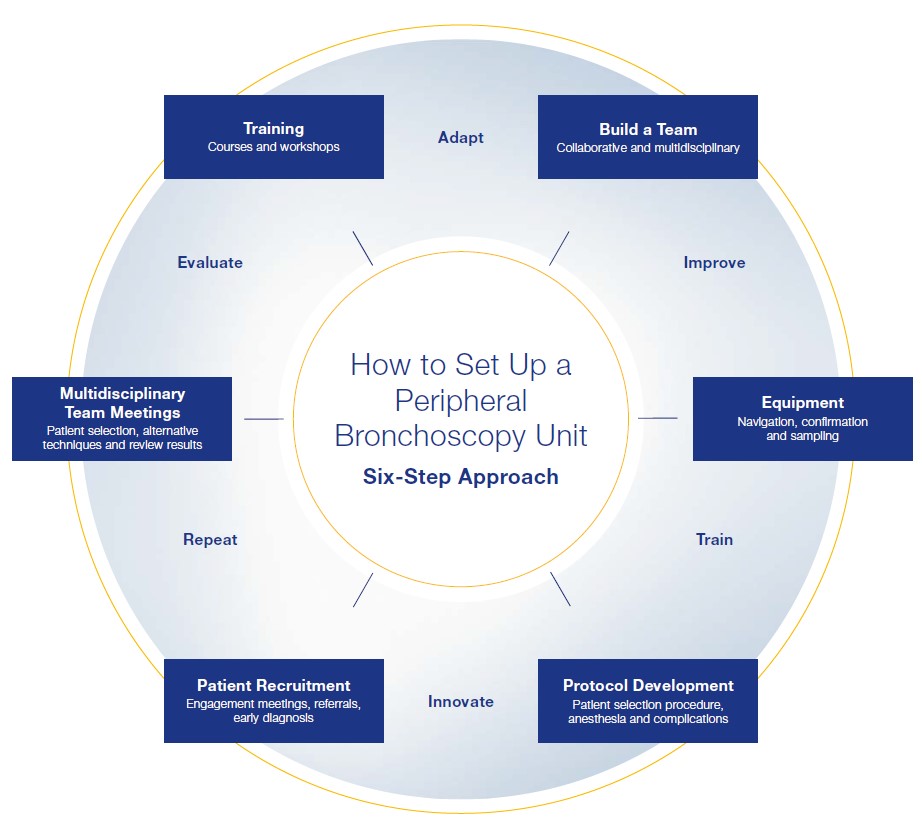
How to Set Up a Peripheral Pulmonary Nodule Service
The Six-Step Approach
While funding is often the first thing that comes to mind, it alone is not enough to develop an advanced peripheral bronchoscopy platform. The six-step approach encompasses the key factors involved in setting up a peripheral pulmonary nodule (PPN) service.
Step 1: Training
∙ Medical and Paramedical: Ensure all medical personnel, including nurses and technicians, receive specialized training.
∙ Courses: Engage in educational courses focused on PPN diagnostics and treatment.
∙ Workshops: Provide hands-on workshops for real-time learning.
∙ Airway Anatomy: Focus on in-depth understanding of airway anatomy to improve procedural accuracy.
Step 2: Build a Team
A collaborative, multidisciplinary approach enhances the overall care and decision-making process.
∙ Interventional pulmonology
∙ Thoracic surgery
∙ Interventional radiology
∙ Thoracic oncology
∙ Anesthesiology
Step 3: Equipment (Three Tools)
∙ Navigation Tools: Instruments to guide you from point A to point B, such as the ultrathin bronchoscope, electromagnetic navigation or robotic bronchoscopy.
∙ Confirmation Tools: Use real-time confirmation tools like radial EBUS probes to verify nodule location.
∙ Biopsy Tools: Choose from biopsy forceps, needle biopsy, brush and cryobiopsy.
In my practice, I combine an ultrathin bronchoscope, radial EBUS probe and cryobiopsy with forceps and needle biopsy techniques. This combination offers a high diagnostic yield while potentially keeping costs lower.
Step 4: Protocol Development
∙ Patient Selection: Set clear criteria for identifying appropriate candidates for the procedure.
∙ Procedure Outline: Standardize the steps of the bronchoscopy process.
∙ Anesthesia Protocol: Design a tailored anesthesia protocol for optimal patient comfort and safety.
∙ Complication Management: Establish protocols for managing potential complications such as pneumothorax or bleeding.
Step 5: Patient Recruitment
∙ Multidisciplinary Team Meetings: Engage with your team to discuss potential candidates.
∙ Referring Physicians: Collaborate with referring doctors to identify suitable patients.
∙ Screening Programs: Use lung cancer screening programs to identify early-stage PPNs.
∙ Improve Diagnostics: Focus on improving diagnostic techniques to attract more patients.
Step 6: Multidisciplinary Team Meetings
∙ Patient Selection: Reassess patient suitability for bronchoscopy.
∙ Alternative Techniques: Discuss potential alternative approaches if necessary.
∙ Review Results: Share and analyze procedure outcomes with the entire team for continuous improvement.
Once everything is in place, the key to long-term success is continuous improvement: evaluate, adapt, improve, train, innovate and repeat. This ongoing cycle ensures the service stays at the forefront of medical advancements, maximizes patient outcomes, and fosters a culture of growth and excellence within the team.
Conclusion
Building a successful peripheral pulmonary nodule (PPN) service hinges on a well-executed six-step approach that integrates key elements for success. Comprehensive training, the foundation of this approach, ensures that both medical and paramedical staff are well-prepared. Establishing a strong multidisciplinary team allows for seamless collaboration across specialties. Choosing the right combination of navigation, confirmation and biopsy tools enhances diagnostic accuracy while managing costs effectively. A structured protocol for patient selection, procedure execution and anesthesia guarantees safety and consistency. Strategic patient recruitment, backed by referrals and screening programs, keeps the service thriving. Finally, regular multidisciplinary team meetings ensure continual evaluation, refinement and improvement. By following this six-step approach, a PPN service can deliver superior, high-quality care tailored to patient needs.
References
1 Coutinho, Gonçalo F., Rita Pancas, Eunice Magalhães, João E. Bernardo, Luís Eugénio, and Manuel J. Antunes. “Diagnostic Value of Surgical Lung Biopsy: Comparison
with Clinical and Radiological Diagnosis.” European Journal of Cardio-Thoracic Surgery 33, no. 5 (1 May 2008): 781-85. https://doi.org/10.1016/j.ejcts.2008.02.008.
2 Khan, Taha, Yasir Usman, Tony Abdo, Fawad Chaudry, Jean I. Keddissi, and Houssein A. Youness. “Diagnosis and Management of Peripheral Lung Nodule.” Annals
of Translational Medicine; Vol 7, no. 15 (August 14, 2019): (Focus on “Diagnostic and Therapeutic Advances in the Management of Lung Cancer”), 2019. https://atm.
amegroups.org/article/view/24877.
- Content Type