Introduction
Pelvic organ prolapse (POP) is the dominant pathological condition in urogynecology. With the continuous development of minimally invasive surgery techniques the medical treatment of apical compartment defects and mixed defects has achieved significant improvement. Due to advances in laparoscopic surgery of urogynecological disorders this treatment may be provided to a wide range of patients. Beginning in the 1990s, laparoscopic promontofixation (LSC – laparoscopic sarcopexy) has become the gold-standard treatment for apical compartment prolapse.
Case Report
A 63-year-old woman, who underwent uterine corpus amputation due to uterine fibroids several years ago, came to our medical centre with symptoms of cervical stump prolapse accompanied by mixed urinary incontinence syndrome. After the initial diagnosis, she was qualified for surgical treatment using the LSC / promontofixation procedure. The procedure was performed under general anesthesia and the patient was discharged home after another two days. At the time of discharge from the hospital, the patient did not experience any discomfort in area of the reproductive system, and the causes of previous ailments were successfully eradicated.
Procedure
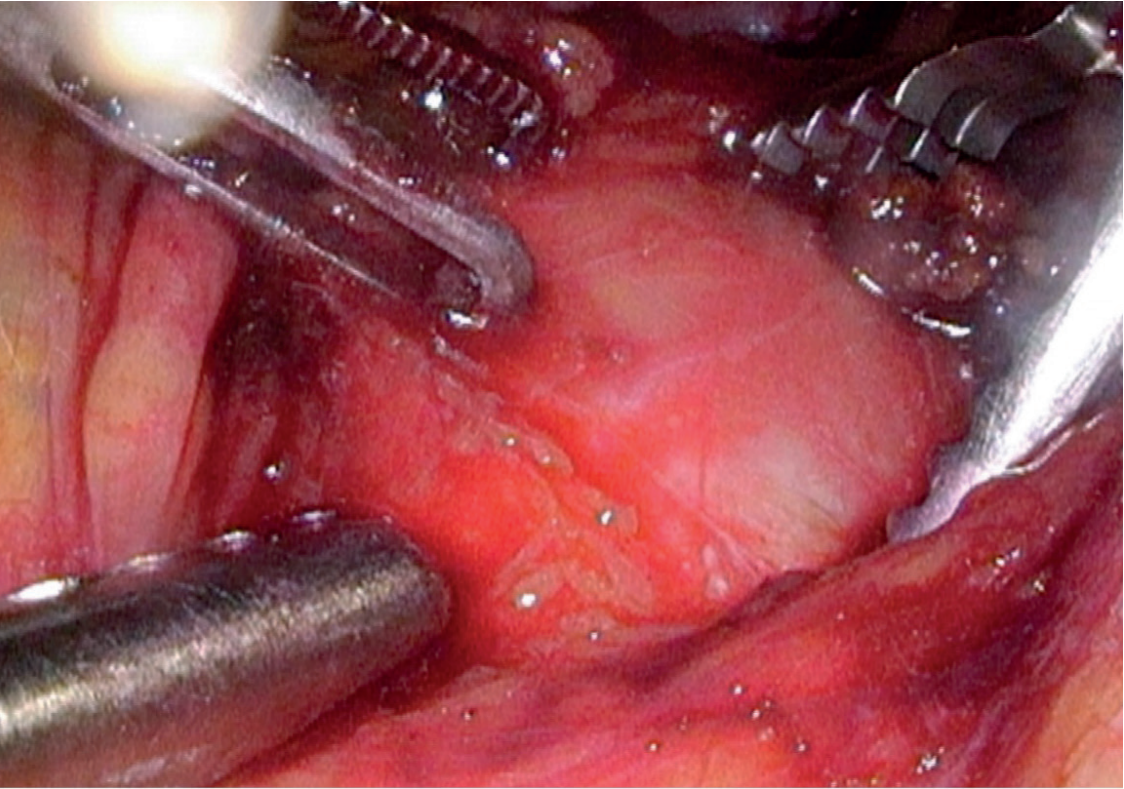
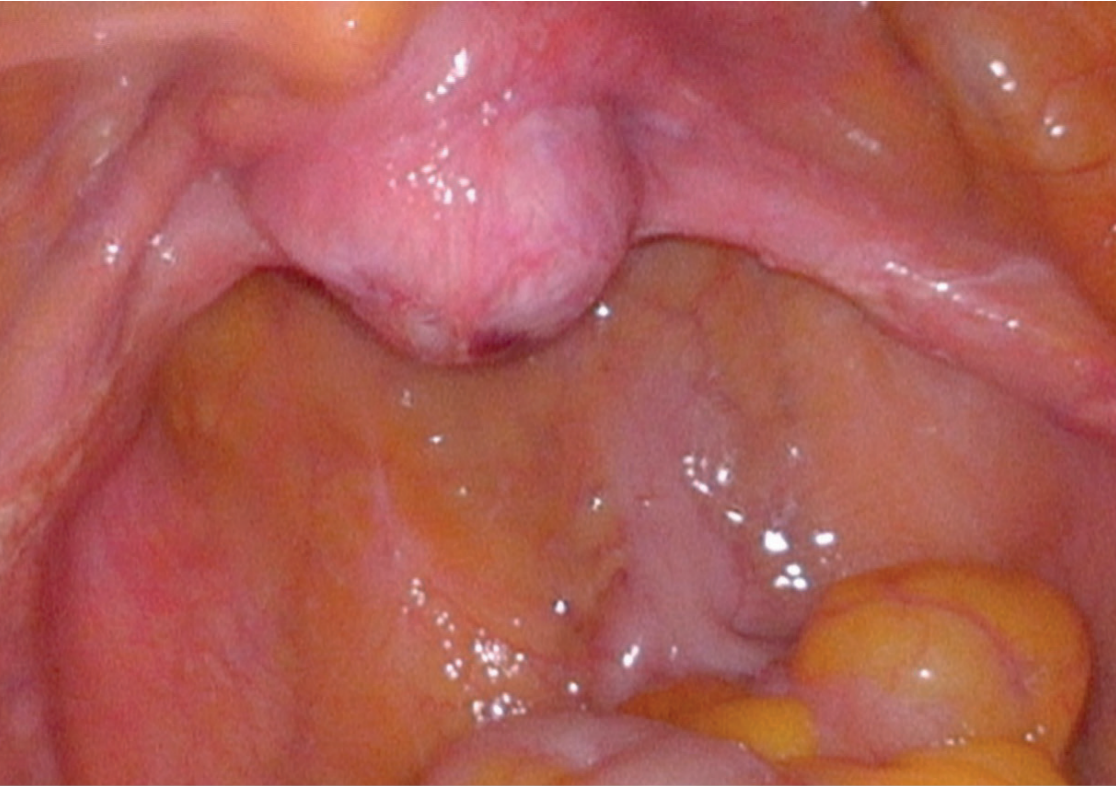
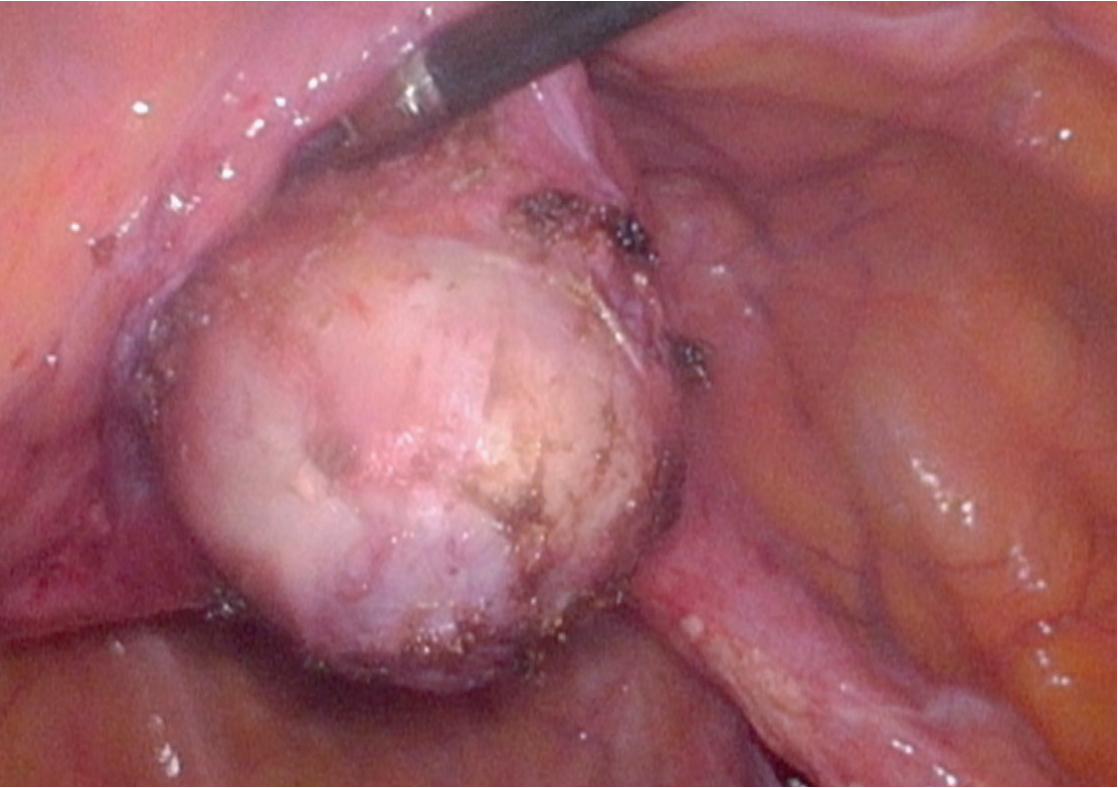
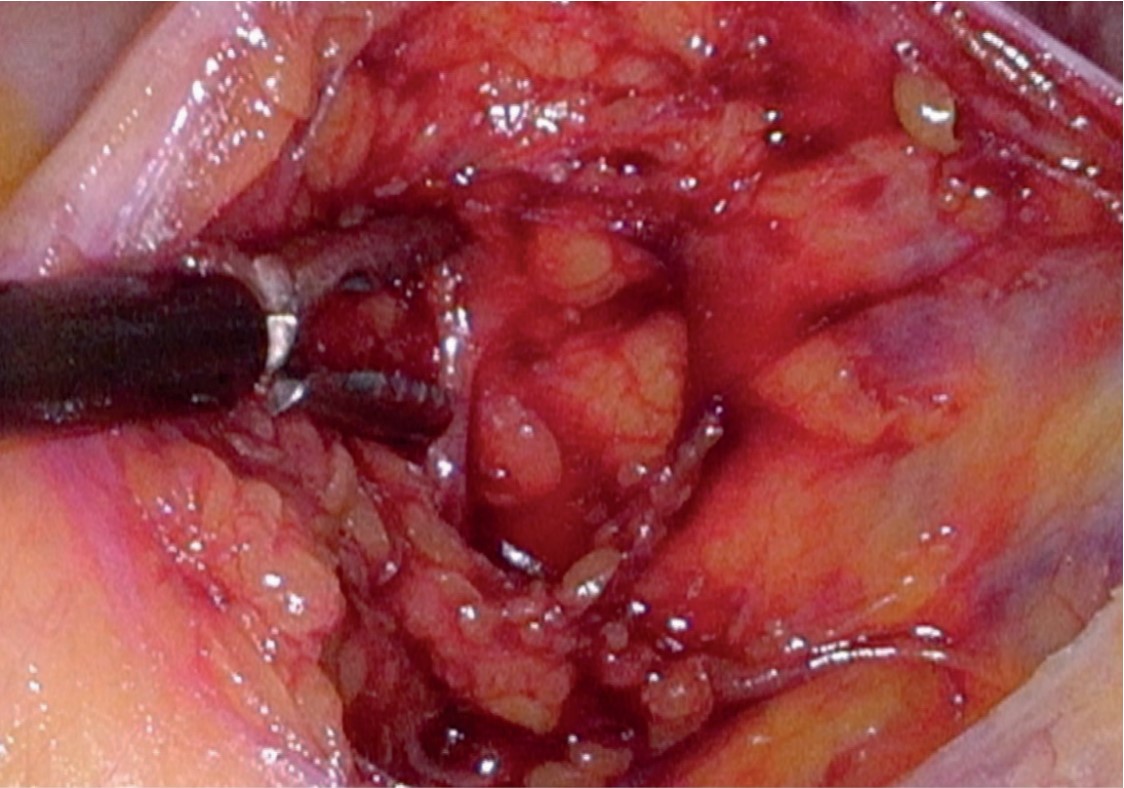
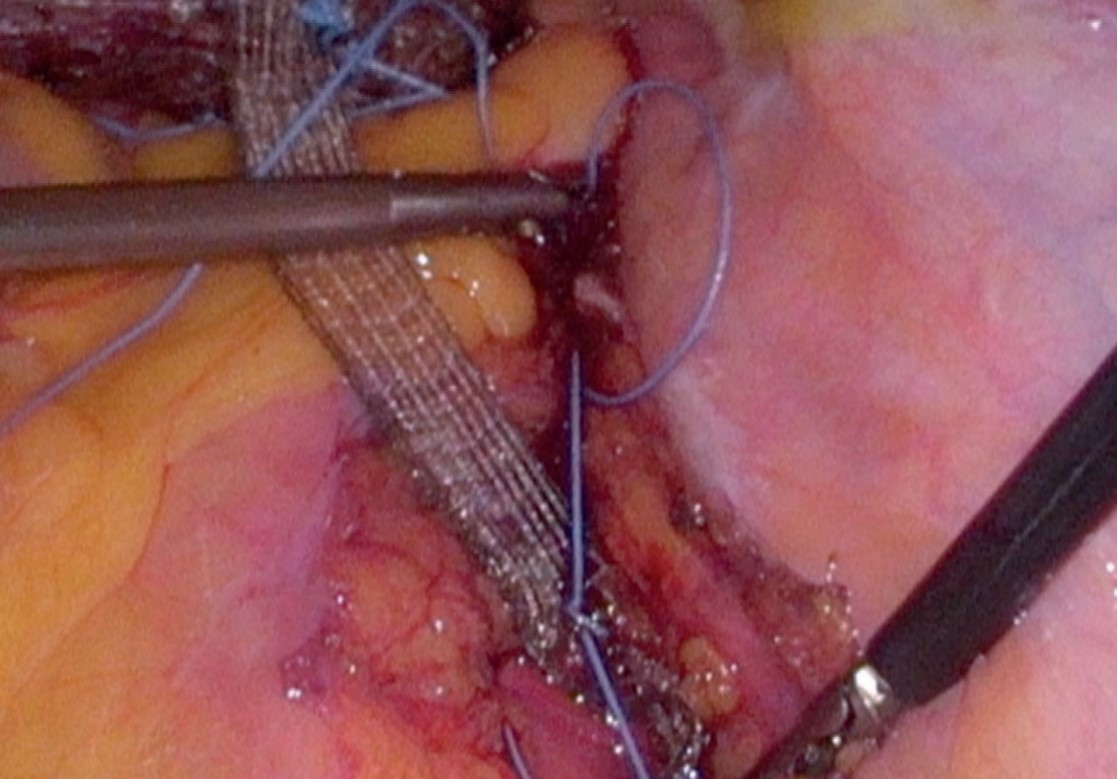
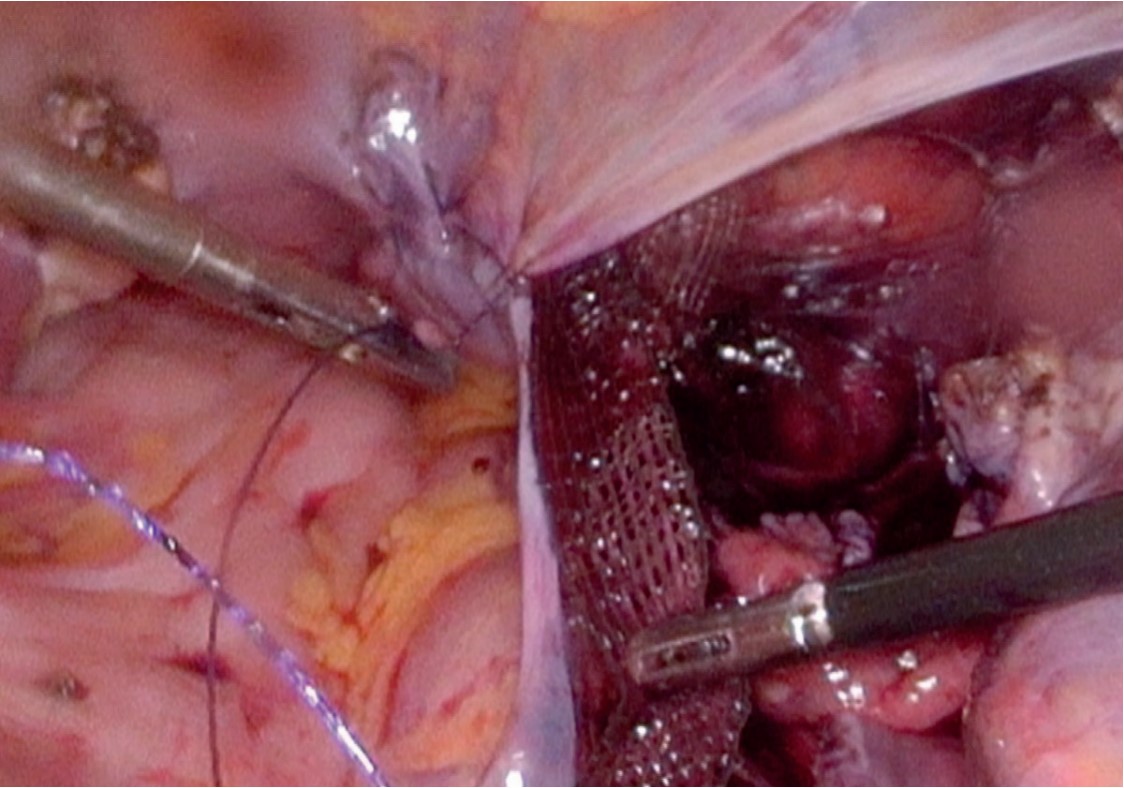
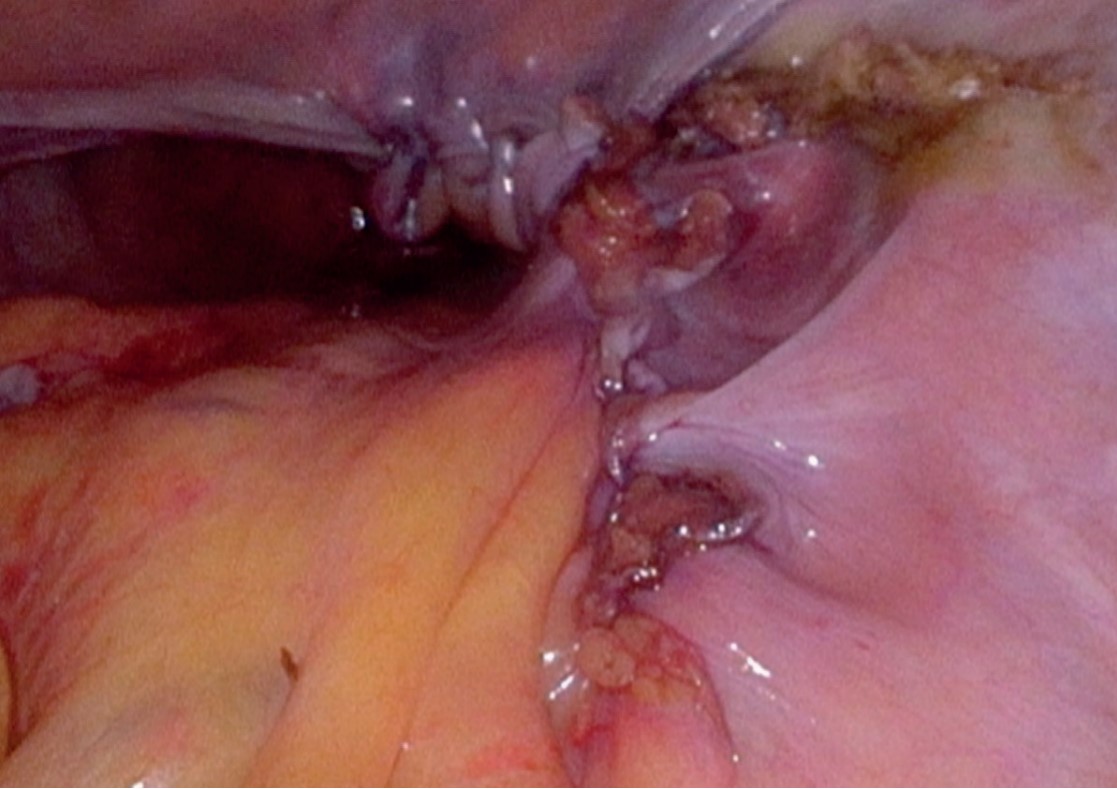
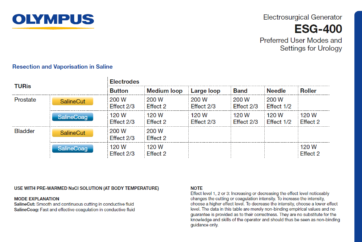
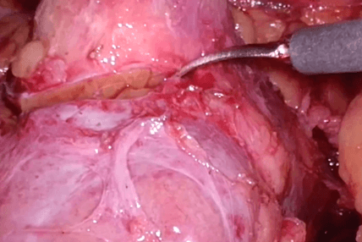
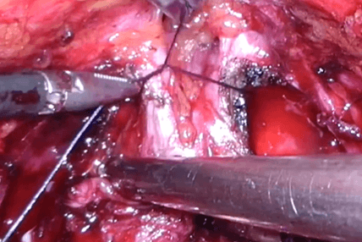
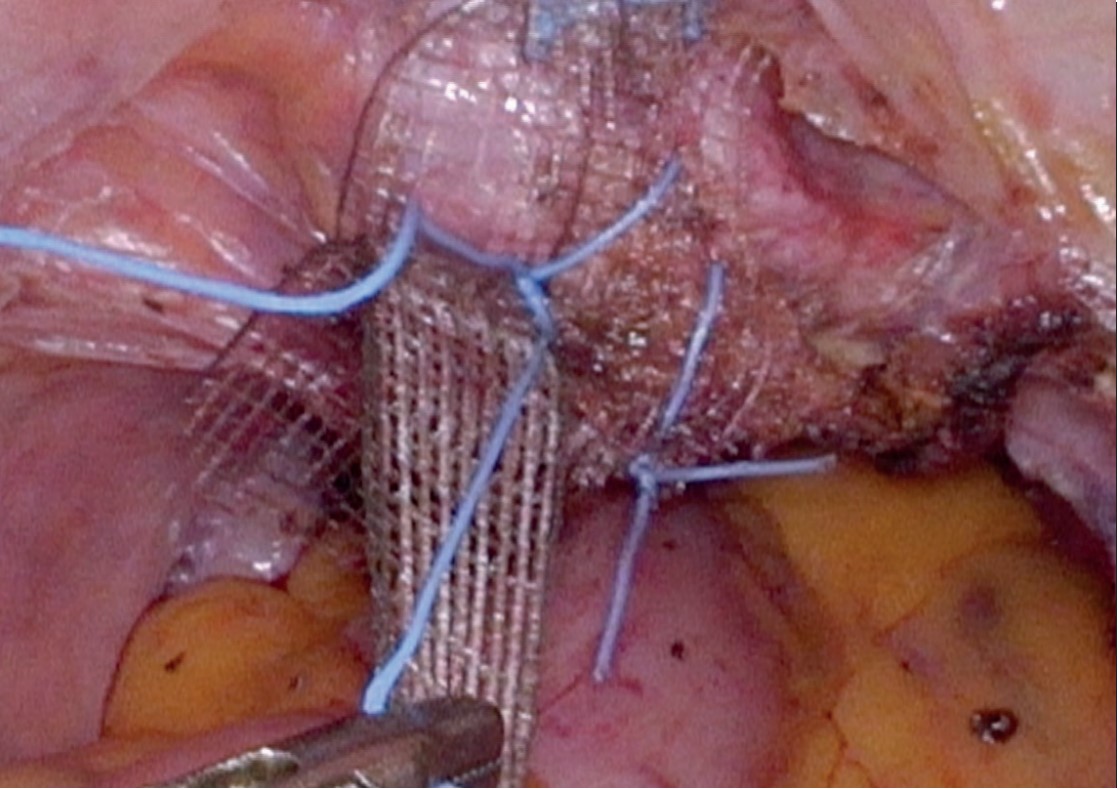
After performing standard insufflation and visual inspection of the abdominal organs, the surgeon proceeds with the main phase of the procedure. The first step includes exposition of the operating field, and the exposure and dissection of the promontory and the cervical stump are of key importance [Fig.1; Fig.2]. Next, the cervical stump is dissected from the urinary bladder [Fig. 3]. The next step is to open the retroperitoneal space and to expose the ureter, iliac vessels and the hypogastric nerve [Fig. 4]. Polypropylene mesh is fixed to the dissected cervical stump and the promontory (anterior longitudinal ligament) using simple interrupted sutures while adjusting their length and tension [Fig.5; Fig.6]. Once the mesh is placed into the retroperitoneal space, the parietal peritoneum is sutured with a knotless barbed suture, e.g. V- Loc™ [Fig. 7; Fig.8].
Discussion
The advantages of promontofixation procedure include a good and permanent anatomical effect, i.e. positioning of the cervical stump in the axis most similar to the anatomical one, which is of key importance in the prevention of secondary genital prolapses. This reduces the reoperation rate to about 4%, and the effectiveness of surgery is estimated to be at 90-97%. Other advantages include the reduction of the risk of postoperative urinary incontinence and dyspareunia. The shorter operation time, hospital stay and faster recovery are other benefits of this technique as well as lower perioperative cardiac risk in the group of obese patients with concomitant diseases. The positive outcomes emphasized in the literature include also decreased postoperative pain, decreased intraoperative blood loss and lower overall treatment cost.
Laparoscopic promontofixation technique requires a higher level of operator’s skill; however, the learning curve is quite short for the experienced physician who performs other laparoscopic pelvic procedures. Undoubtedly, the use of 3D imaging system for this surgical treatment facilitates the procedure performance and minimises a risk of complications. 3D imaging allows the surgeon to visualize very precisely the spatial position of the cervical stump. The precise dissection of anatomical structures is highly important in this type of surgery, which is also facilitated by the 3D technique. Suturing makes up a significant part of the procedure. The use of 3D imaging helps to reduce the operative time because suturing and knot-tying techniques may be performed more easily.
The complications of this procedure include bowel damage and obstruction, injury risk to the iliac vessels and the ureter. Significant disadvantages include also possible anatomical variations encountered within the operating field, e.g. peritoneal adhesions, as well as high-complexity and technical difficulty of this procedure.
The advantages and disadvantages of the laparoscopic promontofixation procedure are presented in Table 1.
| ADVANTAGES | DISADVANTAGES |
|
|
Table1 Advantages and disadvantages of laparoscopic promontofixation
Conclusions
Laparoscopic promontofixation is a highly effective surgical technique for management of pelvis organ prolapse. The procedure shows successful outcomes in effectiveness and minimizes the risk of polypropylene mesh erosion. Promontofixation is now considered a gold standard treatment, and the further improvement and standardization of this method can make a significant contribution to minimally invasive gynecologic surgery and urogynecology. The use of the 3D imagining system certainly facilitates the procedure performance, reduces the operative time and minimizes the risk of complications
Author
Tomasz Kluz, MD, PhD, Provincial Consultant for Gynecologic Oncology, specialist in gynecology and obstetrics and specialist in gynecologic oncology.
- Content Type