Professor Naohisa Yahagi
Cancer Center, Keio University Hospital
RDI improves visibility of bleeding points which are difficult to observe under WLI
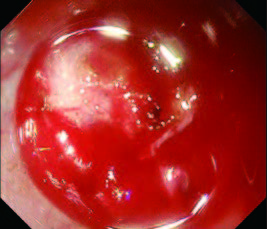
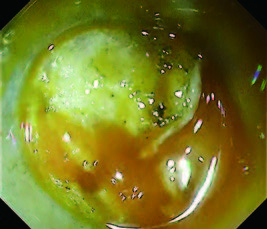
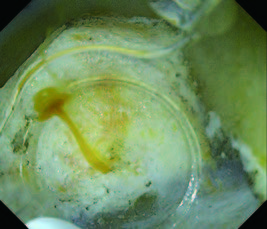
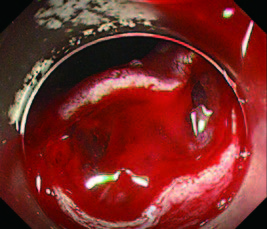
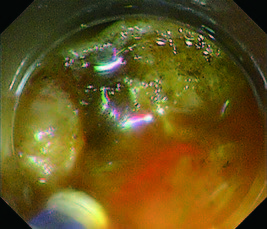
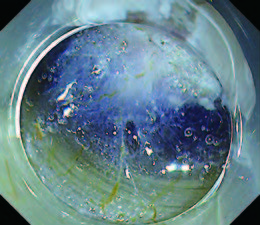
Identification of bleeding points is often difficult when there is excessive bleeding during endoscopic submucosal dissection (ESD), because the entire monitor view turns red and visibility is decreased under white light imaging (WLI). Under such circumstances, the difficulty of precise hemostasis, using high-frequency hemostatic forceps, can cause prolonged treatment time and an increase in the perforation risk due to hypercoagulation. However, even in cases where the bleeding points are obscure, RDI provides the enhanced detection of bleeding points by showing them with a darker, amber color (due the high hemoglobin concentration) (Figs. 1a,b).
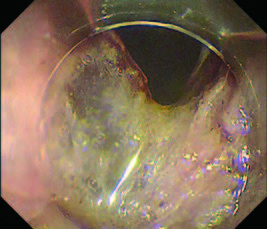
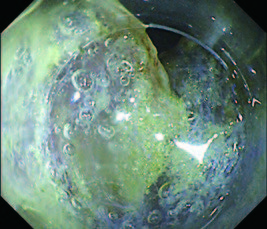
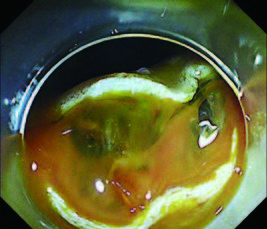
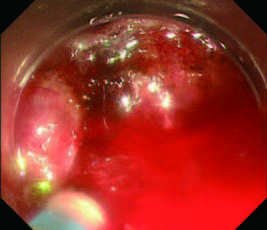
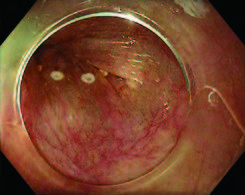
In cases of ESD on the greater curvature of the stomach and the ileocecum, abundant adipose tissues obscures the visibility of blood vessels. Furthermore, lipids from dissected adipose tissues scatter around and adhere on the endoscopic lens, which causes further reduction of visual field and the difficulty in manipulation (Fig. 2a).
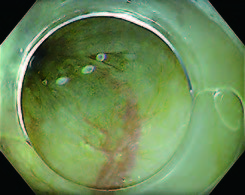
In such difficult conditions, it becomes more difficult to dissect and achieve hemostasis, which may cause not only longer procedure time but also lead to serious situations in the worst case. However, RDI makes adipose tissues less noticeable and visual field clearer, which results in a smoother procedure (Fig. 2b).
Fig. 1 Visibility of the bleeding point under WLI (a) and RDI (b)
Fig. 2 Visual field comparison under WLI (a) and RDI (b) with lipid adhesion on the lens
RDI allows us to select appropriate hemostasis treatment by providing easy assessment of bleeding status
At our medical center (Keio University Hospital Cancer Center), we generally use WLI for performing ESD and switch to RDI mode 1 when bleeding occurs. Under RDI, both the bleeding point and degree of bleeding can be easily assessed thanks to the image processing technology which visualizes the hemoglobin concentration using different tones of amber color. When the entire monitor view appears red due to bleeding, assessment of the bleeding status is difficult under WLI. However, switching to RDI mode enables us to recognize the degree of bleeding and to select the appropriate way of hemostasis.
We continue ESD without performing hemostasis when the bleeding is identified as a microbleed under RDI. In cases of mild bleeding, such as an oozing hemorrhage from a vein or bleeding from a small artery (Fig. 3a), we perform contact coagulation with a retracted knife tip (DualKnife J) instead of conventional hemostasis with hemostatic forceps (Figs. 3a,b). In cases of moderate to severe bleedings, such as a spurting hemorrhage from a large artery, observations of the bleeding point are even more difficult under conventional WLI, because the monitor view instantly turns red. Aspiration and irrigation are not effective to identify the bleeding point in such situations (Fig. 4a). Under RDI, bleeding points appear dark amber color during aspiration and irrigation, which makes them easy to be identified (Fig. 4b).
Fig. 3 Visibility of the degree of bleeding under RDI
(a) An example of mild bleeding which can be treated with a retracted knife tip
(b) Hemostasis by contact coagulation with a retracted knife tip
Fig. 4 Visual field comparison under WLI (a) and RDI (b) in a case of moderate bleeding
However, observing the bleeding point is difficult even after switching to RDI mode when a large amount of blood has accumulated. In such cases, aspiration is performed after switching to RDI mode, and the endoscope is pulled slightly back to gain a distant view of the entire treatment area for the overview. After checking the approximate location of the bleeding point, we approach and irrigate around that point. The bleeding point can be accurately identified during irrigation because fresh blood appears as dark amber under RDI. Especially in areas where water has accumulated, identification of the bleeding point is difficult under conventional WLI because the entire area turns red again after washing. Even in such situations, RDI visualizes the bleeding point as amber color and makes hemostasis easier (Figs. 5a,b).
Fig. 5 Visual field comparison under WLI (a) and RDI (b) with water accumulation
Improvement of visibility under RDI: use of indigo carmine and hemostasis tips
At our medical center, we use a local injection of agent containing a relatively high concentration of indigo carmine to clearly delineate the boundary between the muscular and submucosal layers. Specifically, we add 0.5 to 0.7 ml of indigo carmine to 200 ml of glycerol. In some cases of blood vessel-rich and adipose tissue-rich area, we perform dissection under RDI mode 1. In our experience, the addition of indigo carmine to the local injection agent is effective to improve the visibility of the submucosa in this mode, even though RDI exhibits flat images with weak three-dimensionality due to a different color tone presentation from that under WLI (Fig. 6). While there is an opinion that staining with indigo carmine may obscure small blood vessels, we believe this is not a problem when performing dissection with an electrosurgical knife. It is because bleedings from small blood vessels are often heat-coagulated during dissection. In addition, taking advantage of the improved visibility of blood vessels through the mucosal sur face under RDI, we use this mode to prevent bleeding during puncture with a local injection needle in some cases (Figs. 7a,b).
One useful hemostasis tip is to gaze at the bleeding point continuously once it has been identified regardless of RDI use. It is important to initiate hemostasis immediately after identification of bleeding point. For this purpose, we need maintain focus on the monitor to keep the bleeding point in view during manipulation of the endoscope, insertion of hemostatic forceps, and use of the foot switch.
Even if you promptly identify the bleeding point under RDI, moving your line of sight to the forceps port or foot switch at the time of transition to hemostasis often causes the movement of endoscope and the shift of monitor view simultaneously. The shift of bleeding point from the monitor view requires additional time to reidentify the bleeding point.
Because how to use the foot switch is key to keep on looking at the monitor, we recommend checking the position of the foot switch in advance and planting your heel onto the ground to use as a pivot point during operation.
Fig. 6 Visibility of the muscular and submucosal layers under RDI with a local injection agent containing indigo carmine
Fig. 7 Visibility of blood vessels through the mucosal surface under WLI (a) and RDI (b). The superficial capillaries became indistinct and the thicker deep blood vessels became clearly visible under RDI
Validation of effectiveness of RDI by a multicenter RCT: Reduction in stress of operators
A multicenter randomized controlled trial (RCT) was conducted on the effectiveness of RDI in ESD. We compared outcomes such as hemostasis time, treatment time, and operator stress between observation under WLI and RDI to determine the effectiveness of RDI. Approximately 400 cases of ESD for esophageal, gastric, and colorectal lesions from seven facilities were randomly assigned to either the WLI group or the RDI group. There was no significant difference in hemostasis and treatment times between the two groups. However, when we analyzed the data from the RCT, we found that the number of performed hemostasis was significantly lower in the RDI group than that in the WLI group. We assume that this would reflect that the operators continued ESD without performing hemostasis in many cases because the bleeding condition could be monitored under RDI, and the operators did not mind slight bleeding under RDI. If we compared cases of moderate or severe bleedings which required hemostasis with hemostatic forceps, we would obtain different results in terms of the effect on hemostasis time.
In contrast, operator stress level was significantly lower in the RDI group than that in the WLI group with a five-level evaluation. The heart rate of the operators at our medical center during endoscopic treatment was measured before and after bleeding, and the results showed that the heart rate increased after bleeding in approximately 80% of the operators, indicating that psychological stress is felt when the entire monitor view turns red due to bleeding. We believe that visualizing hemorrhages in amber color instead of red decreases the sense of urgency and stress of operators towards bleeding, which allows operators to identify the bleeding point and perform hemostasis in a composed manner.
Possibilities that the EVIS X1 advances the efficiency and quality of endoscopic diagnosis and treatment
Although no significant difference was shown in the RCT that verified the effectiveness of RDI, we have an impression that the use of RDI helps reduction of hemostasis and treatment times. With the experiences of RDI for hemostasis treatment of gastrointestinal bleeding and diagnosis or treatment of esophageal varices in our medical center, I have been seeing the benefits of RDI use in the other cases from ESD.
With the aim of improving observation performance, the EVIS X1 series not only incorporates new image processing technologies such as TXI and EDOF, but also enhances the brightness and clarity of the images. We believe that this may lead to a higher accuracy of the lesion detection and qualitative diagnosis during screening tests. We expect that the efficiency and quality of endoscopic diagnosis and treatment are advanced using the multiple functions of the EVIS X1, including RDI.