Dr. Tsuneo Oyama
Department of Endoscopy, Saku Central Hospital Advanced Care Center
Endoscopic submucosal dissection (ESD) is a minimally invasive treatment for early gastrointestinal cancer. This procedure needs to be performed safely and reliably to avoid procedural accidents such as perforation. It is crucial to select the most suitable device from various types of high-frequency knives and employ a technique that makes full use of its features. Dr. Tsuneo Oyama from Saku Central Hospital was involved in the development of HookKnife, characterized in an L-shaped hook with rotating function. He has been working to promote ESD techniques using this device. Recently Dr. Oyama was involved in the development of HookKnife J with an added water jet function. We asked him about the usefulness of this device and the expectations on changes for techniques employed in ESD.
Feasibility of safe and efficient incision and dissection utilizing the L-shaped hook and the rotating function of HookKnife.
Key features of HookKnife and tips for using the device
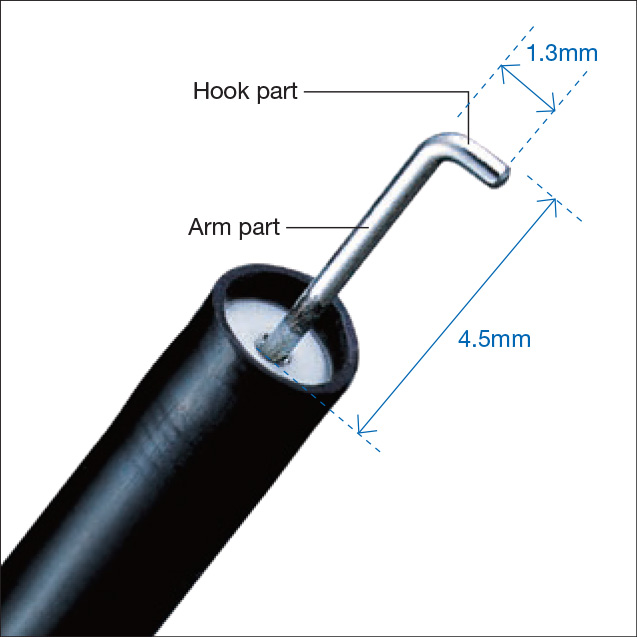
HookKnife is a high-frequency knife used for mucosal incision and submucosal dissection in ESD. Those procedures are conducted by hooking and pulling the mucosa or submucosa with the distal L-shaped hook (Fig. 1), and powering the device. When so-called pointed tip-type knives are used, incisions are made by pressing the knife tip against the tissue and powering the device. Thus, there may be a greater risk of damaging the deep muscle layer, which can result in perforation. In contrast, when using HookKnife, with the tip of the hook turned to the desired direction, the hook is inserted into the tissue in the direction parallel to the muscle layer, then the tissue is cut by pulling the hook towards the inner cavity and powering the device.
Provided the basic procedures are followed, such as hooking the submucosal blood vessels or fibers under direct vision, then powering the device to cut them, the device will enable very safe incision and dissection. A knife such as this, which hooks and pulls the tissues, then applies energy, is highly suitable for safely cutting or dissecting a very thin mucosa or submucosa of the gastrointestinal wall, which is influenced by respiratory variation. Additionally, if it is possible to approach the lesion in parallel to the muscularis propria, the knife enables efficient dissection using the arm part.
Tips for rotating the L-shaped hook
The distal L-shaped hook of HookKnife is composed of a 1.3-mm hook part and a 4.5-mm arm part (Fig. 1). When the assistant turns the handle, the hook part can rotate to the same angle (Fig. 2). Sometimes the rotation of the handle may not transfer well to the knife tip. In such a case, rotating the handle with repeated back and forth manipulation of the slider leads to release the resistance and allow the hook part to be rotated in the desired direction.
Types of approach and procedure using HookKnife depending on lesion orientation
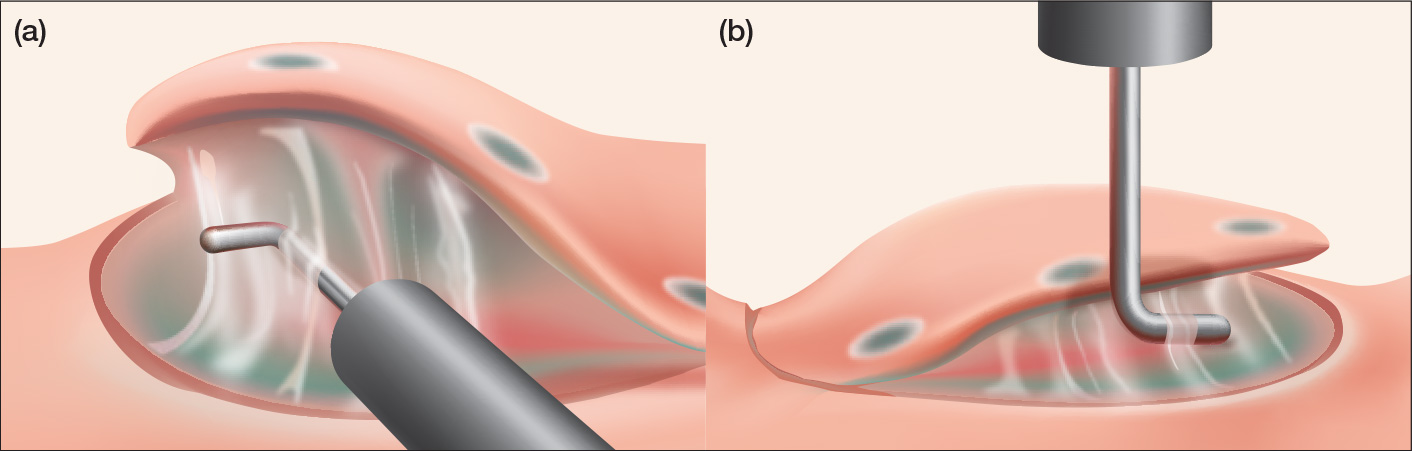
If the lesion can be approached tangentially, the hook part can be turned parallel to the muscularis propria. HookKnife can then be inserted into the submucosal layer and manipulated in parallel with the muscularis propria, enabling efficient incision and dissection (Fig. 3a). Since esophageal lesions will always be approached tangentially, incision or dissection using the arm part of HookKnife is particularly useful.
Compared with knives which can perform sequential incision and dissection, HookKnife may be disadvantageous in some situations in terms of speed. However, where the lesion orientation is favorable, providing traction to the tissue by using the tip attachment may enable efficient dissection by utilizing the long 4.5-mm arm part.
Meanwhile, with respect to the lesion that cannot be approached tangentially and should be approached frontally even though the scope is reversed, short incisions and dissections are made repeatedly after catching small amounts of tissues with the hook part (Fig. 3b). Though incision and dissection with the shorter hook part is less efficient than that with the arm part, one of the major advantages of HookKnife would be that even in case of a frontal approach, it can incise and dissect lesions in the duodenum and colorectum having a strongly curved narrow cavity.
Incision and dissection in difficult lesions, and hemostasis of exposed blood vessels using HookKnife
In cases of ulcer scars or recurrence from a remnant lesion, it may be difficult to achieve sufficient submucosal elevation due to narrowing caused by severe fibrosis of the submucosa, which generally makes it difficult to perform dissection. Even in this situation, dissection can be performed provided HookKnife is used correctly. If the lesion can be approached tangentially, first the surrounding submucosa with mild fibrosis is dissected to confirm the boundary of the muscle layer. Although fibrosis of the central part of the scar is too severe to confirm the boundary of muscularis propria, dissection can be continued using the arm part, leading to connect the exposed boundary of muscularis propria on both lateral sides of the scar. Similar dissection steps are performed in case of fibrotic lesion which can only be approached frontally. After confirming the boundary of muscularis propria in the surrounding area where the fibrosis is milder, short dissections are repeated in small chunks using the hook part.
HookKnife is also useful for preventative pre-cut coagulation of the exposed blood vessels. For veins narrower than the length of the hook part (1.3 mm), both sides of the vessel wall are caught one by one with the hook part and subsequently coagulated by applying low voltage energy to stop the blood flow. For veins that are wider than 1.3 mm, or arteries with thicker walls, where it might be difficult to achieve sufficient coagulation, pre-cut coagulation is performed using Coagrasper (highfrequency hemostatic forceps).
HookKnife J with an added water jet function enabling injection of solution into the submucosa
HookKnife is a very safe and versatile device among the pointed tip-type knives. As a new line-up of the device, HookKnife J has been developed by adding waterjet function from the sheath. With this feature, in case that additional submucosal elevation is required during incision and dissection, solution can be injected into the submucosa from the nozzle at the tip of the device without switching from the knife to an injection needle.
Issues to be addressed during ESD when using HookKnife and their solutions
In conventional ESD techniques, safety during incision and dissection was secured by submucosal elevation using local injection needles. However, the injected fluid would soon disperse with the reduction of submucosal elevation, thus, the step of additional needle insertions and injections is required. Therefore, it was unavoidable to bear the burden of switching to another device, resulting in prolonged duration of procedure. In addition, since local injections involved the use of sharp needle points, insertion into the submucosa would cause hemorrhage, and often resulted in reduced visibility of the operative field. In some instances, this led to the creation of a vicious circle, where an additional local injection just after the hemostasis by Coagrasper would cause another hemorrhage, followed by reusing Coagrasper to stop bleeding. Therefore, in order to avoid hemorrhage we have been performing local injections into the submucosa by pressing the sheath tip with the needle being retracted into the sheath to avoid hemorrhage. Furthermore, we have been attempting to secure a good operative field of view by checking the blood vessels before making an incision, and proceeding with the dissection while performing pre-cut coagulation as frequently as possible using HookKnife and Coagrasper.
Improving the safety and efficiency of incisions and dissections by using knife injection for creating additional submucosal elevation
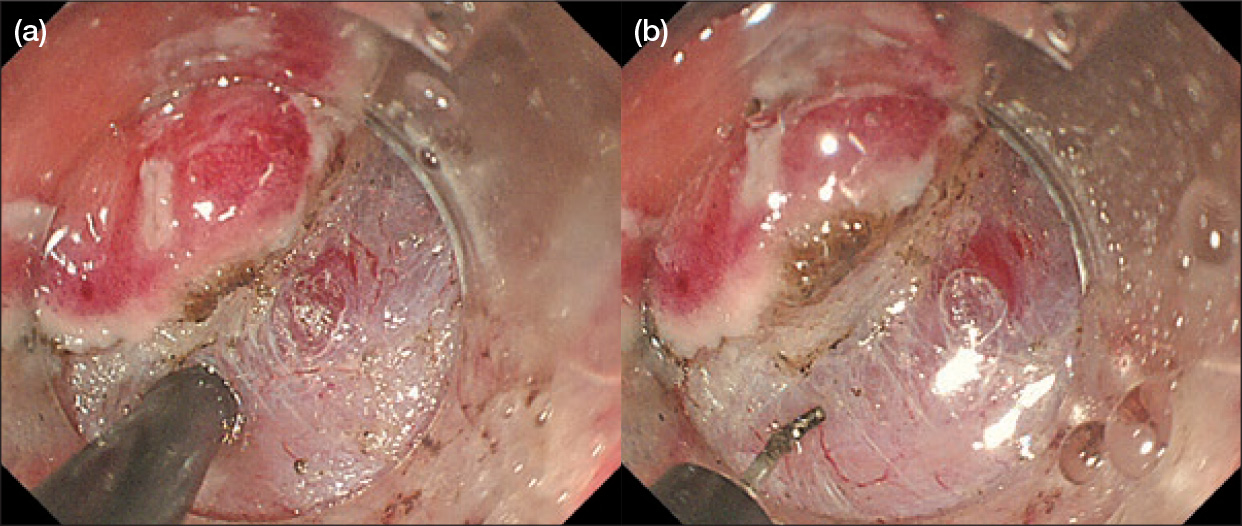
When the newly developed HookKnife J is used, not only is it possible to inject solution into the submucosa, additional injections can also be made from the mucosa by pressing the sheath tip against the marking point. This minimizes hemorrhage during local injection, and makes the development of hematoma in the submucosa extremely rare. In addition, since it is no longer necessary to switch from the knife to an injection needle, procedures can be completed more quickly. Moreover, the device makes it much easier to create additional submucosal elevation during the procedure as needed (Fig. 4a), which improves safety during incision and dissection.
Particularly if a surgeon has limited experience in ESD techniques, the sequence of procedure may often take 2 or 3 minutes from removing the knife to inserting the needle, additional injections, removing the needle and re-inserting the knife. In that time, the additional submucosal elevation would have flattened down again, thus, it would be difficult to incise and dissect under favorable conditions. However, I consider HookKnife J an extremely useful knife because incision and dissection can be resumed with it immediately after creating the submucosal elevation (Fig. 4b).
Tips for injecting solution into the submucosa with HookKnife J
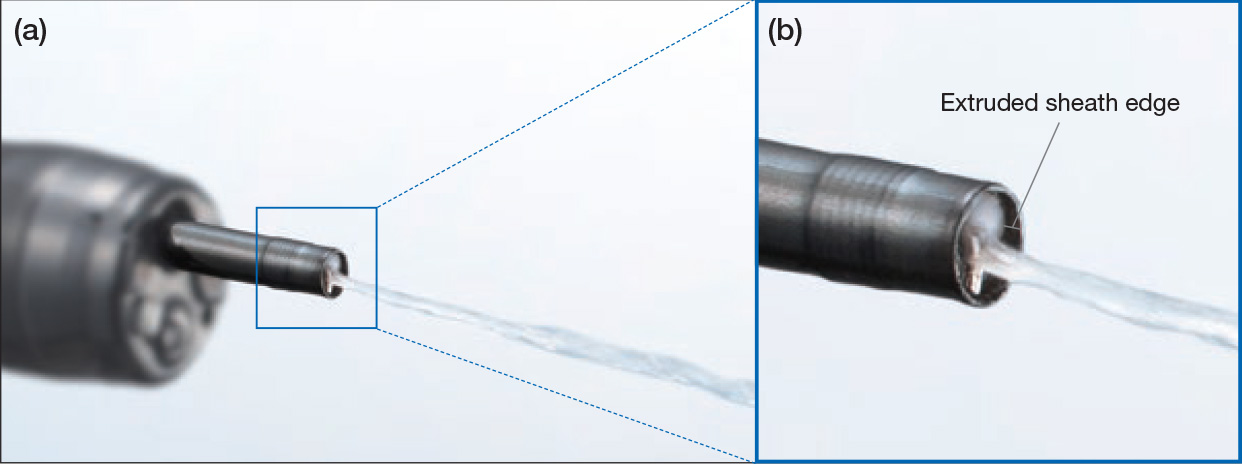
In order to inject solution into the submucosa with HookKnife J safely and reliably, first the L-shaped hook should be kept retracted into the sheath to avoid the risk of perforation (Fig. 5a). To perform the local injection smoothly and create favorable submucosal elevation, it is very important to distinguish the sparse tissues deep within the submucosa to inject into, which can be seen through immediately above the muscle layer. We note that if the tip is pressed against the fibrous layer of white appearance or the yellow fatty layer, the solution would not be injected into the submucosa.
Additionally, as a tip for injecting solution, a short extruded black sheath of HookKnife J (Fig. 5b) can be used as a hood during injection. By injecting solution while the black sheath is pressed against the mucosal surface, knife injection can be performed efficiently without causing backflow, keeping the operative field dry. The amount of solution injected from the knife per shot is 0.5 to 1 cc.
Useful water jet function for cleaning and removing debris from the knife
The water jet function of HookKnife J is also useful for removing tissue fragments and blood clots that build up on the L-shaped hook as the procedure progresses. When we perform incision and dissection in operative fields particularly where there is heavy bleeding, dirt tends to build up on the knife, causing a reduction in the ability to incise. In the case of HookKnife, the knife needs to be removed to clean the L-shaped hook. However, when using HookKnife J, in addition to repeated movement of the handle slider back and forth, the water jet can be used to easily clean and remove debris from the hook. Since the nozzle is designed so that solution can be expelled through 360° around the arm part of the L-shaped hook, it enables efficient cleaning and removal of debris.
How HookKnife J will change ESD
Lesion resection strategies
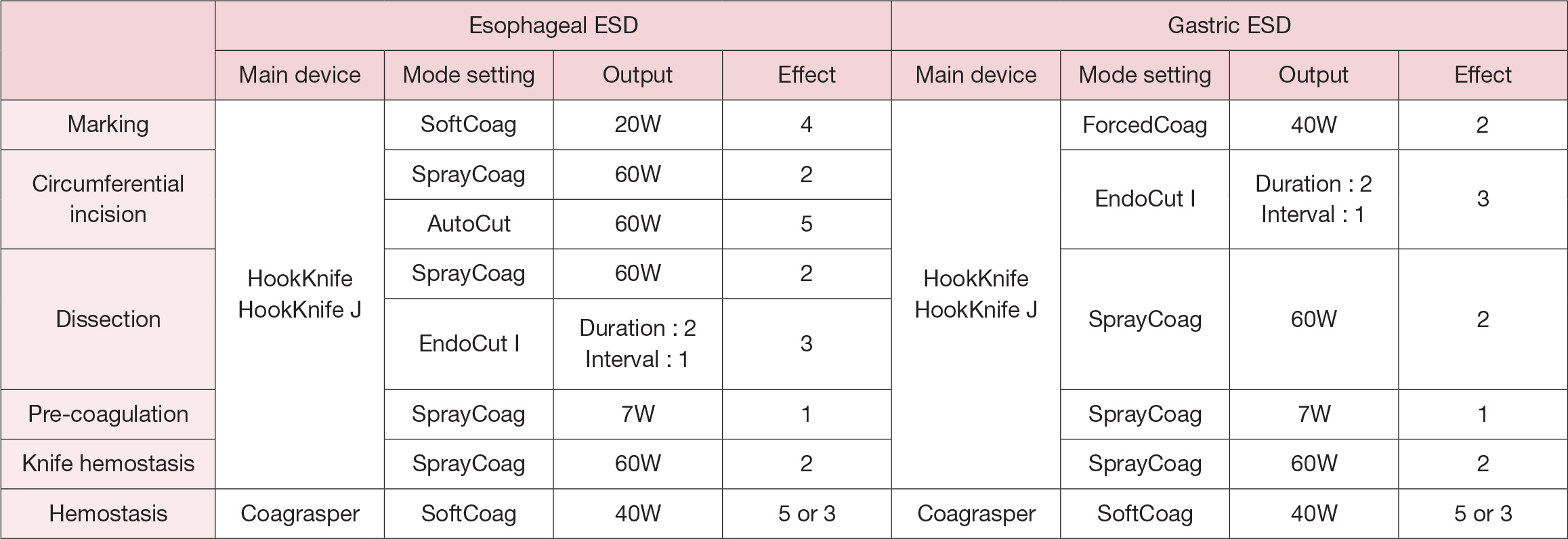
When the water jet function was added to HookKnife J, two aspects were emphasized in the development of the device: first, to retain the rotating function, shape and size of the L-shaped hook and second, not to increase the maximum diameter of the insertion part. HookKnife J meets both requirements, and in practice, the operability and usability of the device seem unchanged. There has also been no change in the output and mode settings of the high-frequency generator (Table 1).
[Table 1] High-frequency settings of HookKnife series during esophageal or gastric ESD (when using VIO300D)
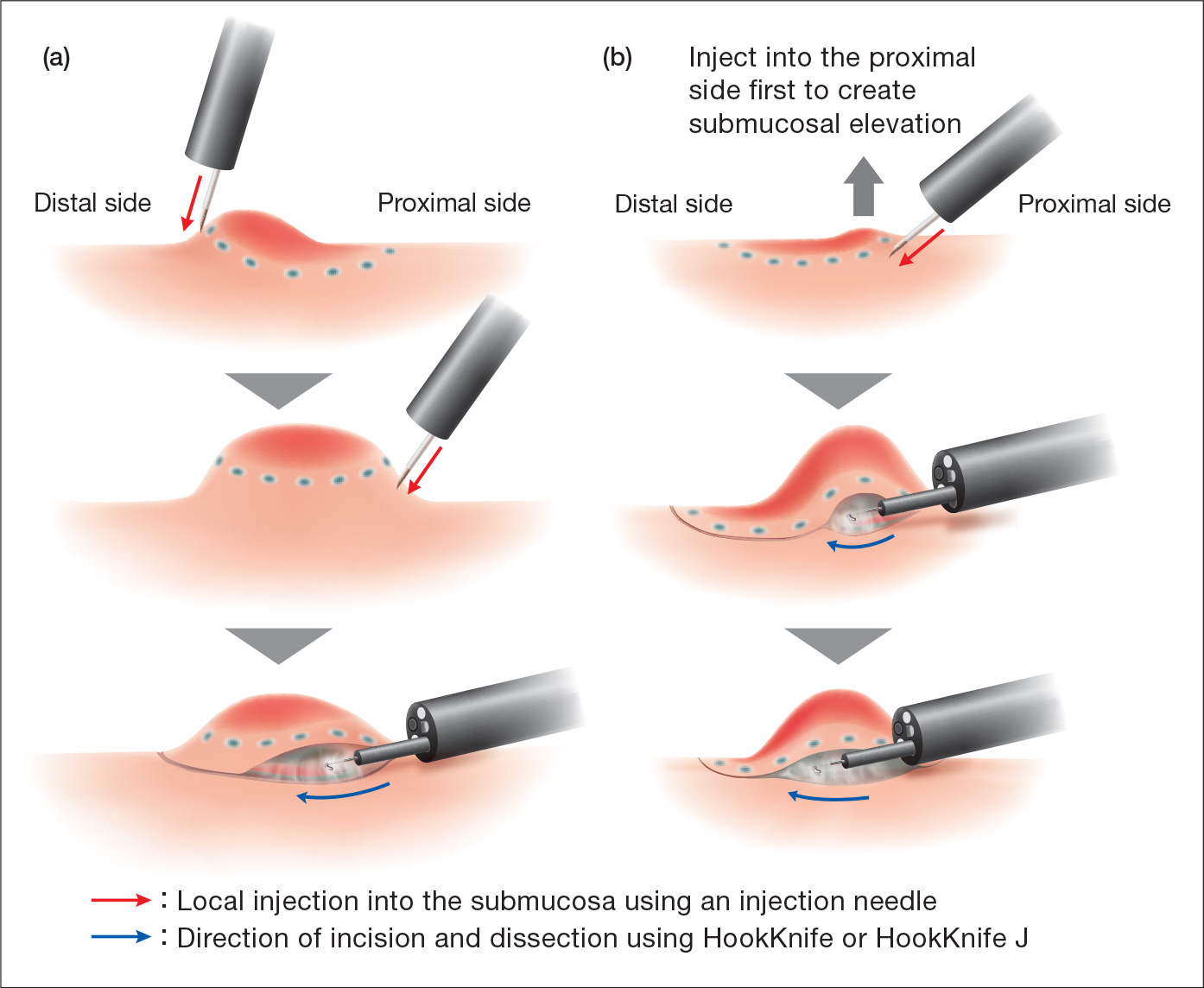
Meanwhile, there has been a dramatic change in the strategies for the starting positions of local injection, mucosal incision and submucosal dissection, made possible by HookKnife J’s new ability to create additional submucosal elevation with knife injection (Fig. 6). In the past, submucosal elevation had to be created by inserting an injection needle into several points from the distal to the proximal side, before the tissue could be incised and dissected from the proximal towards the distal side (Fig. 6a). With HookKnife J, an initial local injection is performed on the proximal side, and mucosal incision and submucosal dissection can be continued while giving additional local injections into the submucosa whenever necessary (Fig. 6b).
Moreover, if necessary, additional local injections can be performed from the mucosal surface. In such cases, HookKnife J is placed against the mucosa with the L-shaped hook retracted, and solution is injected after cauterizing the mucosa with coagulating current. However, a local injection using an injection needle is necessary for lesions with severe fibrosis.
Coordination between surgeons and assistants
Since precise rotating operation is essential for safe incision and dissection in using HookKnife, good coordination between surgeons and assistants is crucial. In the newly developed HookKnife J, with the added water jet function, the injection syringe should be operated simultaneously by one hand with the other holding a handle. This requires even closer coordination between surgeons and assistants.
However, I think assistants will enjoy working in unison with surgeons to proceed the operation.
“The content of this article may contain off-label information”
Introduction of facilities
Saku Central Hospital Advanced Care Center,
Nagano Prefectural Federation of Agricultural Cooperatives for Health and Welfare
With a history spanning more than 70 years, Saku Central Hospital has been providing community-centered healthcare as the flagship hospital for the Eastern district of Nagano Prefecture. Saku Central Hospital Advanced Care Center, established in 2014, specializes in acute phase medicine. The Yatsugatake Gastric Disease Research Group, founded by Dr. Oyama in 1992 to examine cases of gastric disorders beyond the boundary between internal medicine and surgery, led to the creation of a regional medical cooperation for ESD. The Center now accepts ESD patients referred from Nagano Prefecture and surrounding regions. Currently, it performs approximately 60 to 70 ESDs for esophagus, more than 100 ESDs for stomach, and 60 to 70 ESDs for colorectum annually.
- Content Type