Dr. Yutaka Saito,
Director of the Endoscopy Division, National Cancer Center Hospital
The combination of the EVIS X1 and CF-EZ1500D with its improvements in image quality is expected to increase the adenoma detection rate during colorectal cancer screening
Recently, the adenoma detection rate (ADR) has been proposed as a quality indicator in screening colonoscopy1). Although the ADR depends on the purpose of endoscopic examination and have been varied among endoscopists and hospitals, it was reported that each 1.0% increase in the ADR was associated with a 3% decrease in the risk of interval cancer and post-colonoscopy colorectal cancer2). Thus, an increase in the ADR is one of the most important outcomes of colorectal cancer screening.
Accurate detection of diminutive colorectal lesions, such as lesions of the superficial depressed type (type 0-IIc), is a major factor in increasing the ADR. Thus, we defined flat adenoma detection rate (FDR) and depressed adenoma detection rate (DDR)3) as indicators of minute lesion detection and intend to broadly introduce their importance, with the aim of increasing the ADR. In my experience, the newly released advanced endoscopy system, EVIS X1, and video colonoscope, CF-EZ1500D, provide clearer and higher-quality images than previous models. It is expected that the introduction of these products will increase the ADR, particularly the FDR and/or DDR.
The red color tone enhancement of the mucosal surface under TXI will enable more accurate detection of colorectal lesions
In endoscopic examinations for colorectal cancer screening, white light imaging (WLI) is the conventional method by which most early colorectal cancers can be detected. However, in some cases, lesions with subtle changes in color and shape are difficult to detect. Recently, the effectiveness of narrow band imaging (NBI) for colorectal lesion detection has been demonstrated, and the application of NBI for screening examinations is becoming more prevalent. In addition to NBI, the new model, EVIS X1, is equipped with the latest technologies such as texture and color enhancement imaging (TXI) and extended depth of field (EDOF)†. The new image processing technology TXI was developed to improve observation performance, and EDOF enables easy focusing during magnifying observations.
TXI, a texture and color enhancement function, processes and optimizes three elements of the mucosal surface image under WLI: “texture”, “color tone”, and “brightness”. Lesion visibility of endoscopic images under TXI will be improved by the enhancement of subtle differences in texture and color4).
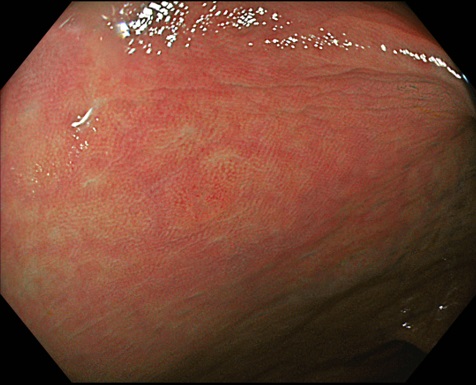
An important aspect of colonoscopy is the ability to detect lesions with increased microvascular density, a common distinctive appearance of tumors. Pale redness of the mucosal surface and disappearance of vascular patterns are important mucosal findings for the detection of colorectal lesions during WLI observation. The red color tone of TXI is more enhanced compared with that under WLI. I assume that use of TXI results in an increase in the ADR, since it enables clear recognition of pale redness. In our experience, soon after we started using the EVIS X1, TXI enabled the detection of 1-2mm type 0-IIc lesions in two successive cases (Fig. 1). It would have been difficult to detect the lesions in both cases if only conventional observations under WLI were available.
† Available in the combination of the EVIS X1 and GIF-EZ1500 or CF-EZ1500D series.
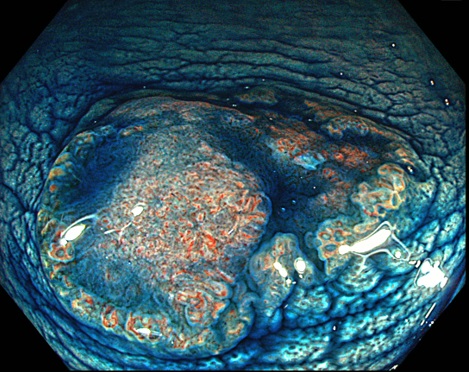
<Fig. 1> Endoscopic images of a 1.5mm type 0-IIc lesion located in the transverse colon under TXI mode 1 before (a) and after (b) indigo carmine dye spraying.
TXI mode 1 shows greater enhancement of red color tone, and the color tone of TXI mode 2 is similar to that of WLI
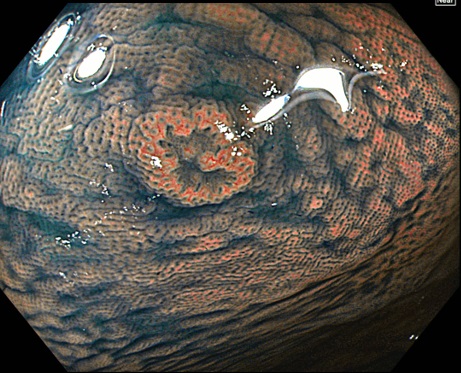
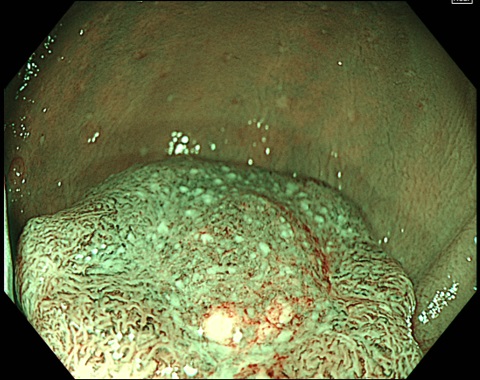
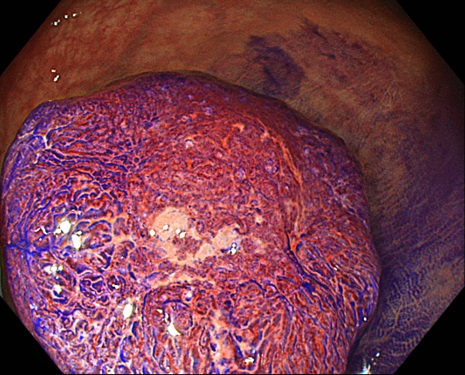
TXI has two modes, modes 1 and 2 (Fig. 2b, c). Mode 2 provides optimized images with texture and brightness while the color tone is similar to that of WLI. Alternatively, mode 1 appears to enhance the red color tone of the mucosa to a greater extent than mode 2. The selection of these two modes depends on the preference of each endoscopist using the EVIS X1. Mode 2 may be more convenient for endoscopists who are accustomed to diagnoses using conventional WLI images.
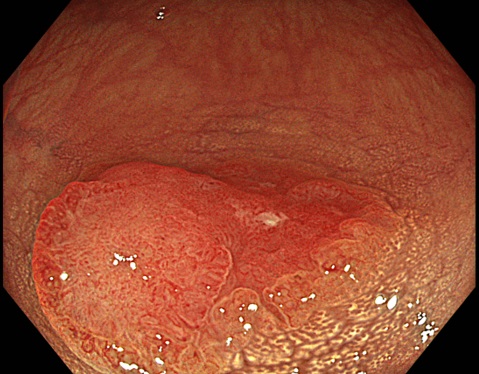
During the detection of colorectal lesions at our hospital, all four modalities (WLI, TXI mode 1, TXI mode 2, and NBI) are currently used to examine the appearance of each lesion, particularly the type 0-IIc (Fig. 1), superficial elevated type (type 0-IIa, Fig. 2), and sessile serrated lesions. As more users utilize these technologies and accumulate evidence, we can establish an optimized selection of observation modes for more accurate detection of lesions. In addition, a concern is that the differentiation between inflammation and tumors may be difficult in certain cases under TXI mode 1 due to the strong enhancement of the red color. This may be an issue for future consideration.
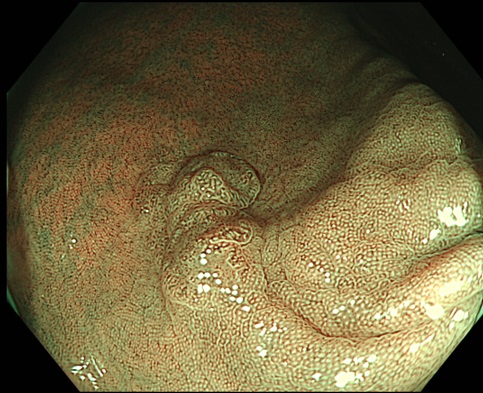
<Fig. 2> Endoscopic images of a 10mm type 0-IIa+IIc lesion in the cecum The demarcation line and depressed shape under WLI (a) is sharpened by switching to TXI mode 1 (b). TXI mode 2 also shows a demarcation line and surface pattern similar to that of mode 1 (c). The lesion is identified as an O-ring sign under NBI (d).
The incorporation of the Dual Focus function and EDOF technology enables easier focus adjustment during magnifying observation by using the combination of the EVIS X1 and CF-EZ1500D.
EDOF, an extended depth of field function of the EVIS X1, is available in combination with the CF-EZ1500D video colonoscope. This technology projects two images that focus on near and far points and combines them into one image in real time. The obtained image has a wide observation depth which enables far and near points to be in focus. CF-EZ1500D is equipped with the Dual Focus function that enables switching from the Normal mode (for middle to long distance views) to the Near mode (for close-up magnification), with one push of a button. The combination of these two functions will allow easier focus adjustment for magnifying observations compared with that of the conventional manual zoom models and also with that of other Dual Focus function models.
Experts in magnifying observation procedures can steadily observe lesions in the frontal view even in cases where focusing is difficult, such as for tangential approaches to lesions. CF-EZ1500D provides easier focus adjustment that is useful particularly for non-experts who have not yet mastered such techniques. Quick focusing will reduce the time not only for examination but also for non-experts’ learning curve for magnifying observation. We hope that the combination of the EVIS X1 and CF-EZ1500D will lead to widespread use of magnifying observation procedures.
Wide observation depth provided by EDOF will enable detailed evaluation of lesions using magnifying observation with CF-EZ1500D at a level that is equivalent to that of manual zoom scopes
EDOF will be beneficial, particularly for the observation of tumorous lesions. Because tumors generally have irregular and uneven mucosal surfaces, only part of the lesion can be focused on at a shallow depth of field. The overall image of the lesion can be observed in focus using the CF-EZ1500D that is equipped with EDOF, which will enable a more detailed evaluation to narrow down the region of interest in magnifying observations.
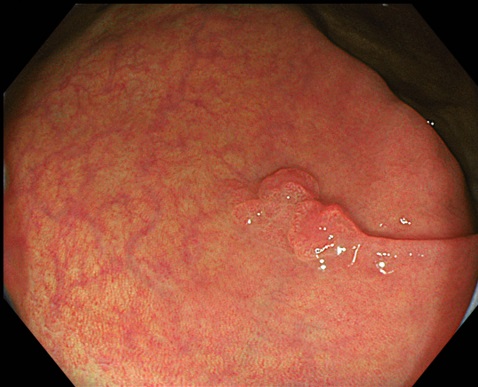
In practice, in pit pattern observation, lesions with highly irregular VI pit pattern are often difficult to evaluate with Near mode in previous Dual Focus function models. However, we have an impression that the Near mode of CF-EZ1500D can exhibit as good image quality as magnifying observations with manual zoom scopes, which helps us evaluate lesion in these difficult cases. Similarly, in magnifying observations under NBI, surface and vessel patterns can be observed very clearly in the Near mode with the CF-EZ1500D (Fig. 3a). These impressions suggest that the magnifying observation with CF-EZ1500D exhibits diagnostic accuracy equivalent to that of the manual zoom scopes in diagnoses based on the JNET classification5-7).
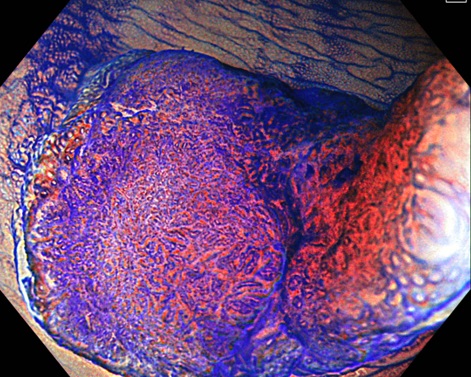
<Fig. 3> Endoscopic images of a node in Near mode using CF-EZ1500D The vessel and surface patterns at the top of the node have been disturbed and are considered to correspond with Type 3 in the JNET classification (a). Magnifying chromoendoscopy with crystal violet staining under TXI mode 2 visualized highly irregular VI pit pattern (invasive pattern) and a partial type VN pit pattern (b).
Chromoendoscopy under TXI will enable clear visualization of the pit pattern
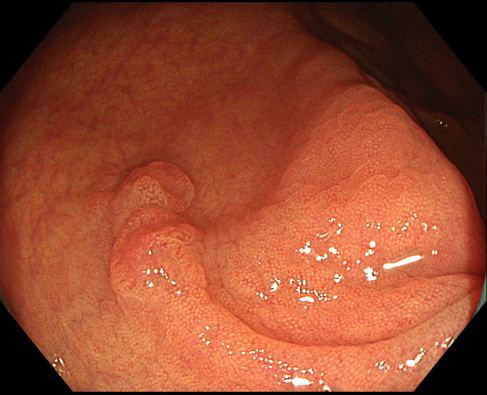
Chromoendoscopy under TXI with CF-EZ1500D will visualize the pit pattern more clearly with the enhancement of texture (Figs. 3 and 4).
For example, switching from WLI to TXI may be helpful for the evaluation of type V pit patterns in cases where the pattern is not clearly obtained with crystal violet staining in the CF-EZ1500D Near mode (Fig. 3b).
Alternatively, when chromoendoscopy with indigo carmine dye spraying is used for the diagnosis of lateral extension prior to endoscopic submucosal dissection or endoscopic mucosal resection, switching from WLI to TXI will lead to a more accurate pit pattern diagnosis (Fig. 4b). Therefore, chromoendoscopy under TXI will advance the accuracy of qualitative and quantitative diagnoses in various cases.
<Fig. 4> Diagnosis under TXI before endoscopic treatment TXI mode 2 clearly visualized the boundary of the depressed structure (a), and the unevenness of the lesion surface, including the elevated part surrounded by the depressed structure, which is enhanced by indigo carmine dye spraying (b). The Near mode under TXI mode 1 visualized highly irregular VI pit pattern (invasive pattern) after crystal violet staining (c).
1) Rex DK, et al. Am J Gastroenterol. 2006; 101: 873-885.
2) Corley DA, et al. N Engl J Med. 2014; 370: 1298-1306.
3) Saito Y, et al. Dig Endosc. 2021; 33: 486-519.
4) Sakamoto T, et al. Dig Endosc. 2023; 35: 529-537.
5) Sano Y, et al. Dig Endosc. 2016; 28: 526-533.
6) Iwatate M, et al. Dig Endosc. 2018; 30: 642-651.
7) Saito Y, et al. Dig Endosc. Epub ahead of print: [2023 Sep 13].