Hiroo Imazu, MD, PhD
Professor, Division of Gastroenterology and Hepatology, Department of Medicine, Nihon University School of Medicine
Academic/professional background:
1991 Graduated from Medical Program, Asahikawa Medical University
1991-2003 Third Department of Internal Medicine, Nara Medical University
2003-2004 Department of Interdisciplinary Endoscopy, University Hospital Hamburg-Eppendorf, Germany
2004-2017 Department of Endoscopy, Jikei University School of Medicine
2017- Division of Gastroenterology and Hepatology, Department of Medicine, Nihon University School of Medicine
This is a clinical study report using a prototype for validation with specifications equivalent to Single Use Sphincterotome V (Distal Wireguided) KD-VC433Q-0720.
I. Development of a novel cannulation catheter based on risk factors of post-ERCP pancreatitis
It has been reported that there are a wide range of significant risk factors associated with post-ERCP pancreatitis (PEP), such as age, female, SOD, PEP history, unintended pancreatic access with contrast or Guide-wire, endoscopic papillary balloon dilation (EPBD), difficult cannulation, precut and so on. The study at our institution also identified specific risk factors associated with PEP as the following: age of the patients under 50 years, EPBD, biliary stent placement, and pancreatography1). Theoretically, it might be possible to eliminate all operator-related factors such as unintended pancreatic access and difficult cannulation. Therefore, to prevent operator-related PEP, we developed a novel oblique-tip papillotome to facilitate biliary cannulation and reduce the incidence of unintended contrast injection or Guide-wire insertion into the pancreatic duct.
II. Concept of the oblique-tip papillotome
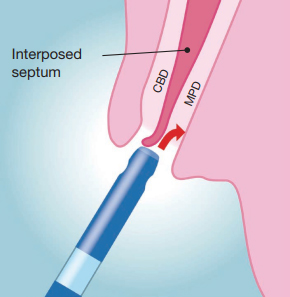
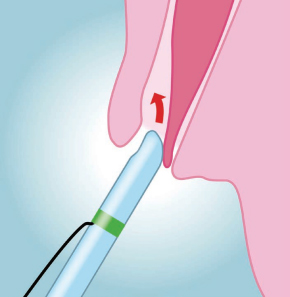
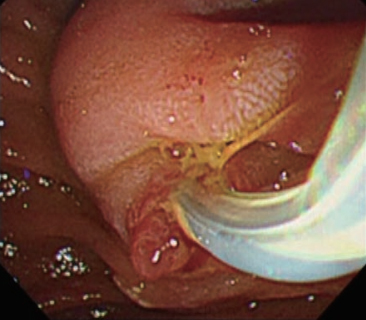
In pancreaticobiliary anatomy of papilla, the opening of the bile duct is usually separated from the pancreatic duct by a septum, and is located above the pancreatic duct 2). To cannulate the bile duct selectively, the catheter tip or Guide-wire should be advanced to the bile duct above the septum, aiming at the 11 o’clock position 3). Endoscopists will encounter cases in which cannulation of the pancreatic duct can be easily achieved but deep access to the bile duct remains elusive. In such cases, the tip of the catheter or Guide-wire may easily be advanced below the septum, i.e. to the direction of the pancreatic duct (Fig. 1). Based on this concept, we designed a novel 4.5Fr oblique-tip papillotome in order to facilitate biliary cannulation and reduce unintended contrast injection or Guide-wire insertion into the pancreatic duct. The tip of this new catheter was sharpened obliquely and circumferentially, and angled at approximately 40 degrees. Therefore, this modified tip can deflect the interposed septum downward and be aligned with the axis of the bile duct, allowing this new catheter to enter the bile duct preferentially (Figs. 2 & 3).
III. Results of pilot study using the oblique-tip papillotome
As a pilot study, we conducted a retrospective study to compare a novel oblique-tip papillotome (OT; n=40) with a standard 4Fr straight-tip catheter cohort (ST; n=45) 4). In order to compare the utility of the tip shape between the oblique-tip papillotome and the standard straight-tip catheter, we did not use the bow-up function of the oblique-tip papillotome in this pilot study. Although the biliary cannulation success rate, total procedure time, and PEP incidence rate were similar in both cohorts, the frequency of unintended contrast injection into the pancreatic duct and the time required for the OT cohort during biliary cannulation were significantly less than those of the ST cohort (0.56 vs. 1.65 times and 103.3 vs. 287.9 seconds). Thus, the new oblique-tip papillotome could facilitate biliary cannulation while reducing the unintended access to the pancreatic duct during ERCP. In addition, multicenter study with wire-guided cannulation (WGC) using the oblique-tip papillotome are ongoing, and early analysis shows the oblique-tip papillotome is useful in WGC.
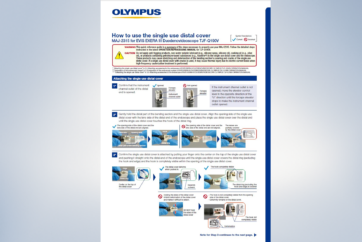
IV. How to use the oblique-tip papillotome in biliary cannulation
The oblique-tip papillotome could be used in almost the same way as the standard-tip catheter in selective biliary cannulation. The duodenoscope should be manipulated to position the papilla so that the direction of the oblique-tip papillotome matches the axis of the bile duct. Then, biliary cannulation should be attempted, giving attention to the septum between the opening of bile and pancreatic ducts, and the distal end of oblique-tip papillotome. As a result, selective biliary cannulation could be easily achieved as long as the distal end of oblique-tip is located above the septum, i.e. the opening of bile duct, even if the axis of papillotome itself is aligned with pancreatic duct (Fig. 2). In addition, a tiny groove is set on the distal end of oblique-tip to enable the tip to be hooked onto the opening of bile duct. This novel oblique-tip papillotome can be applied to both contrast-guided and wire-guided cannulation techniques, and bow-up function of papillotome is also available to direct the oblique-tip to the axis of bile duct.
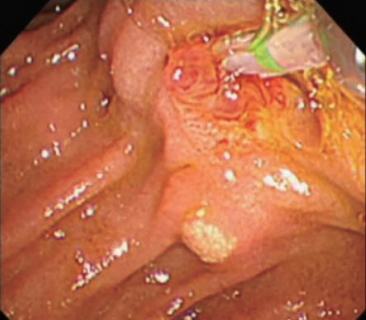
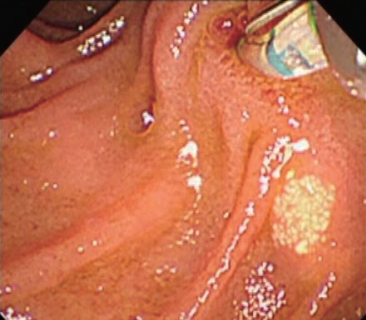
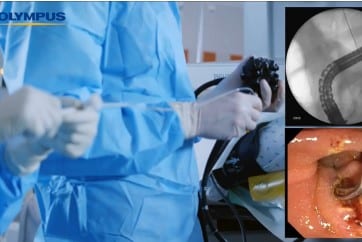
A representative case of biliary cannulation with the oblique-tip papillotome is shown in Figures 4, 5 and 6. Endoscopic finding showed a papilla with a tiny protrusion, which was regarded as one of the factors for difficulty in biliary cannulation. After obtaining an en face view of the papilla, the distal end of oblique-tip papillotome was placed at the opening of bile duct, while matching the axis of oblique-tip papillotome and bile duct (Fig. 4). Then, the oblique-tip papillotome was advanced toward the axis of bile duct, using upward angulation of duodenoscope (Fig. 5). Finally, biliary cannulation was easily achieved without unintended pancreatic access (Fig. 6).
V. Conclusion
Biliary cannulation is the first step in all ERCP-related procedures. Any troubles at this first step might not only prolong the procedure time but also increase the likelihood of complications such as PEP. We believe that the use of oblique-tip papillotome in biliary cannulation can make ERCP procedures safer and more effective.
VI. References
- Kakutani H et al. Risk factors of post-ERCP pancreatitis at a tertiary referral center in Japan. Surg Laparosc Endosc Percutan Tech. 2014; 24: 270-3.
- DiMagno EP et al. The relationship between pancreaticobiliary ductal anatomy and pancreatic ductal and parenchymal histology. Cancer. 1982 15; 49: 361-8.
- Bourke MJ, Costamagna G, Freeman ML. Biliary cannulation during endoscopic retrograde cholangiopancreatography: core technique and recent innovations. Endoscopy. 2009; 41: 612–17.
- Imazu H et al. A pilot study of the novel offset-tip papillotome for selective biliary cannulation in ERCP. Minim Invasive Allied Technol. 2012; 21: 335-41.
- Content Type