Safer, Easier Management of Difficult Bile Duct Stone Cases
Expert tips on EST and EPLBD techniques using the Olympus StoneMasterV

Takao Itoi, MD、PhD、FASGE、FACG
Department of Gastroenterology and Hepatology, Tokyo Medical University
Introducing the StoneMasterV, a new device that enables you to perform both EST and EPLBD procedures with a single device
What is EPLBD?
Over the past few years, endoscopic papillary large-balloon dilation (EPLBD) — which, as its name implies, uses a large balloon — has become an increasingly popular technique for the extraction of large bile duct stones. It is important to point out that there are at least three EPLBD techniques used in treatment of the papilla. The first is the original EPLBD technique documented by Ersoz et al.1 for the first time in 2003. Their paper specified that the indication for EPLBD should be restricted to cases where stone extraction would be difficult even when EST had been performed and introduced the execution of EPLBD on papillae that had been treated with EST. What was most remarkable about this paper was that the authors specified the incision length of EST from the papillary orifice to the vicinity of the hooding fold, ensuring that EST was successfully performed. The second EPLBD technique is for cases recurring after EST has been performed. In this case, EPLBD is performed in a separate session following EST (irrespective of the time elapsed since EST was originally performed) in cases where successful extraction of the stone was not possible with EST alone. Both the first and second EPLBD techniques are quite similar in that both involve EST. The third and final technique is EPLBD without EST.
Is EST necessary in EPLBD?
First of all, let’s examine the mechanism of the original EPLBD technique based partly on my opinion.
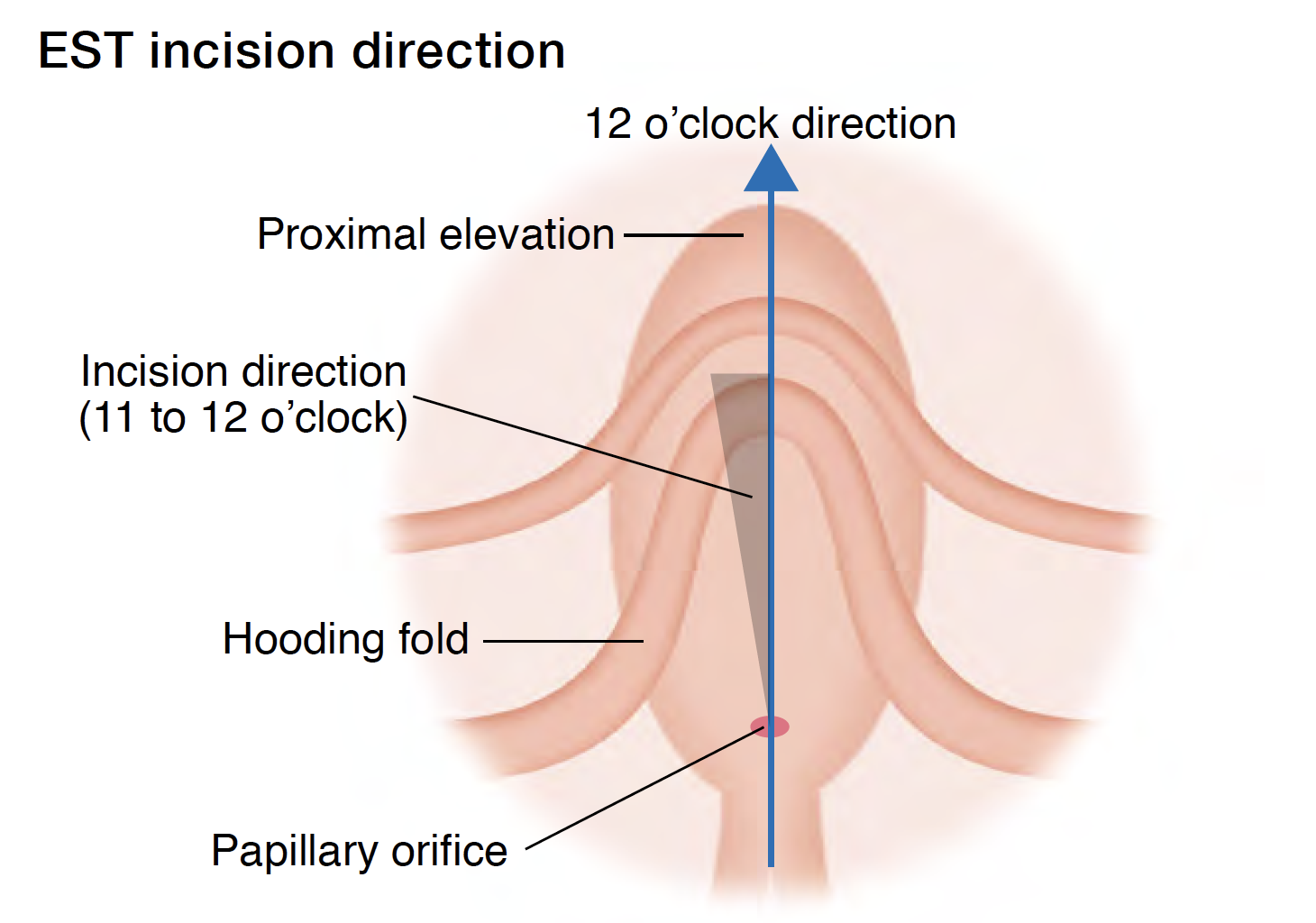
The purpose of dilation of the papillary orifice using a large balloon is to enlarge the bile duct opening to facilitate stone extraction. When a balloon for standard endoscopic papillary balloon dilation (EPBD) — which has a diameter of about 8mm — is used, the papilla dilated by the balloon — uniformly dilated in many cases — can be observed quite clearly. Even if the balloon is inflated to its maximum, the proximal side of the balloon does not cross over the hooding fold. In other words, even when partial tearing of the papillary sphincter occurs, there is no tearing of the papilla itself. On the other hand, in papillary dilation using a large balloon measuring 15 mm or 18 mm in diameter, the papillary opening is excessively dilated almost to the point where the original shape of the papilla is no longer recognizable, and the balloon ends up crossing over the hooding fold when fully inflated. In other words, as a result of excessive dilation, tearing of the papilla becomes much more likely. Consequently, in techniques where EST is performed prior to EPLBD, a cutting margin is required to allow the balloon — when it is inflated excessively — to extend correctly towards the bile duct (in the 12 o’clock direction [see Figure below]). This is the same idea as performing an episiotomy during the second stage of labor. In obstetrics, it is possible to perform a safe parturition with appropriate pretreatment backed up by experience and theory.
Apart from minimizing incidents such as bleeding and puncturing, the cutting margin can also potentially reduce the occurrence of postoperative acute pancreatitis by preventing the mechanical pressure on the pancreatic duct that accompanies EPLBD. In some countries, postoperative acute pancreatitis now occurs more frequently with EPBD than with EST. As a result — and also because fatal cases were reported in RCTs of EPBD2, virtually no EPBD is now performed. Theoretically, the possibility of the occurrence of postoperative acute pancreatitis using EPLBD without EST is the same as with EPBD.
As for EPLBD without EST, there have been some prospective and retrospective studies, but none can be considered sufficiently reliable at this point, leaving open the question as to whether EPLBD with intentional omission of EST can be justified or not. At our hospital, when EST could not be performed for some reason in one clinical case of severe pancreatitis, the patient did not survive. Therefore, we recommend that EPLBD is being performed following a previous EST (we call it ESLBD3 to differentiate it from simple EPLBD) whenever possible to ensure that EPLBD can be regarded as safe.
Interestingly, even Dr. DiSario, who cancelled his RCTs due to a fatal EPBD case and subsequently denied the efficacy of EPBD in his paper2, has said that he could support EPLBD after EST for the same reason4.
Actual EPLBD procedure and the StoneMasterV
Now, let’s see how EPLBD following EST actually works when
the StoneMasterV is used.
Before the introduction of this device, it was necessary to withdraw the sphincterotome after EST, while leaving the guidewire in place, and then insert a large balloon — one which would exactly fit the bile duct diameter and the stone diameter. Common practice also includes preparing a large balloon in advance. Though in some cases, the balloon had the wrong size and a second one had to be utilized. Conclusively, this approach has a negative costs and time performance. To solve these problems, we developed the StoneMasterV sphincterotome with a large balloon in cooperation with Olympus, which took us eight years.
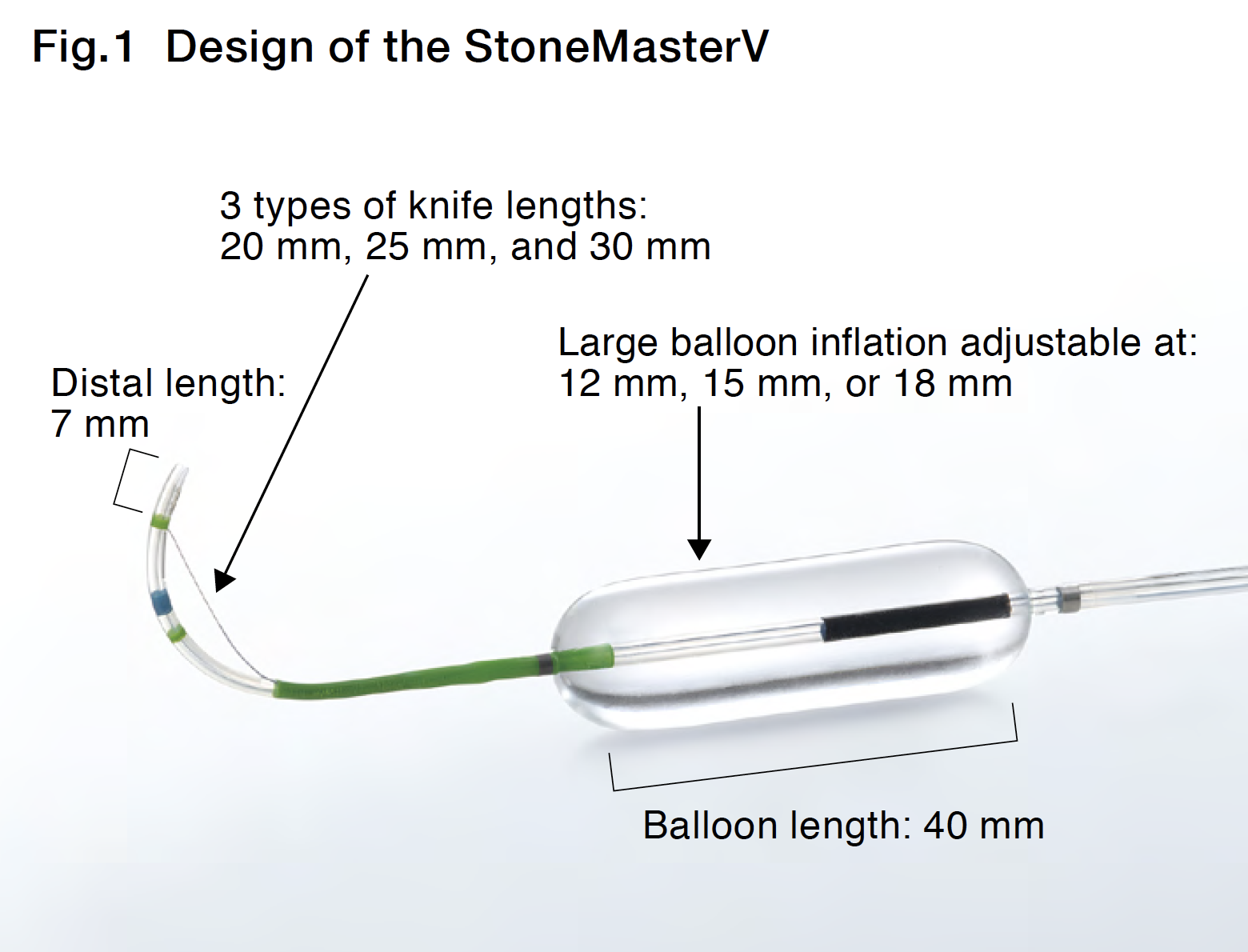
This device is an all-in-one sphincterotome for difficult stone management, featuring a 7-mm distal tip and a 20, 25 or 30mm cutting wire length, — equipped with a 40-mm long — large balloon on the proximal side of the cutting portion (Fig.1).
Thanks to this design, you can perform EPLBD by advancing in the sheath of the sphincterotome continuously after EST. More importantly, unlike other models, you can adjust the size of the large balloon from 12 mm to 18 mm by controlling the inflation pressure, making it truly the world’s first “all-in-one” large balloon for EPLBD (for your information, the inflated balloon diameters are 12 mm, 15 mm, and 18 mm at 0.5 atm., 2.0 atm., and 3.5 atm., respectively).
The following are difficult bile duct stone cases that were managed with the StoneMasterV.
Clinical Case1
Recurrent stacked stones
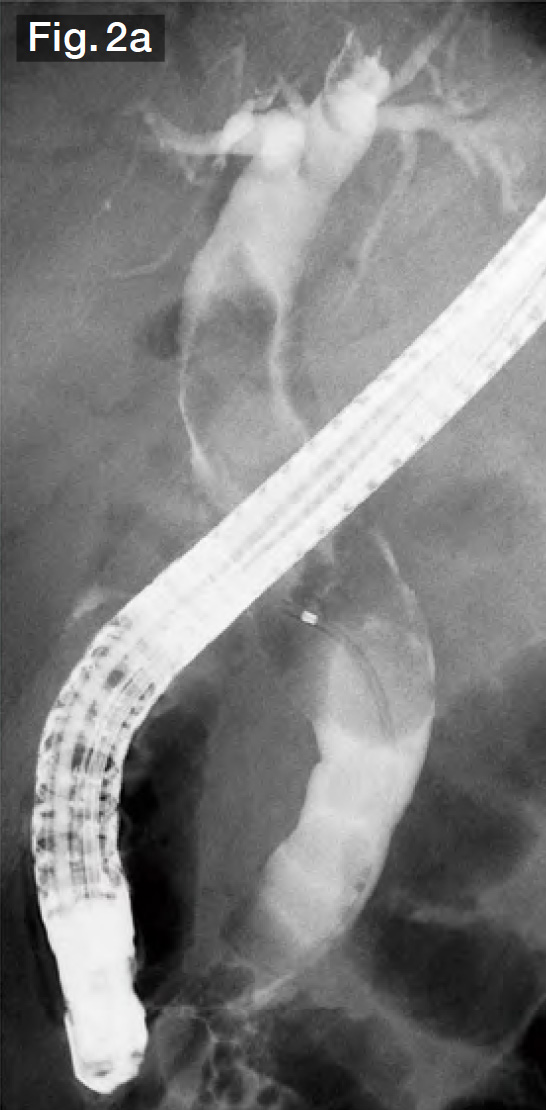
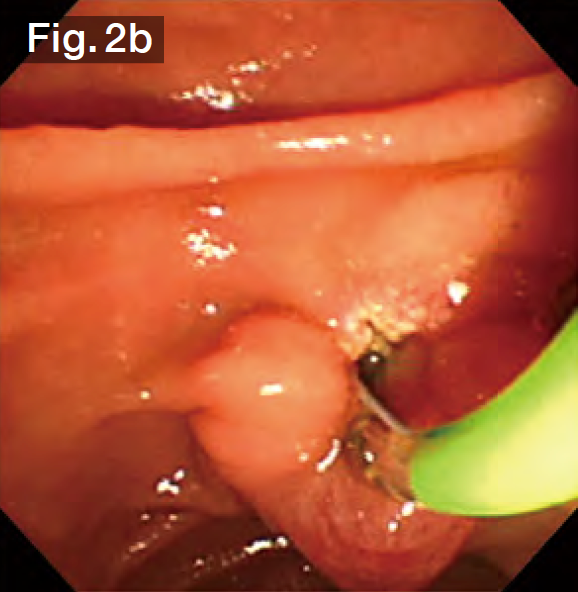
The selective cholangiography we performed for this case showed that the bile duct was filled as far as the porta hepatis with stones ranging in size from 10 to 15 mm (Fig.2a). In therapeutic ERCP at our hospital, we normally perform wire-guided cannulation (WGC) after the execution of EST, so we performed selective bile duct cannulation using the StoneMasterV from the start.
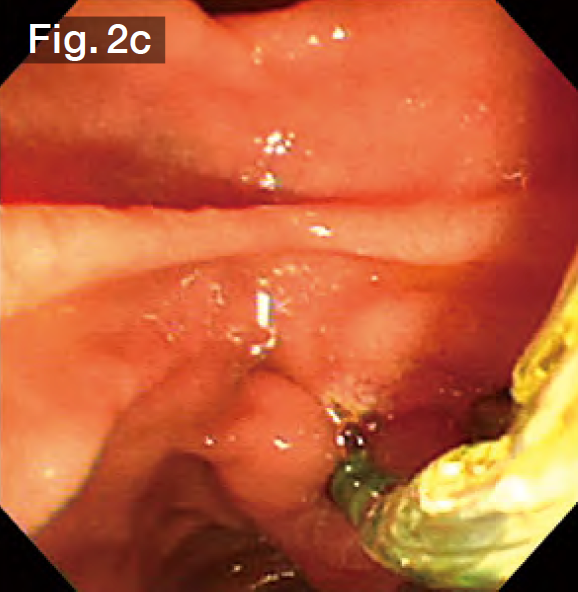
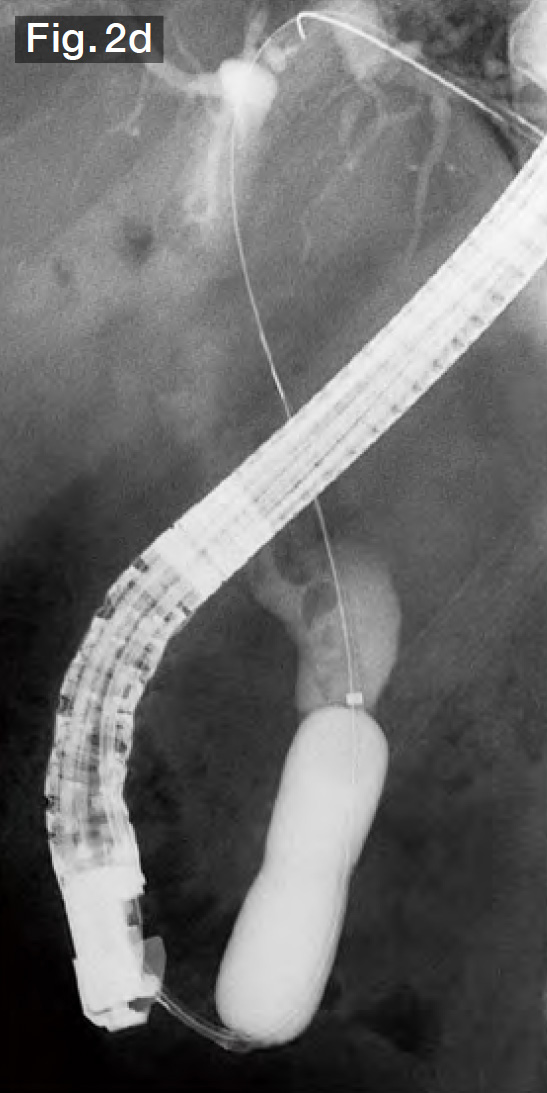
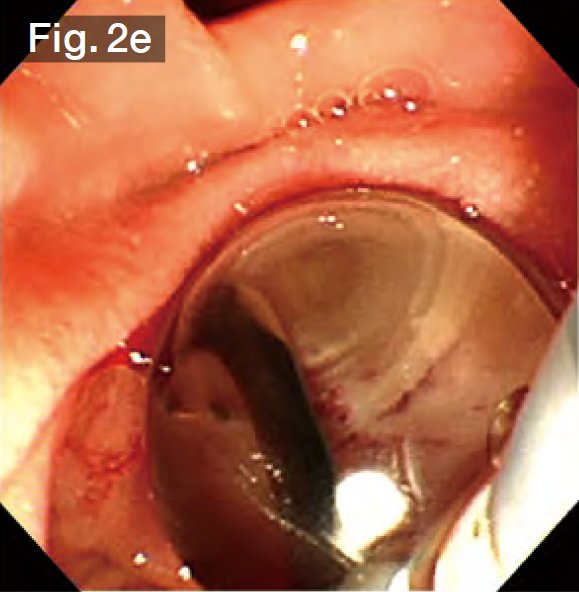
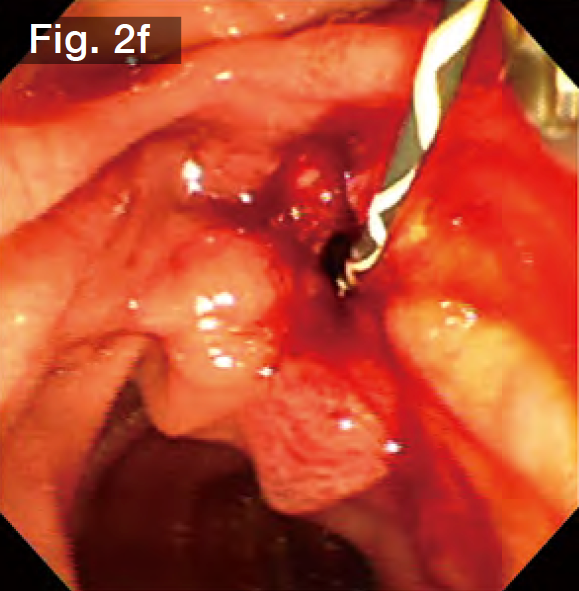
Although EST was performed by the previous doctor, it was insufficient, so we made an additional incision using the Endo Cut mode (Fig.2b) until we reached the point where bile started flowing out naturally. Subsequently, the sheath of the StoneMasterV was advanced, the large balloon portion was inserted into the bile duct (Fig.2c), and the balloon was inflated with a contrast medium diluted by half. The balloon diameter was set to approximately 17 mm at about 2.5 atm., making it roughly the same diameter as the stones and the bile duct (Figs.2d and 2e). The balloon was kept inflated for about 10 seconds and was then slowly deflated. It was confirmed that there was no bleeding (Fig.2f).
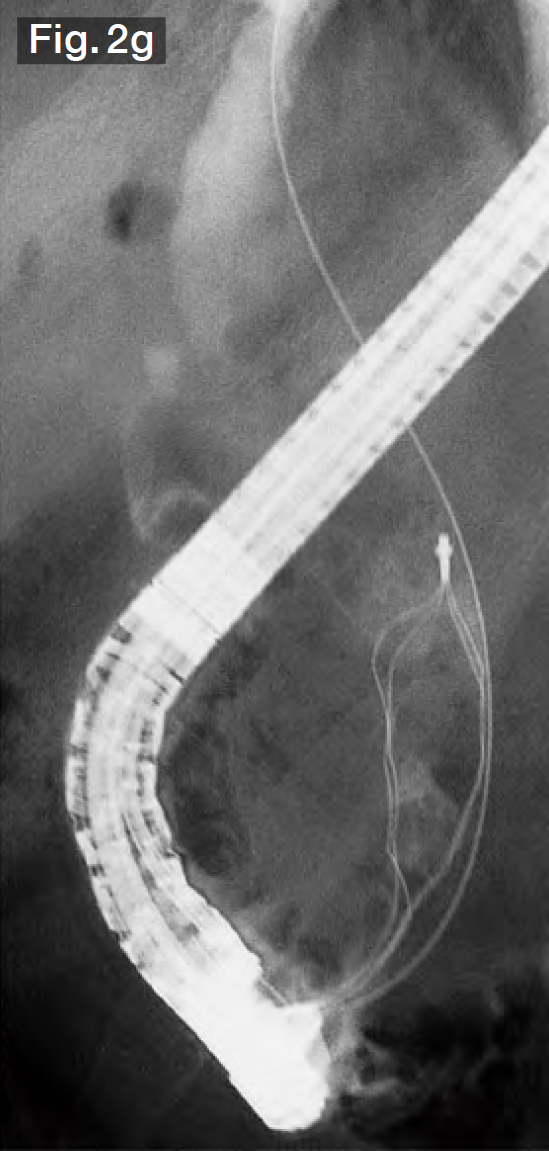
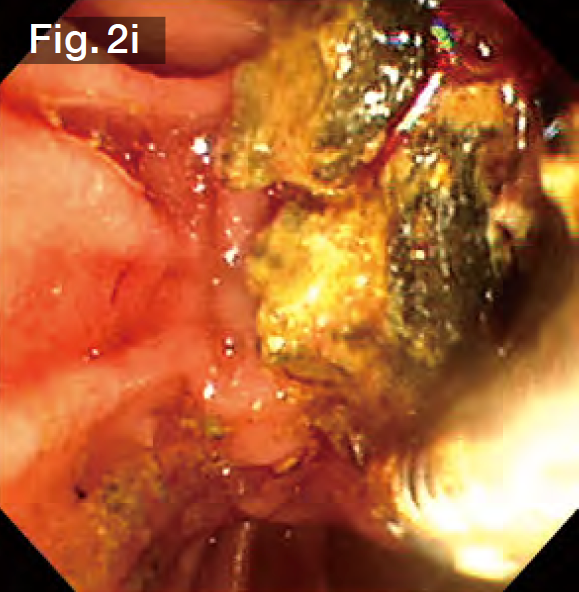
After the StoneMasterV was pulled out without resistance, a wire-guided mechanical lithotripsy basket (Single Use Mechanical Lithotriptor V BML-V437QR-30; Olympus Medical Systems) (Fig.2g) was used to simultaneously extract 3 stones in the lower bile duct (Fig.2h). More stones were subsequently extracted from the lower bile duct without crushing. Finally, we grasped a giant stone in the upper bile duct and tried to extract it. However, it became impacted at the papilla. After pushing it back to the middle bile duct, we crushed it and then extracted it (Fig.2i). Impaction of stones is possible whenever multiple stones are grasped — regardless of whether they are large or small, so it is a good idea to use a basket lithotripter with stone crushing capability.
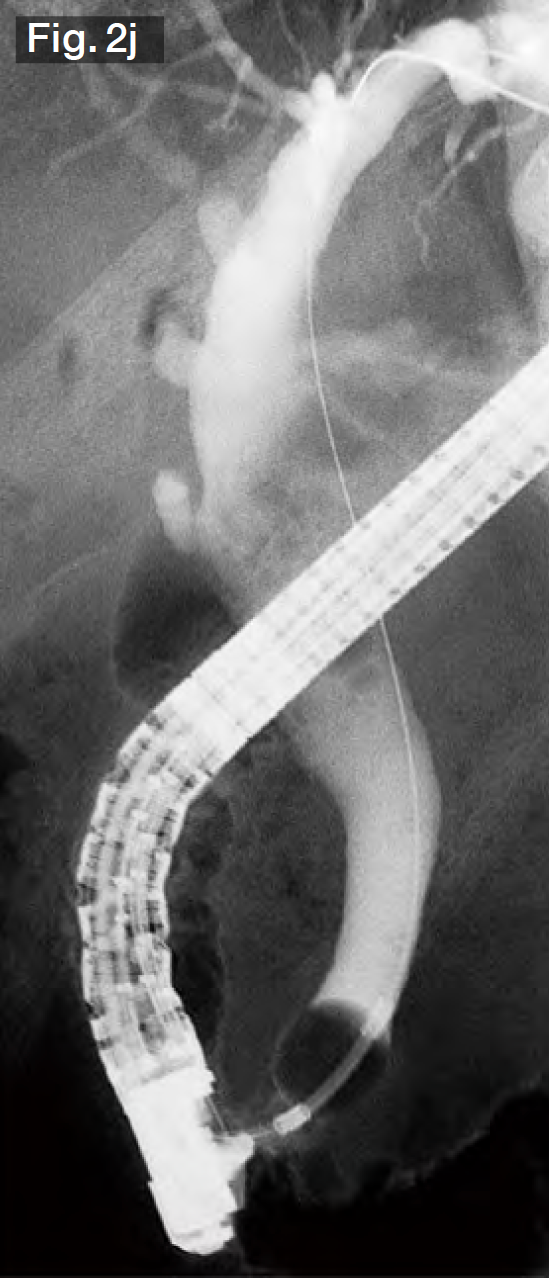
Following stone extraction, no residual stones were observed under fluoroscopy with a contrast-filled balloon (Fig.2j).

Clinical Case2
Post-gastrectomy Billroth-I reconstruction, giant stones
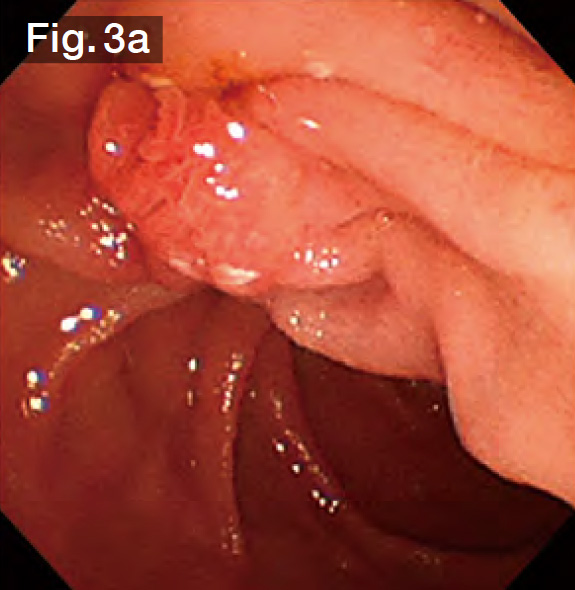
Although we experienced difficulty in viewing the site from the right front (Fig.3a) because this was a Billroth-I case, we started the procedure using the StoneMasterV to perform selective bile duct cannulation. Then we performed further bile duct cannulation with WGC.
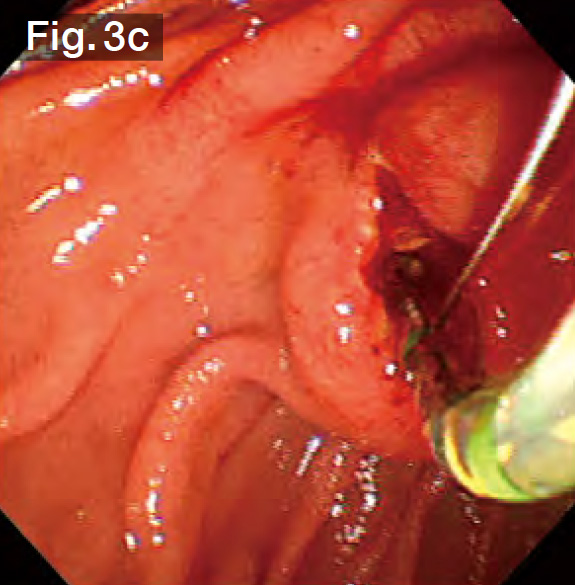
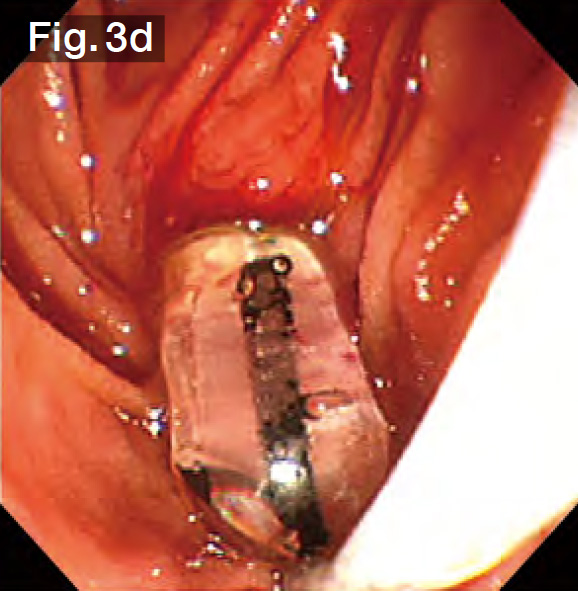
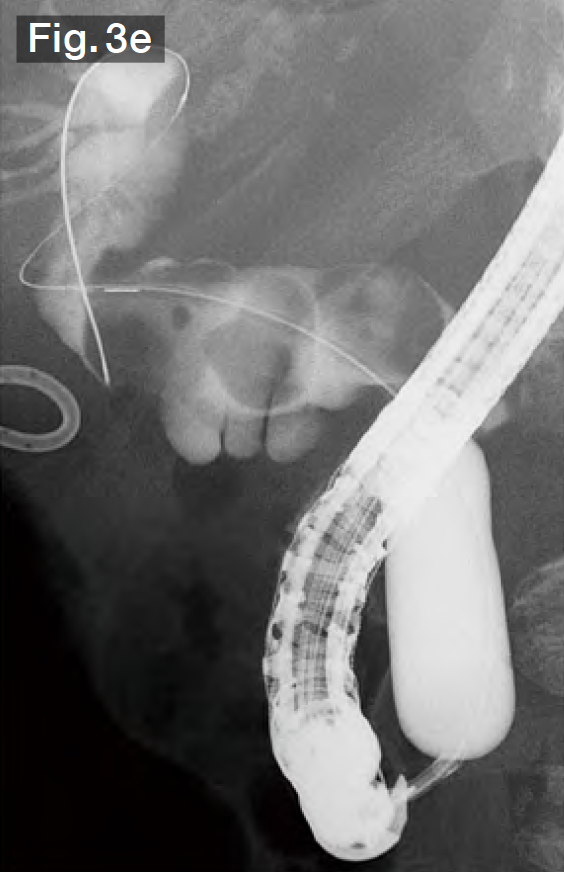
Under cholangiography, we observed 3 stones ranging in size from 15 to 20 mm in the curved bile duct (Fig.3b). The bile duct axis is often curved in Billroth-I cases, so we performed EST precisely in the 12 o’clock direction (Fig.3c). We continued to advance the sheath of the StoneMasterV, inserted the large balloon portion in the bile duct, and inflated the balloon (Fig.3d). Taking the diameters of the stones into consideration, we gradually increased the balloon diameter up to 18 mm at 3.5 atm. (Fig.3e). In this case, the lower bile duct at first glance, so we slowly inflated the balloon, taking about a minute while checking the patient’s vital signs and pain reaction.
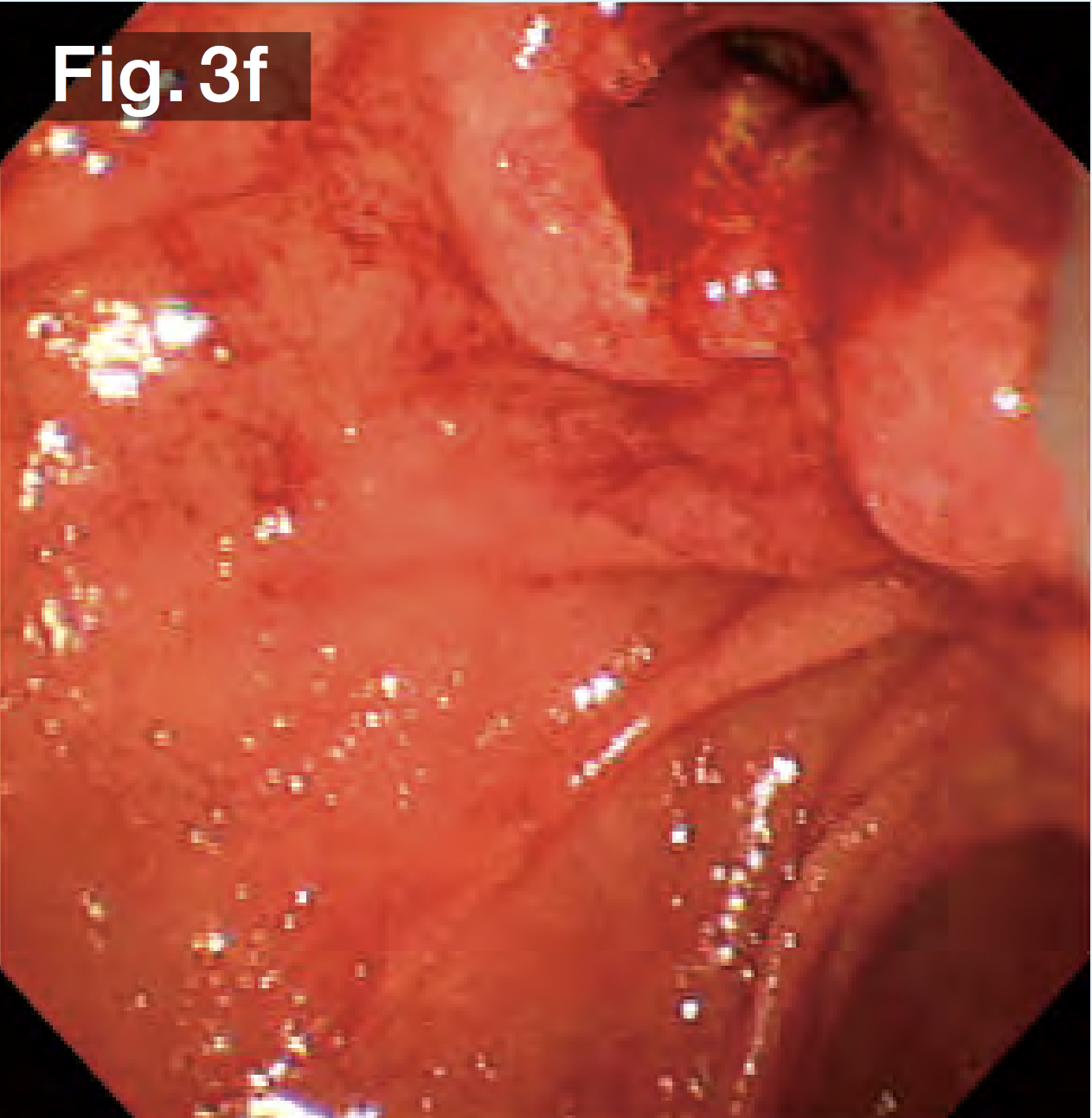
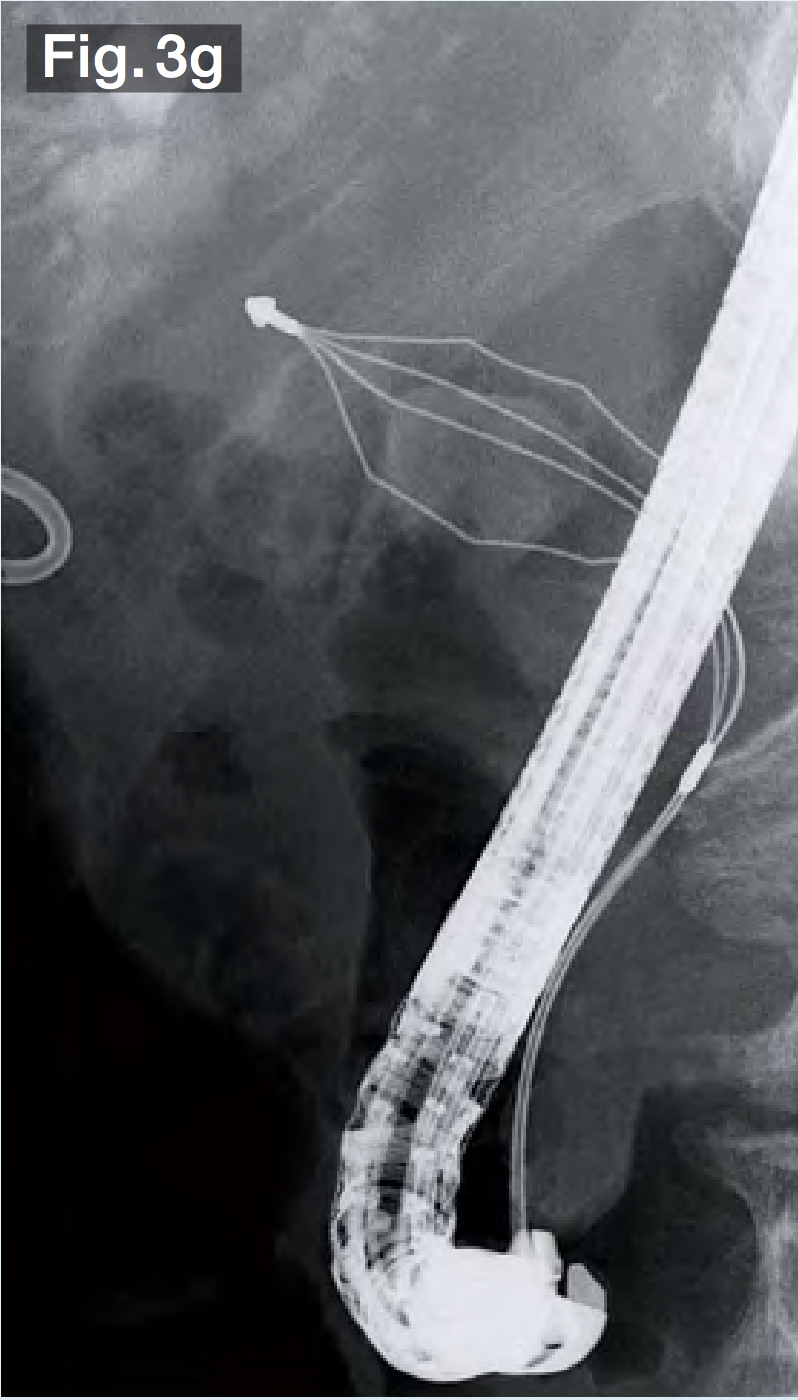
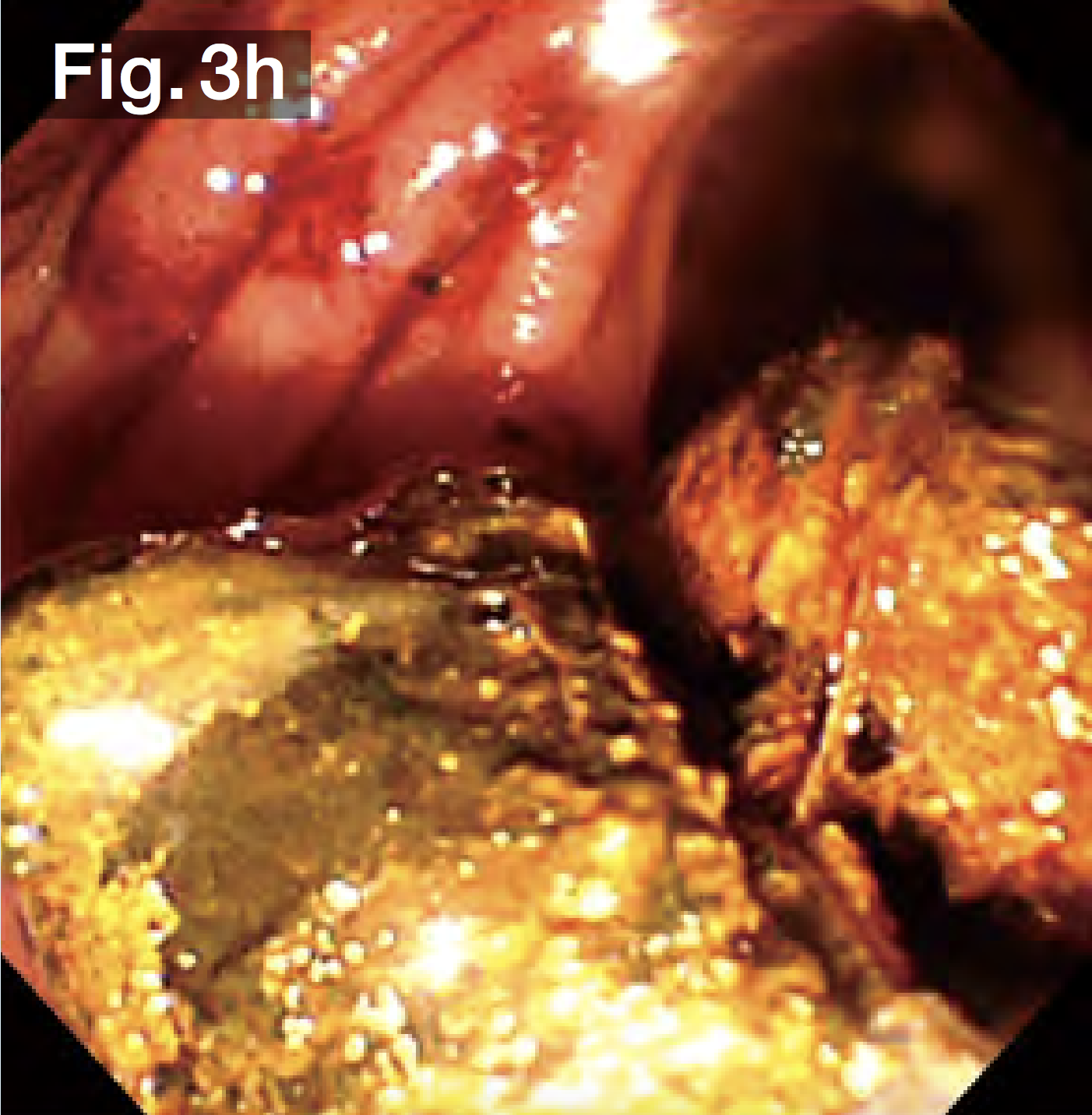
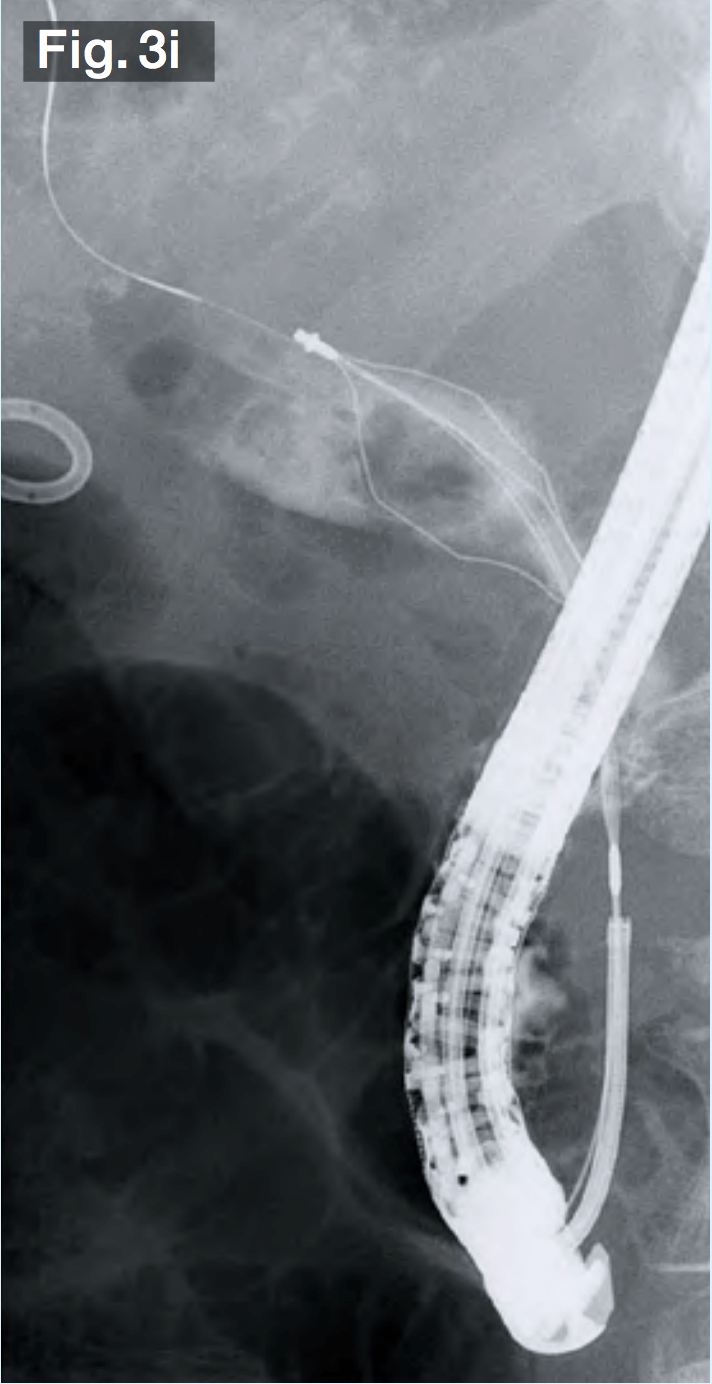
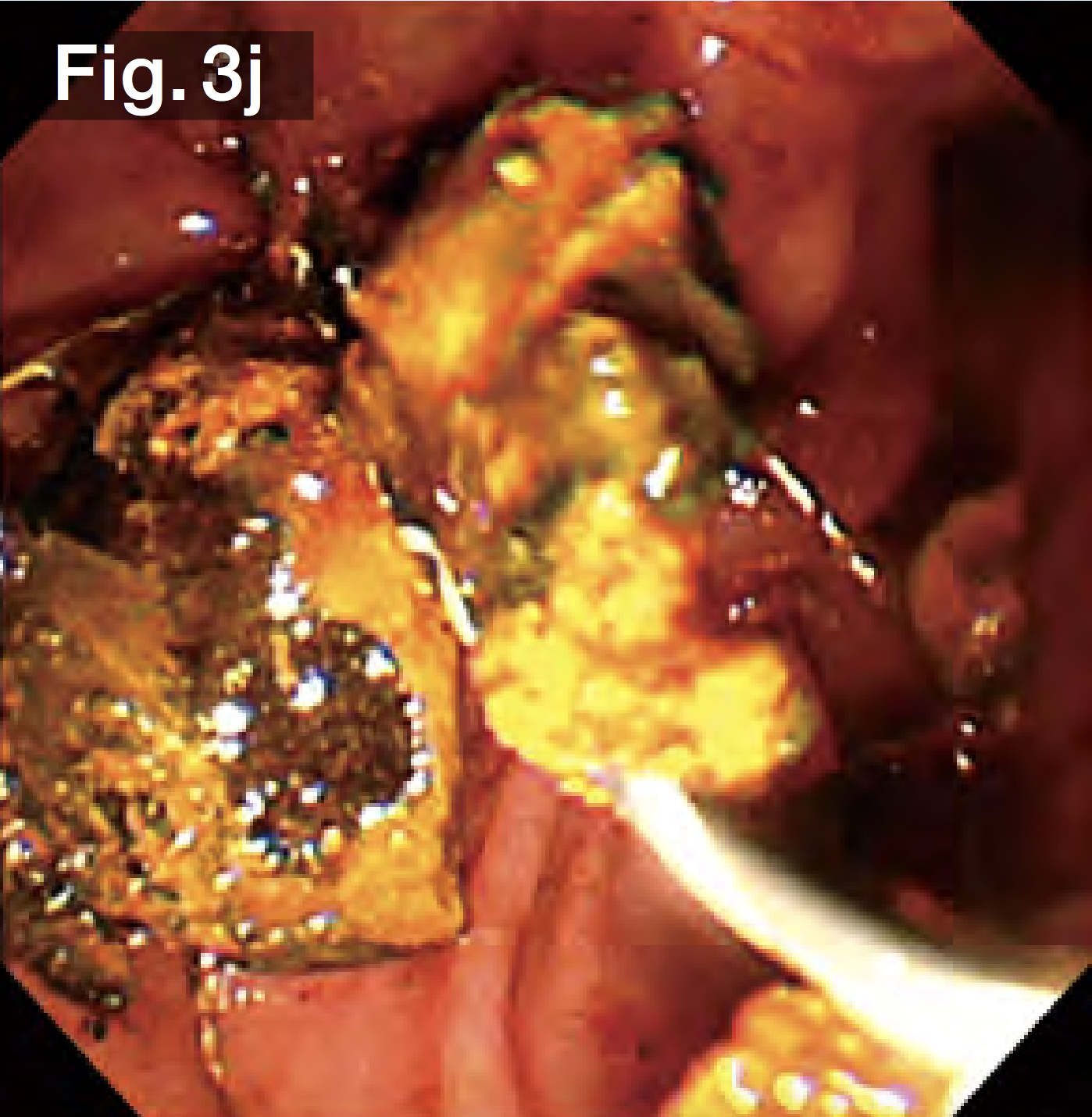
The balloon was deflated slowly, leaving a sufficient bile duct opening with no obvious bleeding (Fig.3f). Since it was possible that the stones would be gigantic and hard, we used a hard wire-type mechanical lithotripsy basket (Single Use Mechanical Lithotriptor V BML-V237QR-30; Olympus Medical Systems) to crush the stones beginning with the ones in the lower duct (Fig.3g) and extracted them (Fig.3h). After this process had been repeated several times, the papilla and bile duct became edematous, making insertion of the lithotripsy basket difficult. We switched to a wire-guided mechanical lithotripsy basket (Single Use Mechanical Lithotriptor V BML-V437QR-30; Olympus Medical Systems) (Fig.3i) to crush and extract the stones (Fig.3j).
After confirming that there were no residual stones under fluoroscopy with the contrast-filled balloon, we finished the procedure.
Mastering the use of the StoneMasterV
In this paper, I have discussed the features and efficacy of the StoneMasterV. While the efficacy of the prototype has already been evaluated in a previous paper5, what distinguishes the final product is its unique, unprecedented all-in-one configuration. Not only does it combine an EST knife and large balloon, it also covers all sizes from 12 mm to 18 mm in a single device.
I am confident that ERCP endoscopists will find difficult stones easier to manage with the StoneMasterV.

REFERENCES
1.Ersoz G, et al. Biliary sphincterotomy plus dilation with a large balloon for bile duct stones that are difficult to extract. Gastrointest Endosc 2003;57:156-9.
2.DiSario JA, et al. Endoscopic balloon dilation compared with sphincterotomy for extraction of bile duct stones. Gastroenterology 2004;127:1291-9.
3.Itoi T, et al. Endoscopic sphincterotomy combined with large balloon dilation can reduce the procedure time and fluoroscopy time for removal of large bile duct stones. Am J Gastroenterol 2009;104:560-5.
4.DiSario JA. Endoscopic balloon dilation of the sphincter of Oddi for stone extraction in the elderly: is the juice worth the squeeze? Gastrointest Endosc 2008;68:483-6.
5.Itoi T, et al. New large-diameter balloon-equipped sphincterotome for removal of large bile duct stones (with videos). Gastrointest Endosc 2010;72:825-30.
Disclaimer:
Any content or information (“Content”) presented herein is illustrative in nature and does not guarantee or represent specific information, outcomes, or results. Olympus Corporation, its subsidiaries, affiliates, directors, officers, employees, agents, and representatives (collectively “Olympus”) does not represent to or warrant the accuracy or applicability of the Content. Under no circumstances shall Olympus be liable for any costs, expenses, losses, claims, liabilities, or other damages (whether direct, indirect, special, incidental, consequential, or otherwise) that may arise from, or be incurred in connection with, the Content or any use thereof
- Keyword
- Content Type