Professor Naohisa Yahagi
Division of Research and Development for Minimally Invasive Treatment,
Cancer Center, Keio University Hospital
DualKnife is a pointed tip-type knife that enables simple operation by creating a sharp cut with minimal thermal injury. It is used in a wide range of ESD techniques including marking, mucosal incision, dissection, and hemostasis. We asked Professor Naohisa Yahagi, who was involved in the development of the new DualKnife J, with an added water jet function to DualKnife, about the clinical utility of DualKnife J and tips for manipulating the device. As well as the characteristics of DualKnife, we asked Professor Yahagi how DualKnife J can bring further advances to ESD techniques.
The criteria for performing ESD at Keio University Hospital
In our hospital, ESD is performed only if the following criteria can be met: there is no risk of lymph node metastasis, the lesion is approachable, and patient safety can be assured including backup by the Surgical Department during and after the procedure. When these criteria are met we shall perform ESD, regardless of the size of the tumor or the patient’s treatment history. Needless to say, we carefully determine which patients are eligible for ESD by consulting surgeons from other departments in multidisciplinary treatment conferences.
Our hospital is unique in having a large number of duodenal cases. Duodenal ESD can be extremely challenging, because the narrow lumen makes the lesion difficult to approach and the endoscope harder to maneuver. Also, the risk of perforation is high due to the thin duodenal wall. Not only does duodenal ESD require great skill, it also demands considerable experience to select the most appropriate treatment strategy and tools for the procedure. Therefore, duodenal ESD should only be carried out by physicians who are considerably experienced in ESD procedures.
Versatility of DualKnife and its utility in ESD
In our hospital, we mainly use DualKnife when performing ESD, which is a multifunctional tool for marking, mucosal incision, dissection, and hemostasis. We use the 2-mm knife for the stomach, which has a relatively thick wall, and the 1.5-mm model for the esophagus, colon, and duodenum. The basic electrosurgical settings for each location are shown in Table 1.
[Table 1] High-frequency settings for DualKnife series during ESD
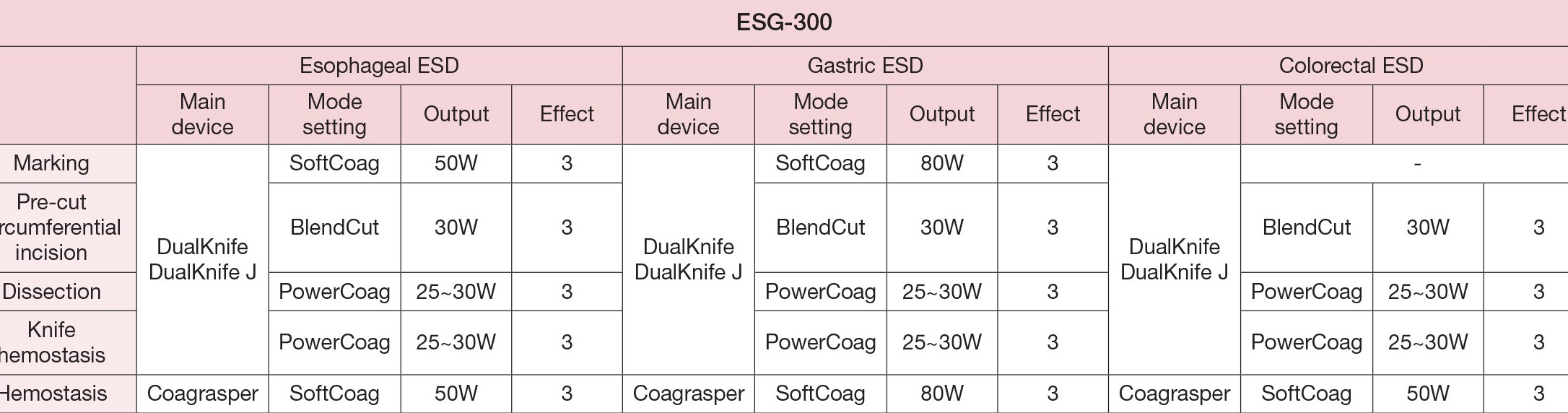
CAUTION: The following settings are examples based upon previous general clinical usage of the device. Please note that clinical staff are solely responsible for the selection of an appropriate mode and power level, dependent upon the instrument being used and the condition of the tissue being treated. Due to the heterogeneity of instruments and clinical conditions, Olympus cannot accept liability for clinical risks arising from the use of these example settings.
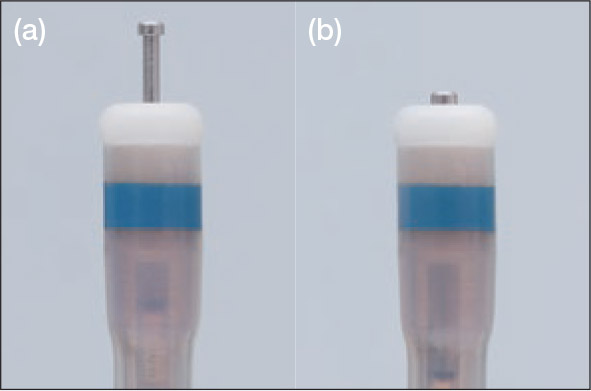
Feature 1: Adjusting the knife length in two positions
A major feature of DualKnife is the simple adjustment of its knife length in two positions: extended or retracted (Fig. 1). Since the knife length of DualKnife (KD-650 series) can be maintained regardless of whether it is in the extended or retracted state, it does not require minute adjustments based on the surgeon’s own judgment, facilitating very stable manipulation. Also, since the knife can fully come in contact with the tissue, the procedure can be performed safely without being affected by trembling or peristalsis.
Marking and hemostasis are mainly performed with the knife retracted. Since it is not necessary to adjust the knife length during marking, the device can be left in the retracted state closely adherent to the mucosa, which makes manipulation of the knife by the assistant far less complicated. Furthermore, hemostasis for minor bleeding or of small blood vessels up to 1 mm can be performed with the knife retracted. Performing hemostasis with the knife in the extended state risks damaging deep veins or the muscle layer. In contrast, when the knife is retracted it
can be used like a cautery to cleanly stop the hemorrhage by simply pressing the tip of the device against the bleeding site, resulting in safe and reliable hemostasis.
Feature 2: Disk-shaped knife tip
Since the tip of the knife is disk-shaped (Fig. 1) and the edge of the disk base has a 90° angle, tissues can be hooked and caught securely using this edge. Thus, even a fibrotic lesion can be cut very precisely, provided the tissues around it have been sufficiently dissected to expose the scar by hooking the scar tissues with the disk edge.
Feature 3: Small diameter (2 mm) of the proximal sheath
Since the proximal sheath has a small diameter of only 2 mm, water, blood, or vapor can be suctioned with the knife inserted in the forceps channel. Furthermore, while irrigation using the water jet can identify a bleeding site, a clear operative field cannot be achieved once there is accumulation of water and blood. When DualKnife is used, the surgeon can proceed directly to hemostasis using the device, since water can be suctioned with the knife in the forceps channel. This is particularly useful when the lumen is narrow and water tends to accumulate such as in the esophagus or the colorectum. Here DualKnife enables ESD to be performed safely and reliably once the position of the knife tip at the contact site is visually confirmed.
Feature 4: Sheath design
DualKnife has a flexible sheath that enables adept front-and-back and left-and-right control, which is particularly useful when approaching lesions through a narrow lumen. Additionally, the sheath’s flexibility and rounded ceramic tip allow the knife to be manipulated smoothly through the scope’s forceps channel even in an up-angle approach, enabling resections that can only be dealt with in tight retroflexion. In order to perform an accurate mucosal incision and dissection, it is crucial to approach the lesion by making full use of the sheath’s flexibility while maintaining the necessary distance from the lesion.
When performing an incision and dissection, the rounded sheath tip allows for smooth manipulation without being caught in the tissues. Moreover, incision and dissection can be performed at a uniform depth by contacting the rounded tip onto the tissues and using only the knife tip to cut into the tissues. Skilled surgeons are thus able to make a sharp incision and dissection at a constant speed without being influenced by respiratory variations or pulsation.
Furthermore, the blue marker on the sheath tip can be used as a depth indicator. If the white ceramic tip and the blue marker are visible during the procedure, the device is used more safely without cutting deeply because the knife can be manipulated at a constant depth.
ESD techniques utilizing the water jet function of DualKnife J and tips for manipulation
Seamless transition from submucosal elevation to incision and dissection assisted by the water jet function
In order to incise and dissect the tissues safely and reliably when performing ESD, it is critical to create optimal submucosal elevation by local injections to the submucosa. For many lesions, at least 4 or 5 additional local injections are performed during a single ESD session.
However, in cases where it is difficult to maintain the submucosal elevation, such as with laterally spreading tumor non-granular type (LST-NG) in the colorectum or with large lesions, more frequent local injections may be required.
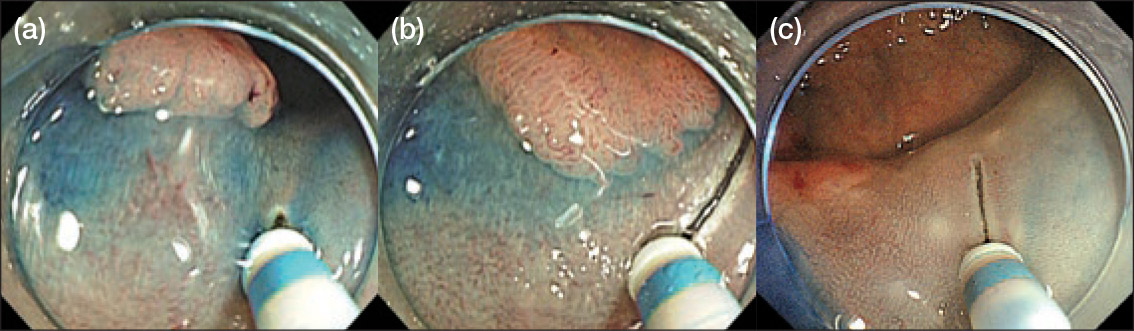
When using DualKnife J (Fig. 2a) equipped with the added water jet function, the surgeon can proceed directly to mucosal incision and dissection after performing submucosal elevation with injections via the knife. Furthermore, when it is difficult to secure a stable surgical view, such as with lesions that are in a strongly curved position in the colorectum, the endoscopic view often alters when changing between the injection needle and the knife. This can create difficulties in continuing the procedure once the endoscopic view is altered when the devices are switched. However, when the water jet function of DualKnife J is used, it is not necessary to change devices. This creates a major advantage in terms of procedural ease and saved time even in difficult cases.
Secure submucosal elevation improves the visibility of blood vessels in the submucosa, which helps to prevent bleeding. Moreover, the water jet function of DualKnife J helps to reliably establish submucosal elevation before powering the device, which reduces the risk of perforation during dissection (Fig. 2b). Therefore, I believe that DualKnife J is a very safe and convenient knife for physicians who want to master ESD techniques.
[Fig. 2] Water jet using DualKnife J

(b) Safety is improved by dissecting immediately after reliable creation of submucosal elevation with the knife injection
When feeding the sterile saline into the mucosa, pull the slider to retract the cutting knife.
Advantages of maintaining knife performance using the water jet function
Additional benefits of the water jet function are demonstrated by its facilitation of optimal knife performance. For example, tissues and clots that stick to the knife during hemostasis can become carbonized, which reduces the knife’s ability to cut and coagulate. When using DualKnife, debris that is adherent to the knife is removed by repeatedly moving the handle slider back and forth. On the other hand, with the added water jet function of DualKnife J, the debris can be removed by irrigating through the water jet, making it easier to maintain the knife’s ability to cut and coagulate. Even when it is difficult to expel debris by extending and retracting the knife as described above, the water jet can usually flush out adhesive material on the tip. Thus, I recommend doing this fairly frequently during the procedure.
Tips for reliably creating submucosal elevations by knife injection
The key to creating an optimal submucosal elevation by knife injection is to approach the lesion site with the knife edge parallel to the wall, instead of approaching the muscle layer en face. Then, knife injections should be performed by perpendicularly placing the knife against the exposed submucosa in order to prevent water leakage to the surrounding area (Fig. 3a). Once a good submucosal elevation has been achieved, the knife tip is extended while brought in contact against the submucosa, and then powered with electrocautery to create a “pocket” (Fig. 3b). Then, additional knife injection with the knife tip extended is performed (Fig. 3c), which more reliably establishes further submucosal elevation. For fibrotic lesions, the solution is first injected into surrounding areas that have relatively mild fibrosis, enabling submucosal dissection of the adjacent tissues. Once the central area with more severe fibrosis is isolated, an injector needle should be used.
[Fig. 3] Submucosal elevation by using DualKnife J
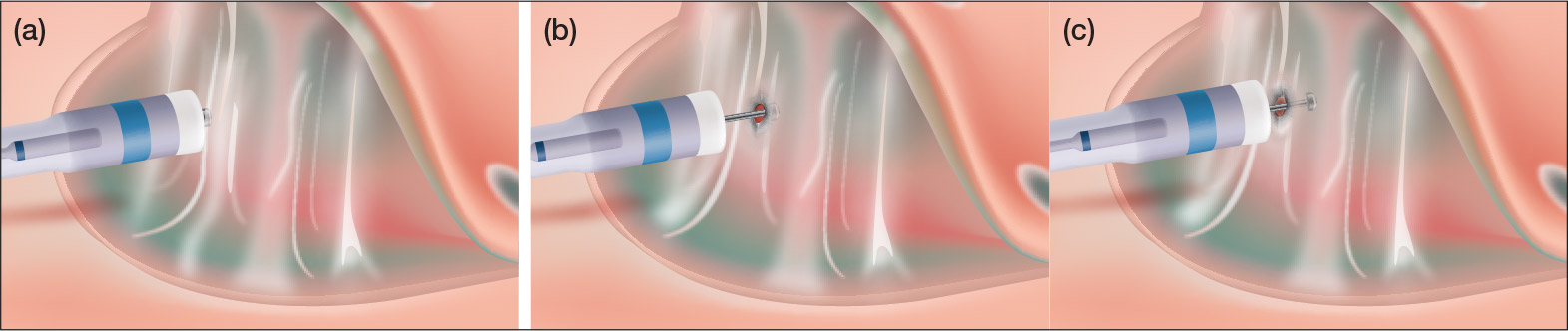
(b)-(c) Water injected from knife the when the tip is extended
Creating a pocket by powering/contacting the device to the submucosa when the knife tip is extended (b) injecting water from the tip with the knife being extended (c)
When feeding sterile saline into the mucosa, pull the slider to retract the cutting knife.
Balance between the pre-existing specifications of DualKnife and the new water jet function
Emphasis on retaining the cutting and suctioning ability of DualKnife
DualKnife J retains most of the features of DualKnife. Since it retains the small knife diameter and the disk-shaped tip, its ability to cut and hook tissues remains comparable (Fig. 4a-c).
Moreover, since DualKnife J has the same sheath diameter as that of DualKnife, it is still possible to suction alongside the knife when it is inserted in the forceps channel. If it were a larger diameter, the knife would need to be removed and reinserted in order to suction, resulting in a prolonged procedure. Since DualKnife J retains the same sheath diameter as DualKnife, seamless transition from flushing to suctioning and dissecting is maintained.
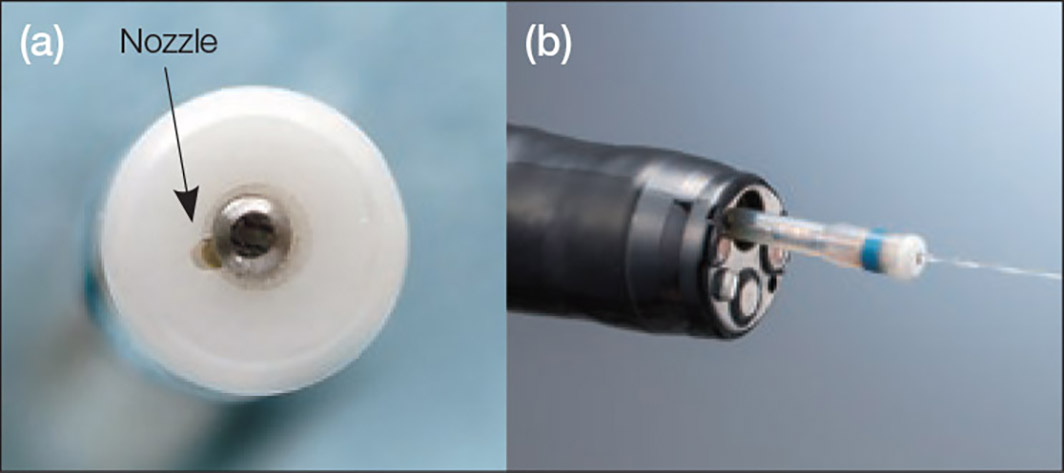
Change in specification associated with addition of the water jet function and tips for manipulation
The water jet function of DualKnife J allows for efficient injection into the submucosa with fairly high pressure. DualKnife J has been designed with the nozzle condensed to a single point beside the knife (Fig. 5a), which can project a linear water jet, allowing efficient injection (Fig. 5b).
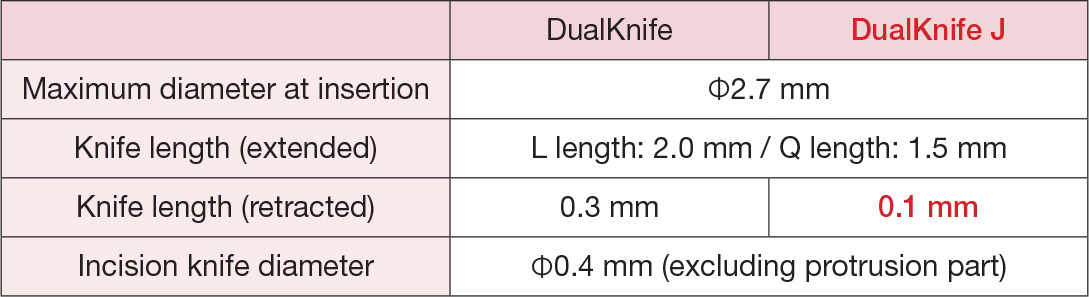
To allow for this specification, the knife length at the retracted position has been changed to 0.1 mm compared to 0.3 mm with DualKnife (Table 2). The shorter knife length results in an increased current density even at the same high-frequency settings, which means that DualKnife J can create more clearly defined markings. However, since the size of the marking itself has become smaller, the high-frequency settings may be appropriately changed by increasing the wattage, in order to create larger markings (see Table 1).
The hemostatic performance of DualKnife J is comparable to that of DualKnife. When performing hemostasis, the knife must be retracted to avoid deep injury leading to perforation, but it remains important to ensure that the disk of the knife tip comes into firm contact with the site of hemorrhage. However, since the knife length at the retracted position for DualKnife J is shorter than that of DualKnife, the shape of the knife tip has become flatter. Therefore, when hemostasis is performed by a physician with less experience in ESD procedures, it is essential to manipulate the device with greater precision to ensure that the center of the knife tip comes into firm contact with the site of hemorrhage.
Seamless ESD techniques brought by DualKnife J
When using DualKnife, it is important for assistants to master the manipulation of “extending the knife during incision and dissection, and retracting the knife during hemostasis.” If hemostasis were to be performed with the knife extended, the risk of perforation would increase.
Therefore, if the assistant lacks experience with ESD procedures, the surgeon must check the status of the knife at every opportunity. This is also true when using DualKnife J. However, since it is no longer necessary to change devices for submucosal injections, this should allow for smoother coordination between surgeons and assistants.
When performing ESD, maintaining an optimal submucosal elevation and performing the incision and dissection at a constant depth results in a safer and more effective procedure with decreased risks of procedural complications. DualKnife and DualKnife J both possess the following three advantageous features that facilitate a successful procedure: [1] flexible sheath, [2] easiness of handling the knife, and [3] stable handling provided by the disk-tipped knife and the rounded sheath tip. Together these allow the operator to incise and dissect in any direction at a stable speed while a constant depth is maintained.
With the addition of the water jet function, DualKnife J can now deal with almost all of the steps involved in ESD. Moreover, because the new knife allows for a stable submucosal elevation to be created as needed, it has made the transition from creation of submucosal elevation to incision and then to dissection seamless, greatly improving the efficiency and safety of the ESD procedure.
Introduction of facilities
Keio University Hospital
The Division of Research and Development for Minimally Invasive Treatment at Keiko University Hospital’s Cancer Center takes a large number of referrals from other hospitals, particularly difficult cases of malignant and benign tumors. The division performs endoscopic examinations in collaboration with other departments through multidisciplinary conferences, with a full surgical backup system in case of serious complications. Although ESD is now covered by health insurance, there has not been a significant increase in the number of ESDs performed for lesions in the stomach and colorectum, because the division has primarily focused on difficult patients who could not be treated at other hospitals. We perform approximately 150 ESDs for stomach, 100 ESDs for colorectum, and 100 ESDs for esophagus annually. The number of duodenal lesions treated by ESD annually is approximately 70 since there has been year-on-year increase in the number of referrals for difficult cases from other hospitals, in particular due to our excellent track record for duodenal ESDs.
- Keyword
- Content Type