Small Intestine case 2

Dr. Kazuo Ohtsuka
Department of Endoscopy, Institute of Science Tokyo Hospital, Japan
Introduction - Features of the Device
Single balloon endoscope (SBE) has evolved. The new SBE, SIF-H190, features improved insertion capabilities by adopting passive bending. Its increased forceps channel diameter enhances maneuverability of instruments. These improvements expand the possibilities of enteroscopy.
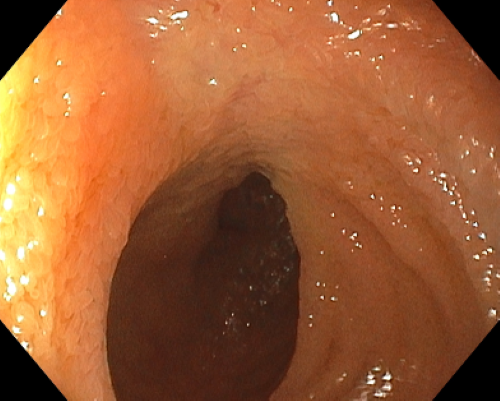
In addition, a simultaneous imaging has been adopted. Another imaging method, sequential imaging was used in Japan because of higher still image quality, though more blurring caused by respiratory fluctuations occurred. However, with the progress of technology, the simultaneous imaging can obtain detailed quality images comparable to the sequential imaging.
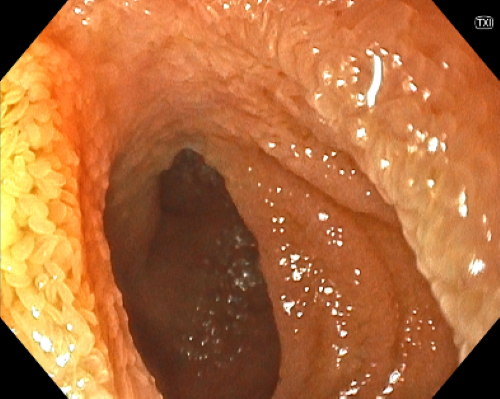
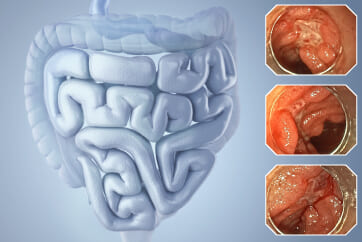
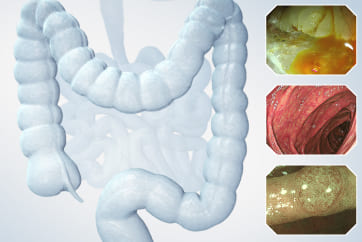
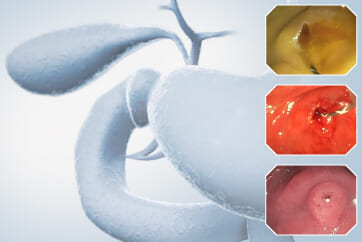
New image enhanced endoscopies are available. Not only classical Narrow Band Imaging (NBI), TXI (Texture and Color Enhancement Imaging) mode and RDI (Red Dichromatic Imaging) mode can also be available. They allow detailed observation.
Benefits of Passive Bending
High accessibility to lesions is critical for enteroscopy. Upper gastrointestinal endoscopy observes the esophagus, stomach, and duodenum, and colonoscopy observes the entire large intestine including the terminal ileum. On the other hand, enteroscopy does not require observation of the entire small intestine in many cases. However, bleeding cases that upper gastrointestinal endoscopy and colonoscopy could not identify the lesion needs examination of the entire small intestine. Furthermore, most of patients with Crohn’s disease that is a chronic inflammatory bowel disease, have small bowel lesions. Its protracted inflammation often leads to intestinal deformity and adhesion. The formation of fistulas and abscesses need surgical operations. These intestinal damages hamper the deep enteroscopy. Endoscopic balloon dilation, which has become popular as a minimally invasive treatment for strictures, is expected to be a new treatment for Crohn’s disease. However, treatment may be abandoned due to inability to reach the lesion in some cases. For these reasons, enteroscope with high accessibility is required. The passive bending function improves insertability dramatically in colonoscopy. This function distributes the force applied to the scope over the entire curved part, transmitting enough force to advance the tip of the scope deeper. It overcomes the difficulties when the tip of the scope becomes cane-shaped and force is not transmitted effectively to the tip. The SIF-H190 also incorporates the passive bending function and has proven to improve insertability. The small intestine has complex curves within the abdominal cavity, but the passive bending function makes it easier to pass through these curves, improving the ability to reach deeper parts.
Case Video
"Observation of the entire small intestine by trans-anal approach"
Changes in Insertion Techniques
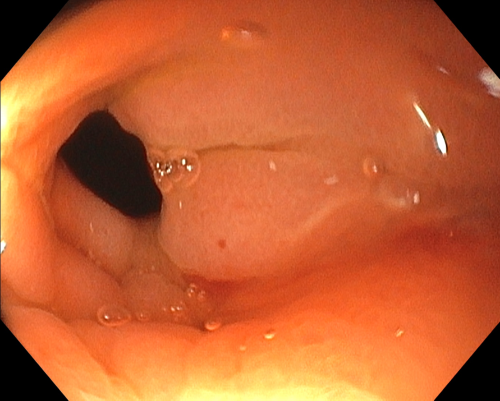
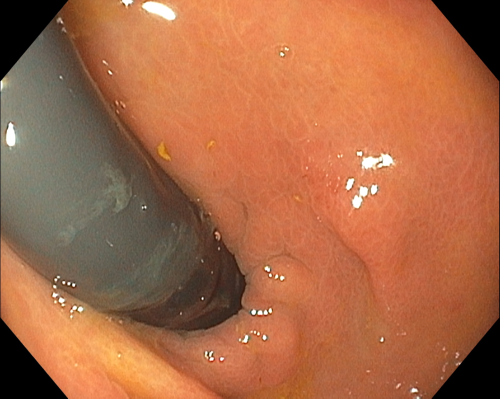
One of the challenging areas to pass during trans-anal insertion is the ileocecal valve. Typically, the ileocecal valve is positioned at the 9 o’clock direction in the field of view, and the scope tip is pressed against the center of the valve to pass through. If the ileocecal valve is facing the cecal side, the balloon on the overtube is used to grasp and pull back the ascending colon, repositioning the valve to face the ascending colon side, and then attempting to pass through. Avoid over-insufflation, as excessive air can cause the ascending colon to distend. Changing the patient’s position from supine to left lateral decubitus is also effective. Manual compression of the right lower abdomen to displace the bowel is another technique. Retroflexion technique was used in some difficult cases. It is that retroflexing the scope in the cecum, then withdrawing the scope while angling it to insert the tip into the terminal ileum, and then gradually releasing the scope angle for paradoxical movement to advance the scope into the deeper small intestine. The passive bending function makes possible to pass through the ileocecal valve simply by inverting the scope within the cecum and carefully advancing it in the difficult cases. It was reported that the passive bending feature reduced the time required to pass through the ileocecal valve after reaching the cecum.
During passage through the pelvic cavity, the scope’s shape can sometimes become hook shape, making deep insertion difficult. To avoid the hook formation, the scope should be advanced in a direction below the center of the endoscopic view. Additionally, avoid shortening the bowel during the initial 1-2 strokes immediately after passing the ileocecal valve. However, hook shape formation can still occur in some cases. And when pulling back the overtube for the changing the angle of the scope tip, the tip of the overtube may slip back from the ileocecal valve into the colon. The balloon’s grasping force on the bowel is not very strong for safety reasons, so it may slip and retract if excessive force is applied. When the balloon slips from the ileum back into the colon, this is detected by a sudden drop in the pressure displayed on the balloon controller. In such cases, wait for the balloon to re-expand at the ileocecal valve, allowing it to regain its grasp on the colon before proceeding to insert the scope into the ileum. During this process, use the passive bending feature by gently pushing the scope forward as it is inserted.
During oral insertion, passing through the pylorus can be challenging. When the stomach with decreased tension becomes excessively distended, the scope tip may take on a hook shape at the gastric angle. To prevent this, with minimized insufflation while passing through the stomach and advance the scope along the lesser curvature. Even when hook shape formation does occur, the passive bending function can be useful.
Enlarged Instrumental Channel Diameter
The instrumental channel diameter has increased from 2.8 mm in the SIF-Q260 to 3.2 mm in the SIF-H190. In the case of procedures on smaller-bodied patients or in cases with intestinal adhesions, the concentric small bowel loops created during insertion tend to be smaller, resulting in increased bending of the scope. These situations make difficult for insertion and removal of thicker devices though the instrumental channel. In cases with intestinal adhesions or deformities, catheter devices are inserted or removed while the scope is sharply angulated though it is not recommended as it can damage the lumen of the instrumental channel. Even in such cases, the increase in the instrumental channel diameter has made the operation easier. Furthermore, since the cross-sectional area of the instrumental channel has increased by 31%, allowing for quicker suction of fluids and gases within the intestines. Suction operations while the forceps are inserted through the channel have also become easier. Multiple strictures can be observed within the small intestine in Crohn’s disease and other stricture diseases. While dilation procedures using TTS balloon catheters are performed in such cases, thicker balloons like the 15mm type were often difficult for multiple procedures. This leads to the use of multiple catheters in a single endoscopy. The increased instrumental channel diameter now allows for easier repeated use, resulting in cost savings and a reduction in medical waste. This is also economically beneficial.
NBI and proprietary IEEs
The SIF-H190 is compatible with the EVIS X1 as the imaging processor. In addition to NBI, it supports Olympus’s proprietary image enhancement endoscopy such as TXI and RDI.
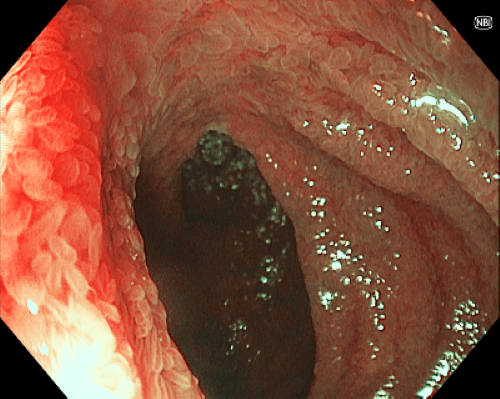
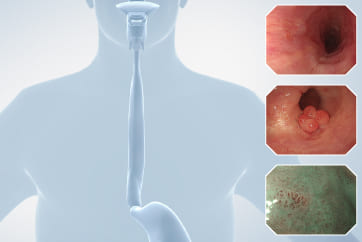
NBI uses two wavelengths of light, 415 nm and 540 nm, narrowed by a dedicated optical filter. These wavelengths are strongly absorbed by hemoglobin, making red blood cells more visible and enhancing the clarity of capillaries and their patterns on the mucosal surface. NBI is useful for diagnosing epithelial tumors, though there are few carcinoma in the small intestine unlike the esophagus, stomach, and large intestine. NBI is also useful for diagnosing angioectasia, which causes bleeding, and erosions and ulcers in inflammatory diseases such as Crohn’s disease.
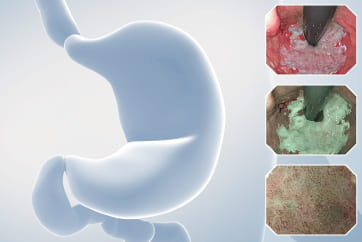
TXI is an image enhancement technology that optimizes three elements of the mucosal surface: “structure,” “color tone,” and “brightness.” By using TXI, even subtle changes in color tone or structure are highlighted, which is expected to contribute to improved observation performance of lesions.
RDI enhances the visibility of blood vessels and bleeding point by illuminating with red light (620-640 nm), amber light (595-610 nm), and green light (520-550 nm). The amber light is more readily absorbed by hemoglobin than red light. It penetrates deeper into the mucosa due to its longer wavelength compared to green light. This characteristics improve the visibility of deep mucosal blood vessels with RDI. Additionally, during bleeding, the entire endoscopic view may become red due to blood, making it difficult to identify the bleeding point. In such situations, RDI allows for the identification of bleeding points and the flow of blood through variations in color intensity.
The use of such image enhancement techniques enables a more detailed assessment of small bowel lesions.
Conclusion
The use of the SIF-H190 improves the approach to the small intestine, which is still challenging. It is expected to be utilized for deep small bowel lesions, enabling accurate diagnosis, assessment, and even treatment with minimal invasiveness.
Dr. Mohan Ramchandani Cases 3: Small Intestinal Lesions in Crohn's Disease
Dr. Takahiro Ito
- Keyword
- Content Type