Basic concepts
Making a good operating field
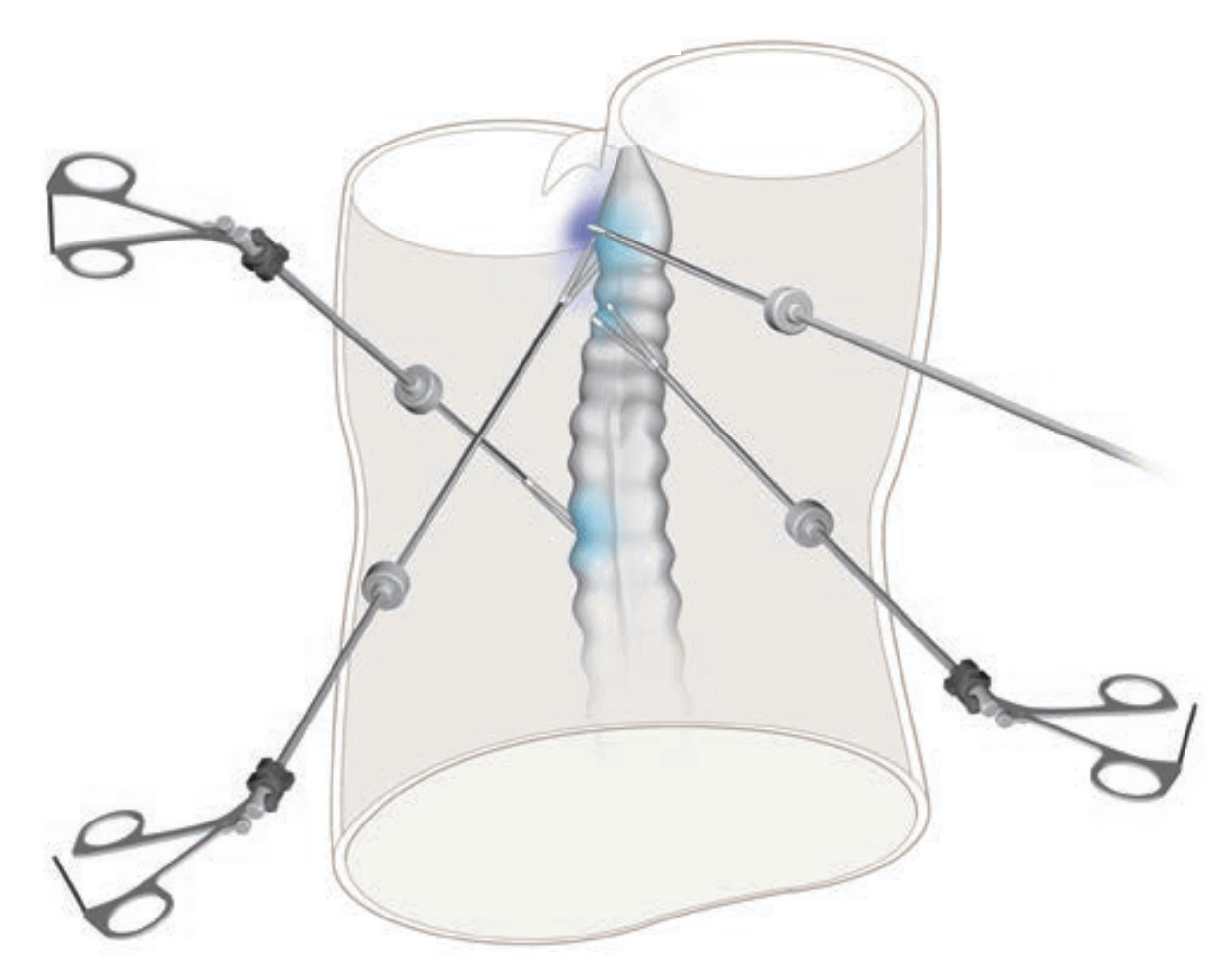
The tissue triangulation is the principle to making a good operating field. The assistant creates a large plane by grasping the tissue at two points, and like a matador waving a red cloth, widens the distance between the two points not to produce slack in the plane. The operator uses both hands freely and performs the dissection while grasping a third point in order to apply tension at the point of dissection. Since it is easy to misinterpret the anatomy during the operation in the pelvic if the sigmoid colon is kinked, the assistant grasps the epiploic appendages of the sigmoid colon using the intestinal forceps with the left hand, and, using lever movements, straightens the sigmoid colon. It is often effective for making a good view in the deep pelvis to open the intestinal forceps widely, like V-shape, and apply it on the dissecting plane with a little traction. We call it “V-shape maneuver”.
The basis of dissection
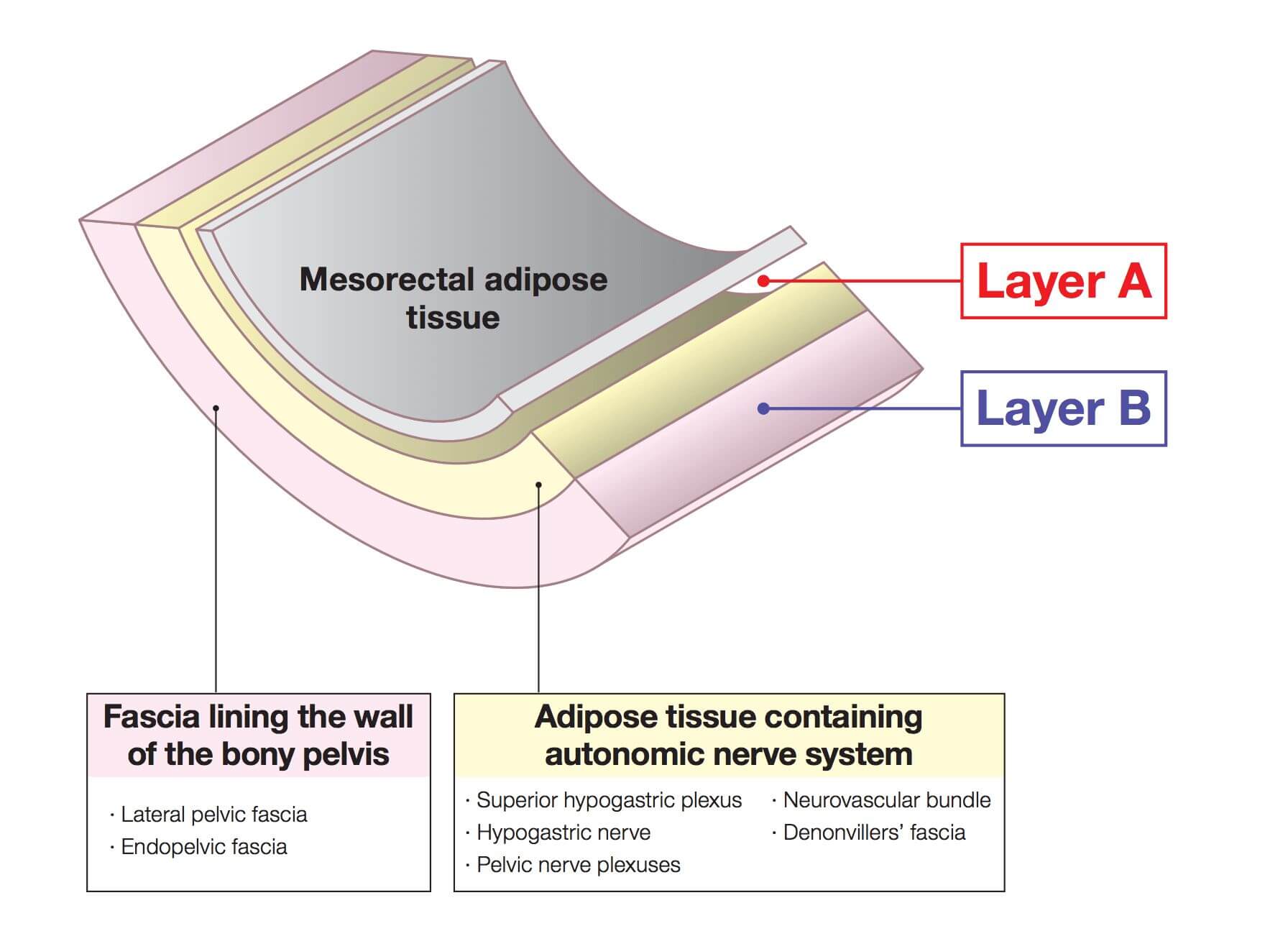
The colon is a long organ and attached to various surrounding tissues. Therefore, during resection, the concept of a “dissection layer” becomes very important. The dissection layer is composed of loose connective tissue of variable thickness, and the dissection that takes place here follows the principle of “a sharp incision in the middle of the loose connective tissue.” Of course, blunt dissection during laparoscopic colon surgery is also effective, but limited to the perirectal dissection in the pelvic cavity, sharp dissection is fundamentally better than blunt dissection. Sometimes, to aid recognition of the dissection layer, “peeking” blunt dissection is effective, but the basic technique to be applied is “sharp incision in the loose connective tissue.” In addition, it is important to establish a strategy for selecting the most appropriate dissection layer depending on the cancer status, using preoperative diagnostic imaging. Another important point is to dissect with a clear understanding of where the adipose tissue that appears during dissection belongs, because a dissection layer exists between two neighboring adipose tissues. The adipose tissue that appears during colon cancer surgery includes the mesenteric adipose tissue, the perirenal adipose tissue, the adipose tissue containing the pelvic nerve plexuses, the adipose tissue surrounding urinary bladder, and the omental adipose tissue. If one understands the “characteristics of the adipose tissue” that will come into view during dissection, it is possible to find a correct dissection layer between two neighboring adipose tissues. It is also important to “dissect with purpose when dissecting the adipose tissue.” When dissecting without purpose and thus dissecting haphazardly across the adipose tissue, not only are the surgical procedures inaccurate, but excessive exudate is produced by the injured adipose tissue, and this can cause inadvertent obscuring of the anatomy. It is most important to bear in mind that when dissecting the adipose tissue, there should be clear purpose, such as to divide mesentery, to resect extendedly surrounding tissue for good margin, and so on.
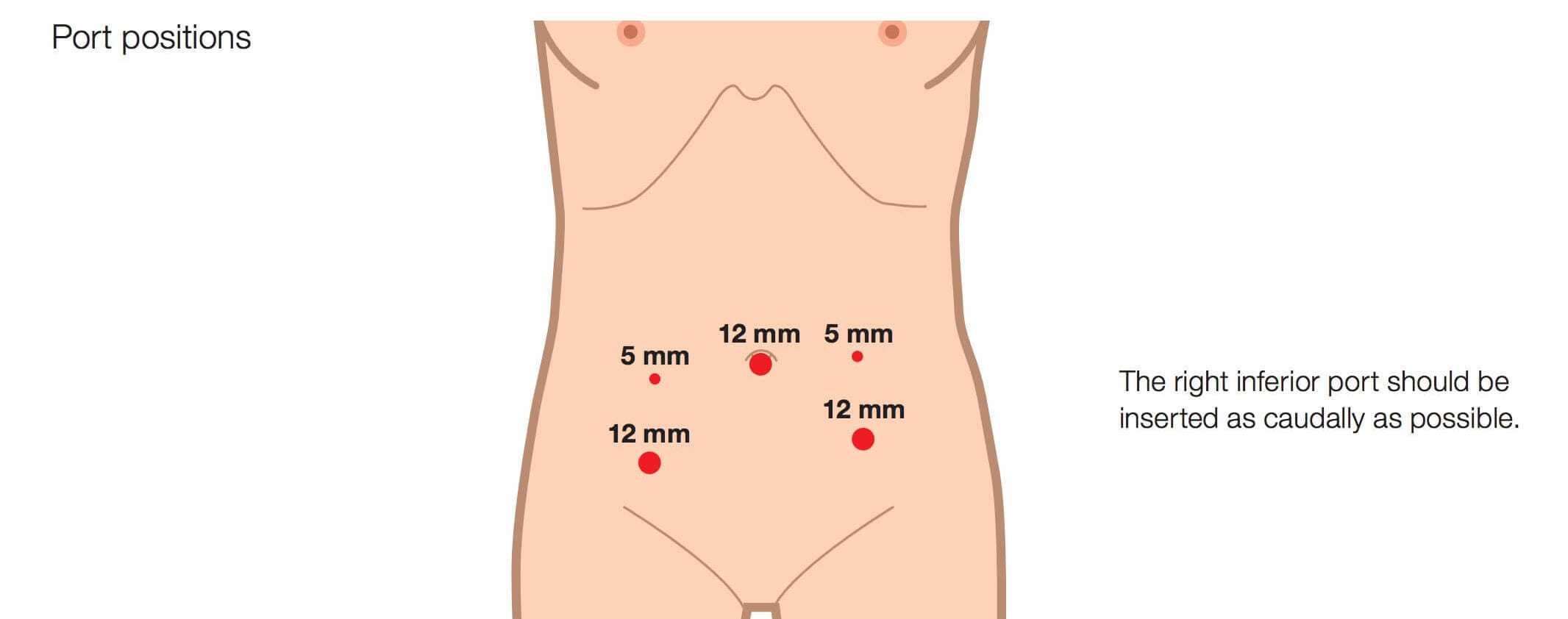
Low anterior resection of the rectum performed with a 3D flexible videoscope
The case illustrated is that of rectal cancer in an obese male patient. Intrapelvic dissection was performed on the basis of the images displayed during laparoscopy.
1.Anatomical diagram of the perirectal area
2.Dissection on the right side | (1) Posterior to lateral
How to make an operating field
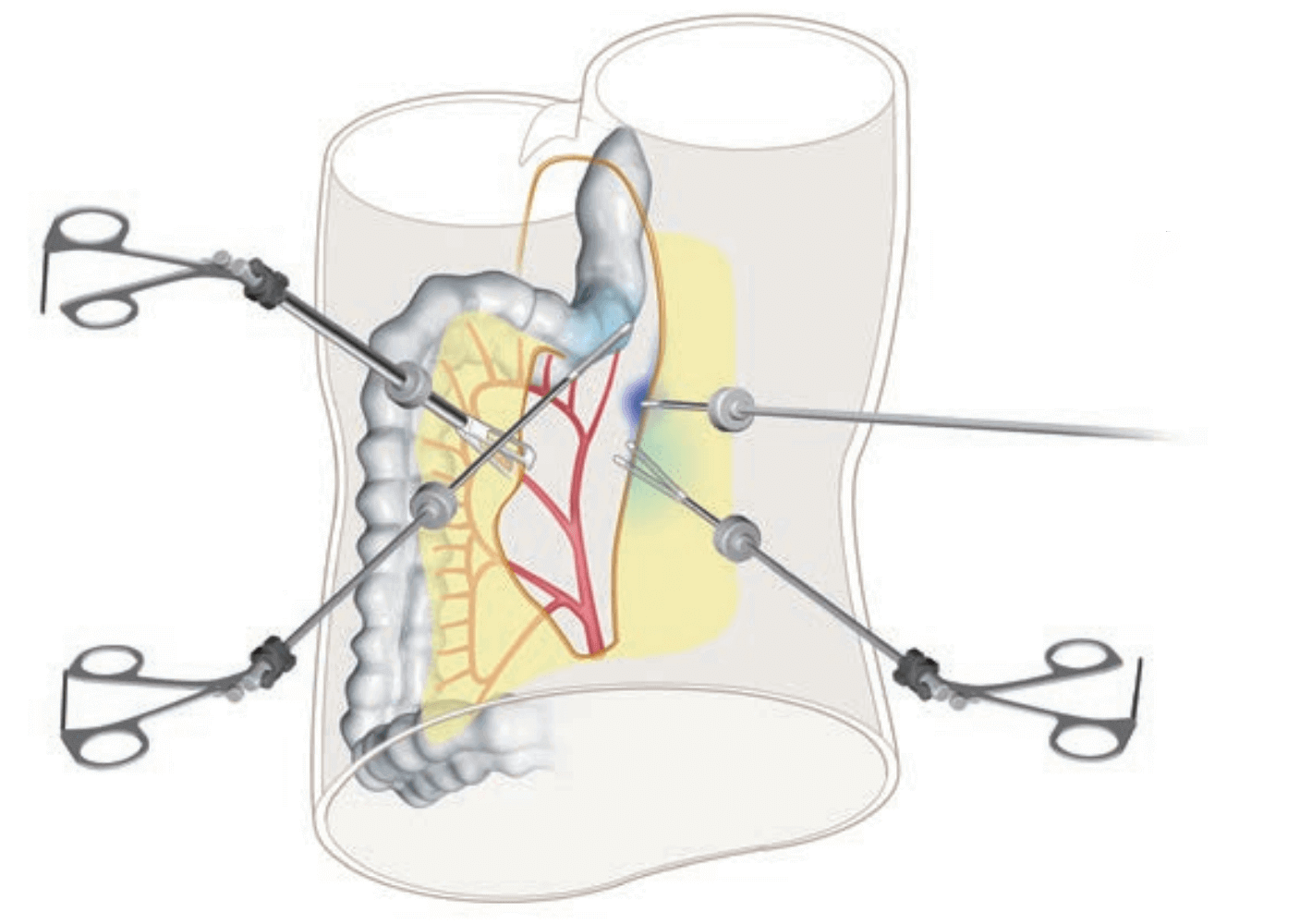
The assistant creates a large plane in the matador-like manner. The operator grasps the pelvic peritoneum and applies counter-traction at the point of dissection.
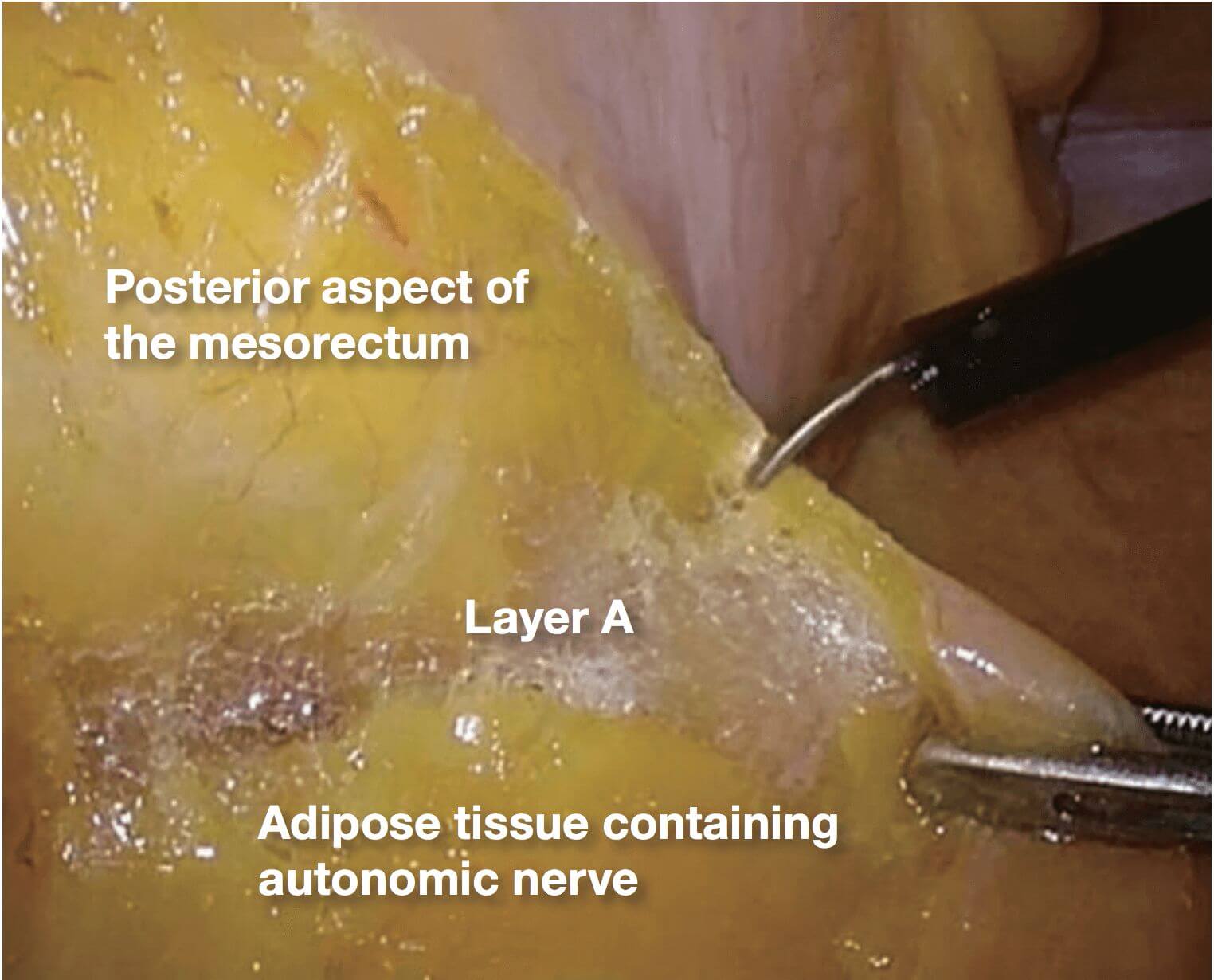
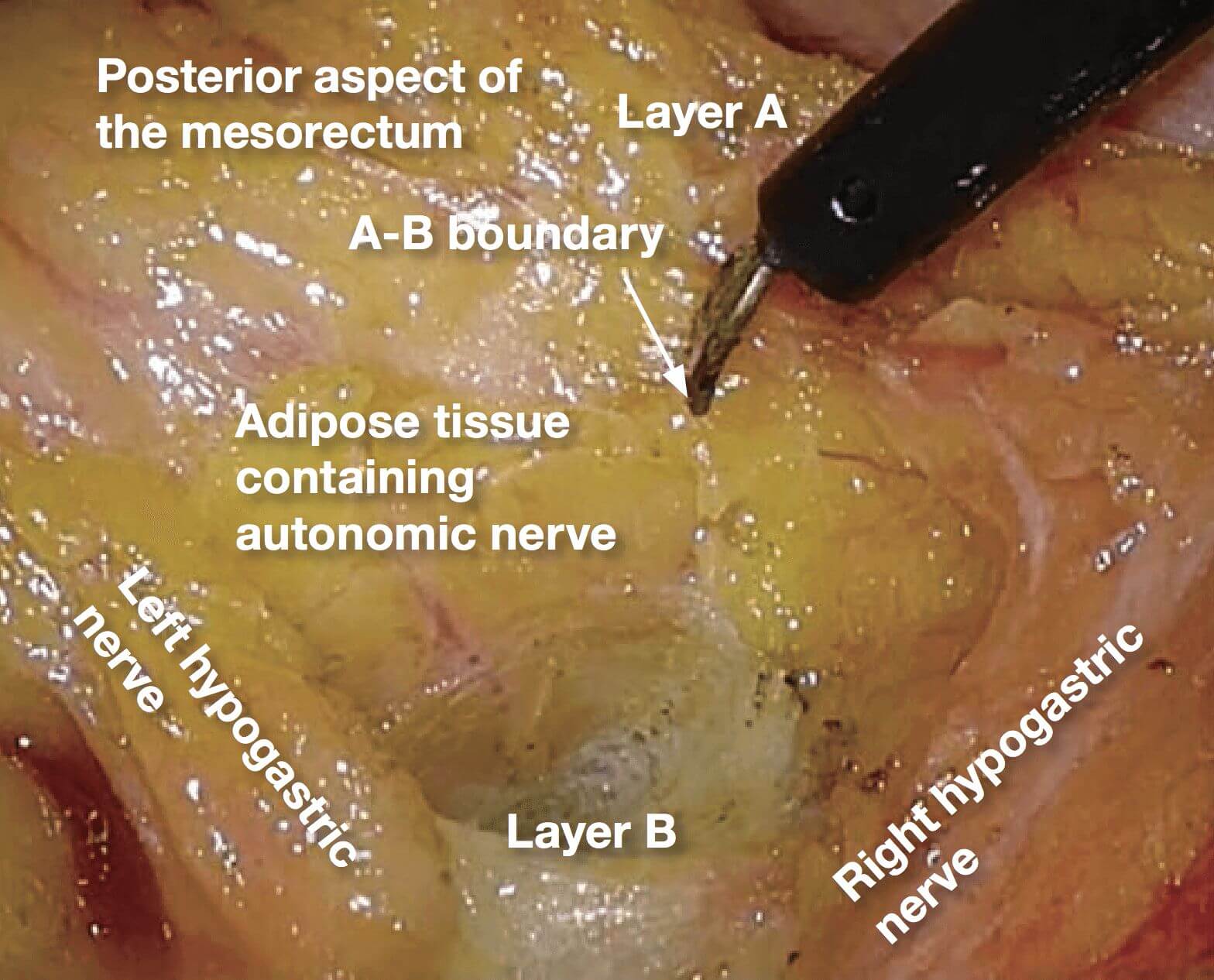
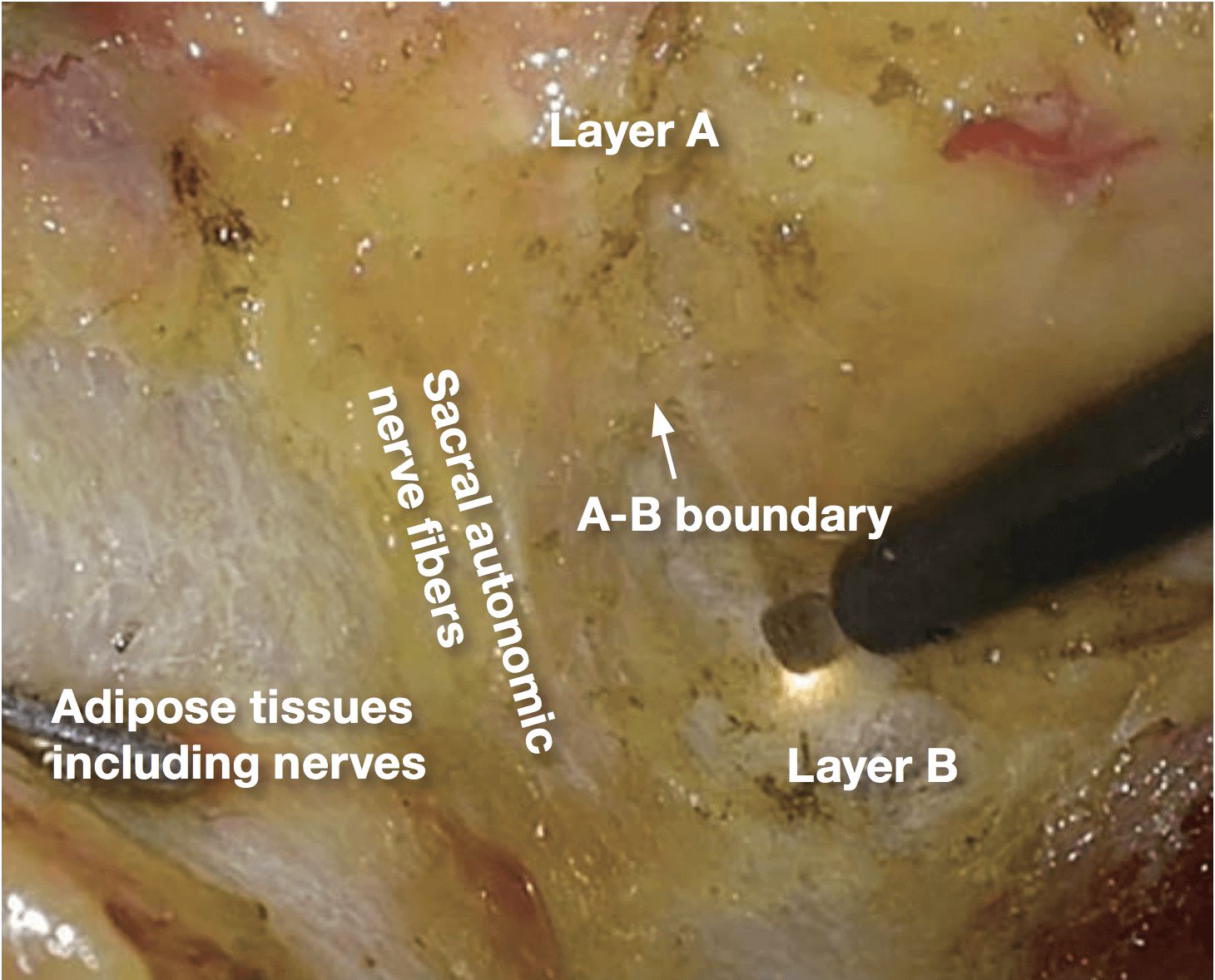
1.The dissection between the posterior aspect of the mesorectum and adipose tissue containing autonomic nerve is being advanced (layer A dissection) until it becomes possible to confirm the right hypogastric nerve.
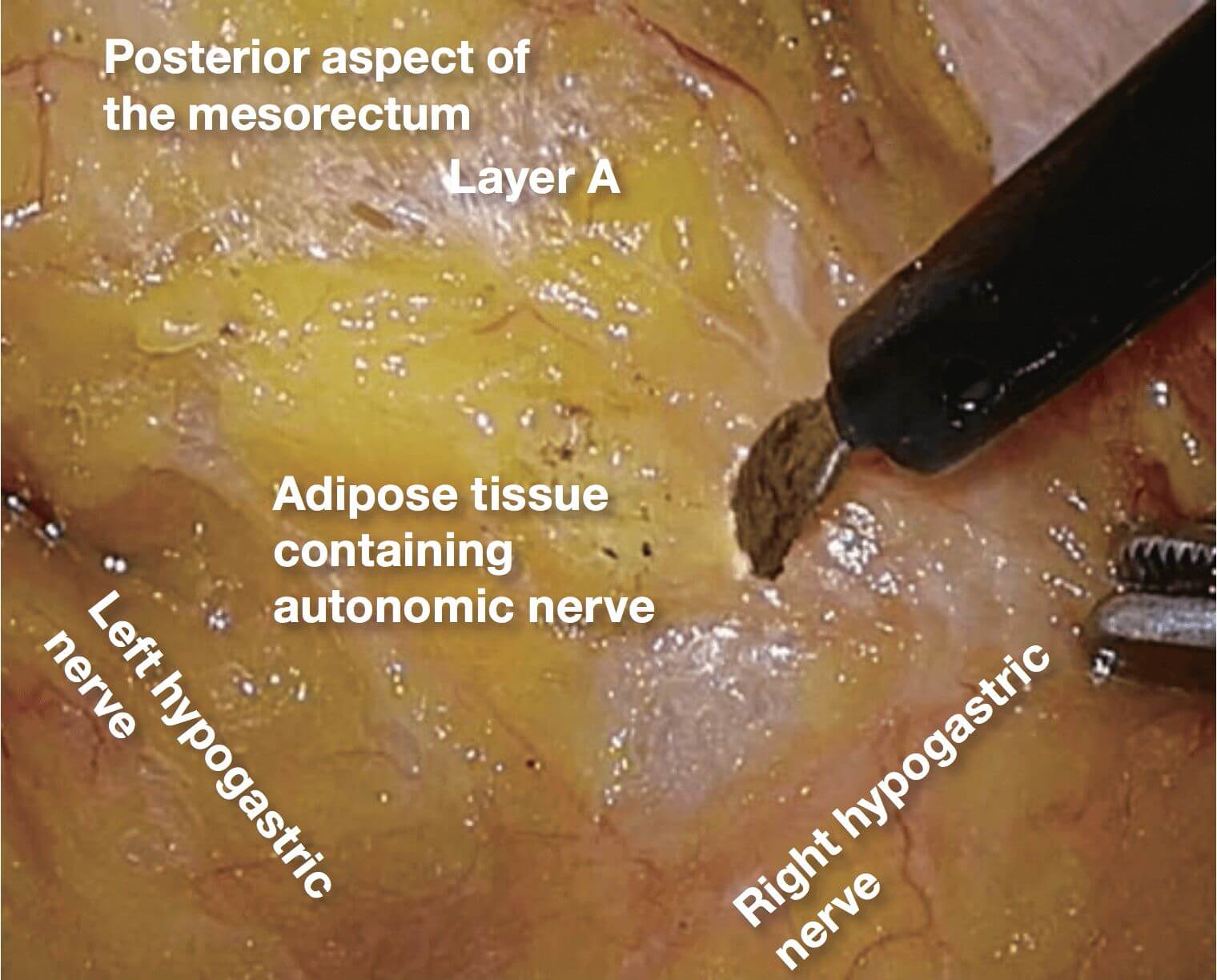
2.When the layer A dissection is advanced, the right hypogastric nerve can be confirmed. (In this case, the nerve on the left was also confirmed.) The adipose tissue medial to the right hypogastric nerve is being divided. It is thick in obese individuals.
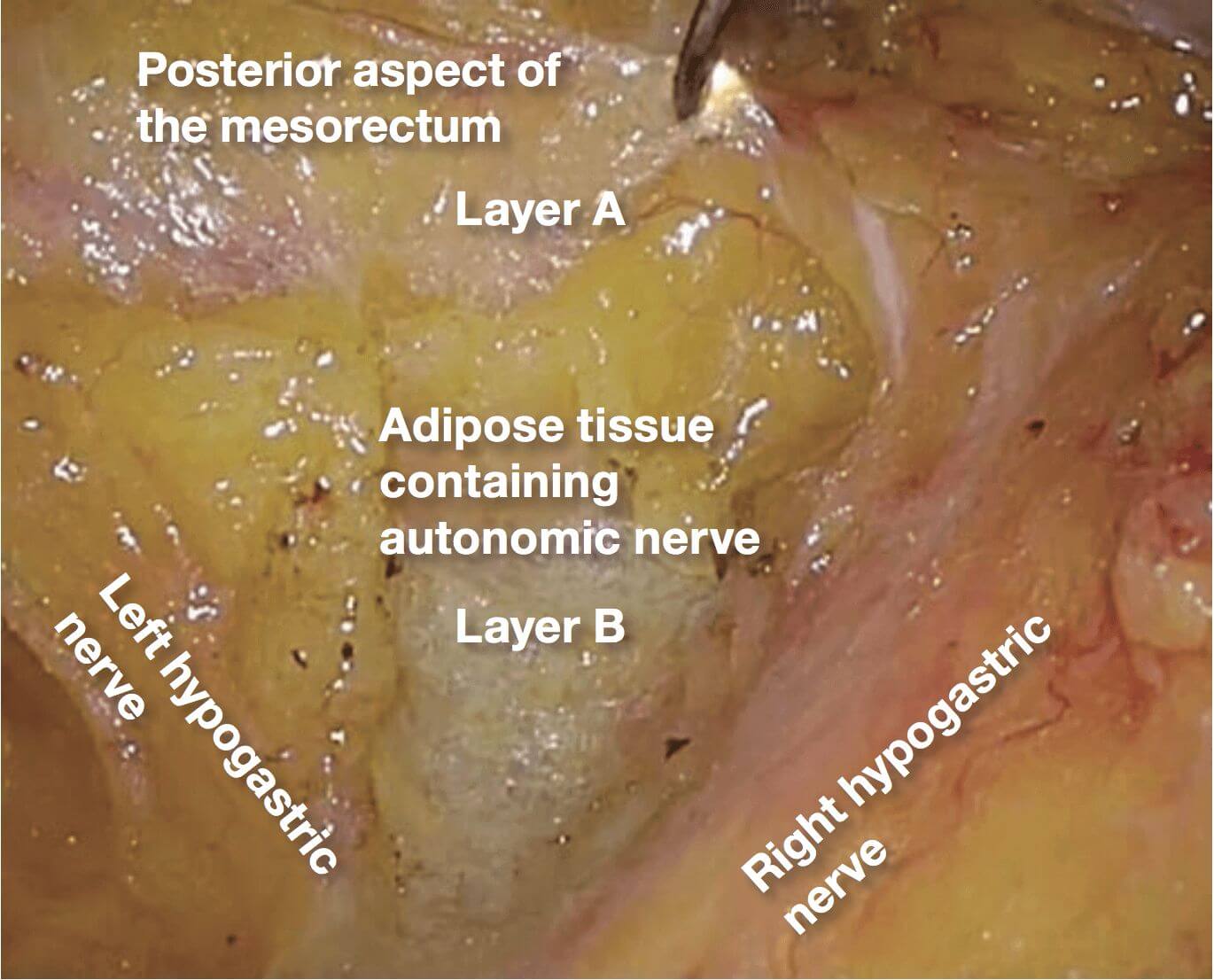
3.The thick adipose tissue is divided until
layer B is reached. Using the 3D videoscope, the loose connective tissue in layer B looks spatially spread.
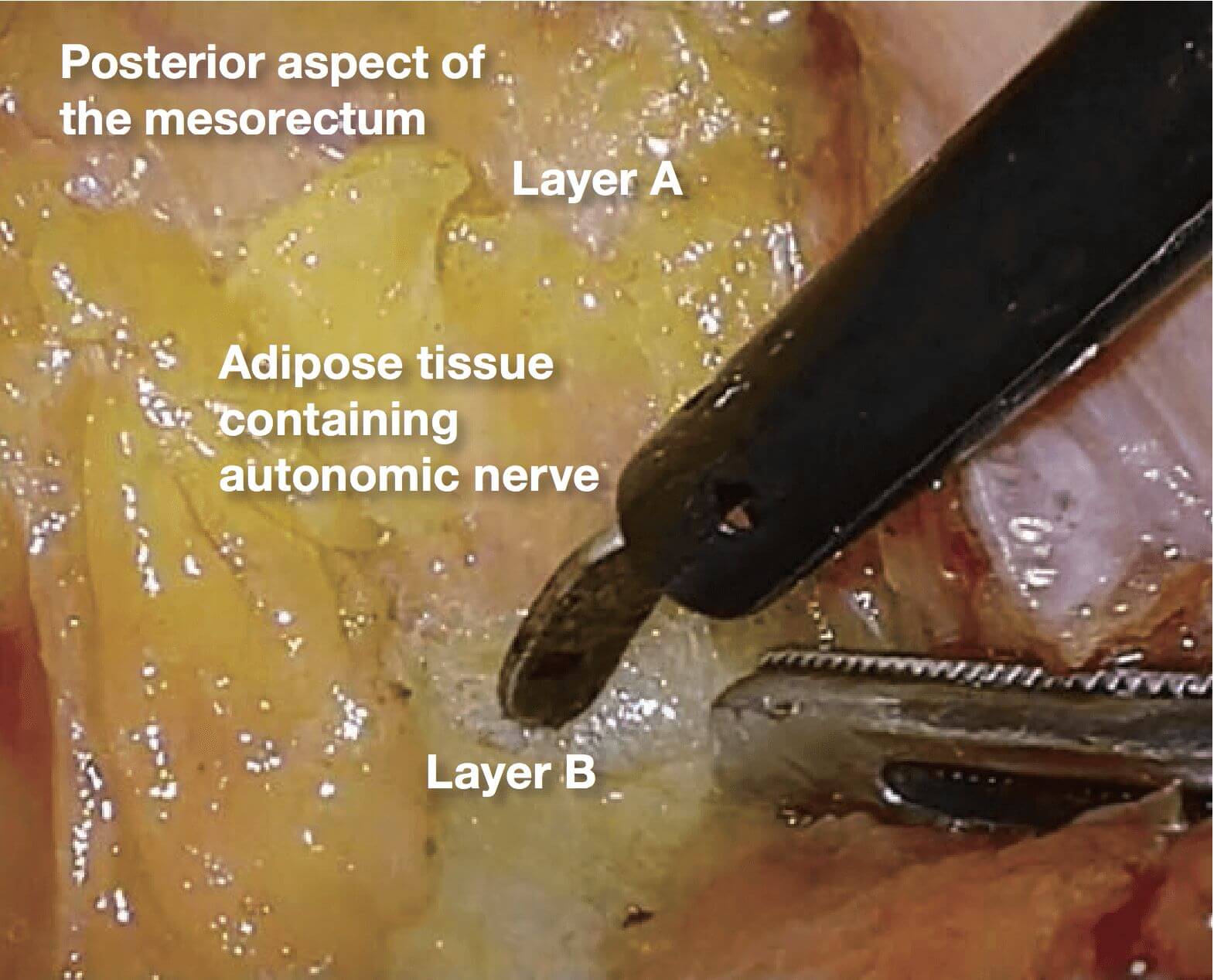
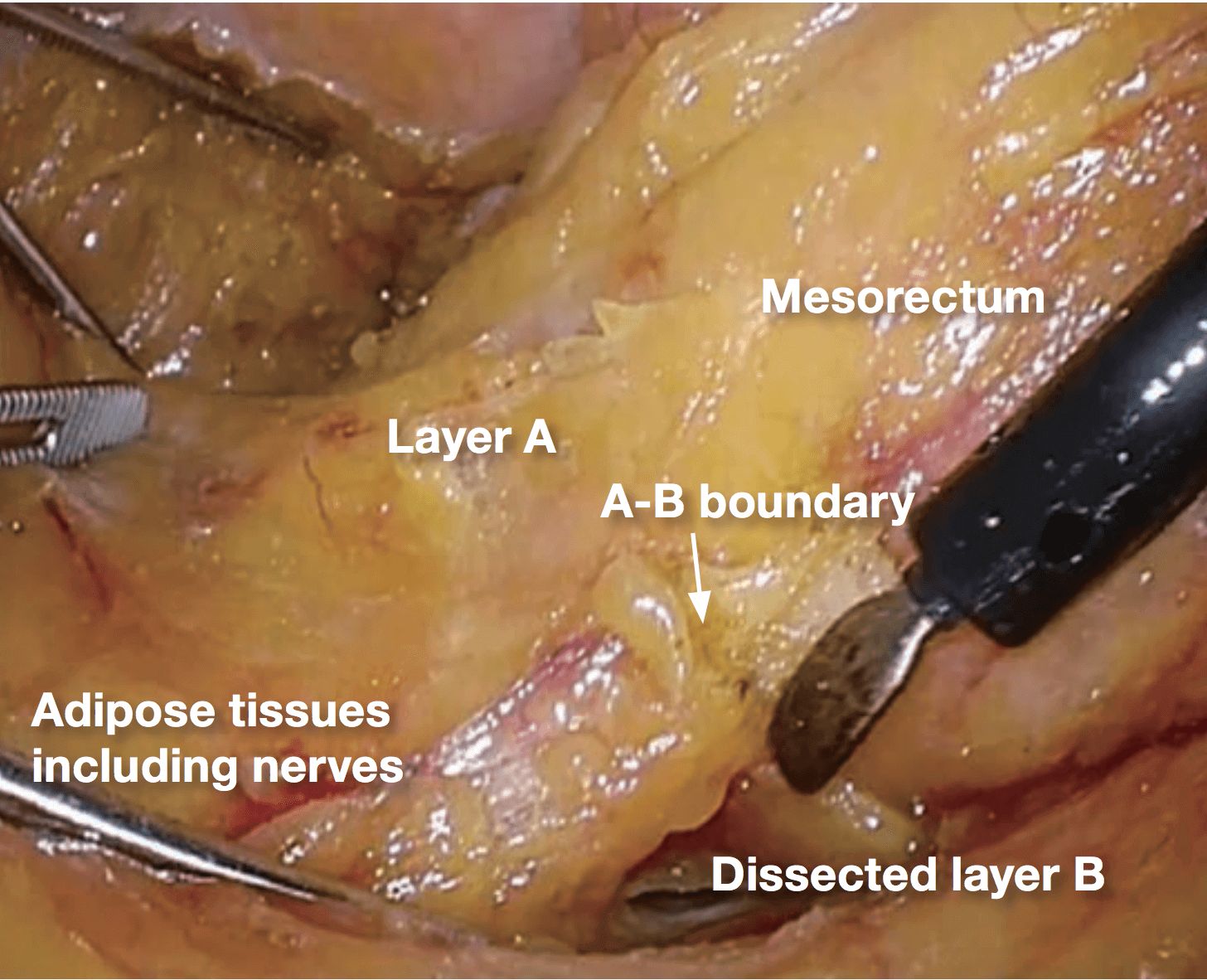
4.Posteriorly, the dissection is advanced in layer B, which is easier to dissect than layer A Dissection is performed at the midline and is not directed toward the left. Dissection to the left here results in inadvertent injury to the left pelvic nerve plexus.
Laterally, the dissection in layer A is necessary to preserve pelvic nerve plexus. Therefore, from posterior to lateral, the dissection layer should be shifted from layer B to layer A. In this procedure, A-B boundary is created, which is same as so- called lateral ligament.
2.Dissection on the right side | (2) Lateral to anterior
How to make an operating field
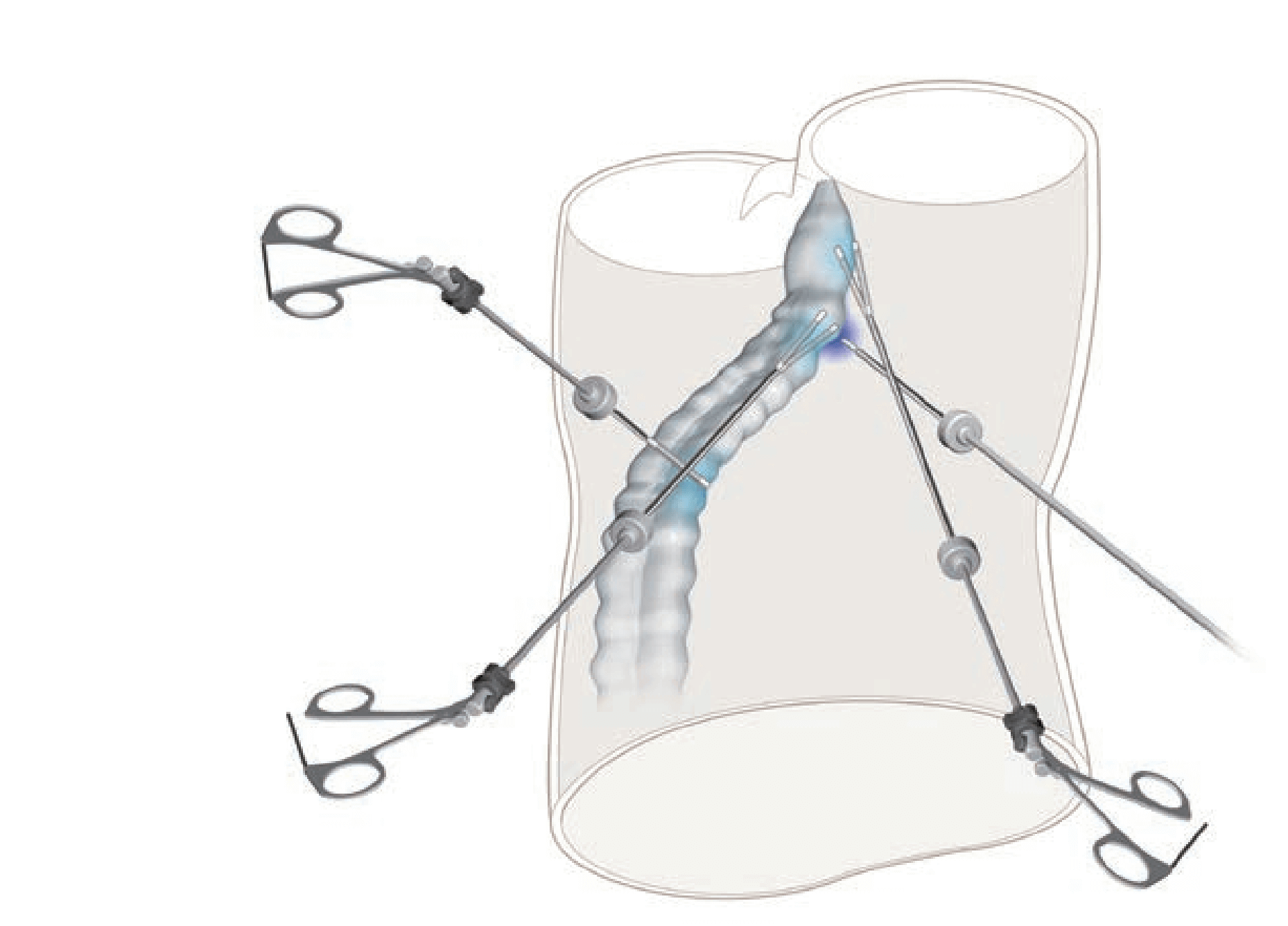
The assistant applies traction to the rectum (levering). The operator exposes the pelvic side and applies countertraction at the point of dissection. Generally speaking on laparoscopic surgery, care must be taken to make operating field so that the forceps do not cross in front of the camera. Oth- erwise, the forceps may disturb the view. This disturbance is emphasized with a 3D scope, so more attention should be paid when a 3D scope is used.
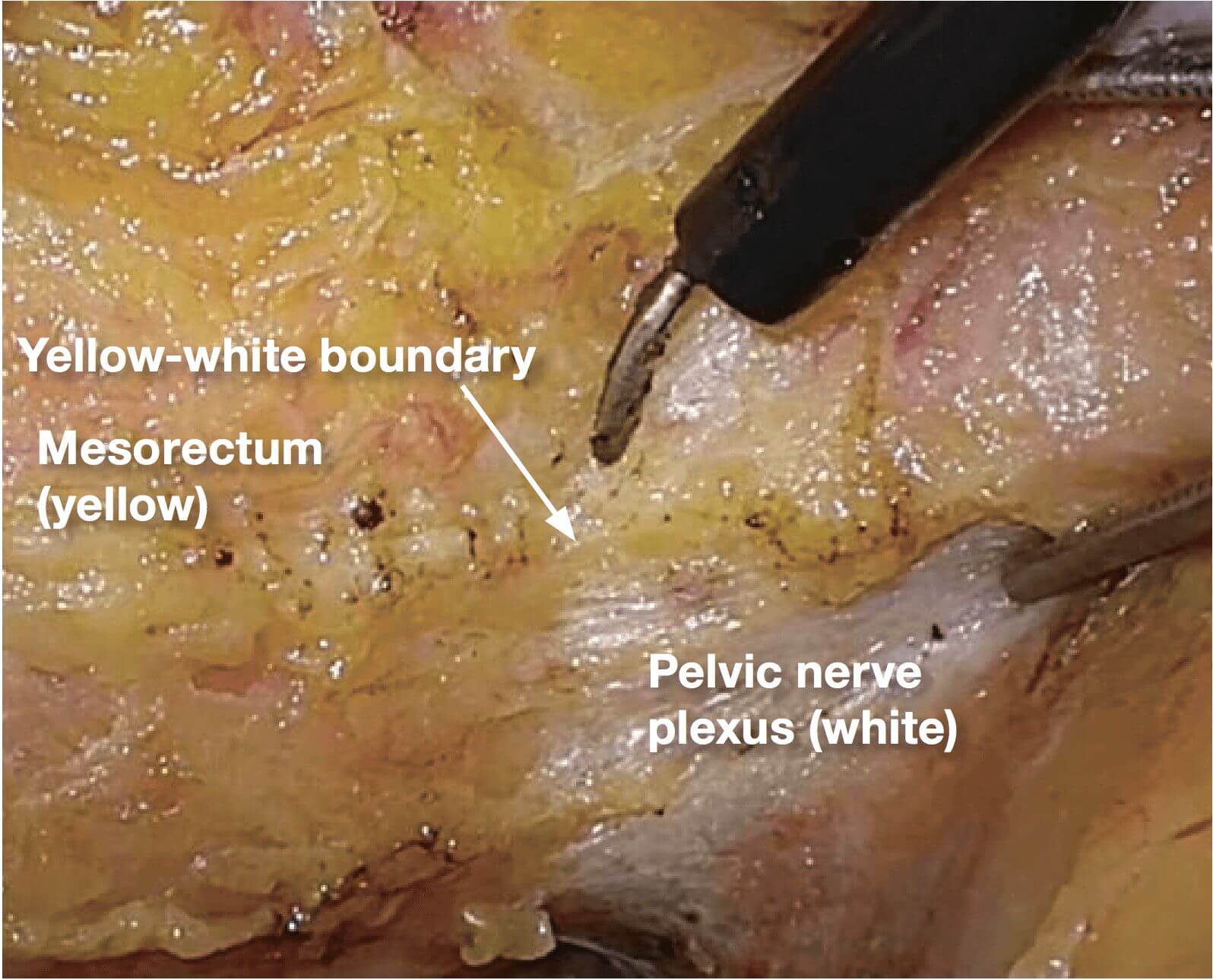
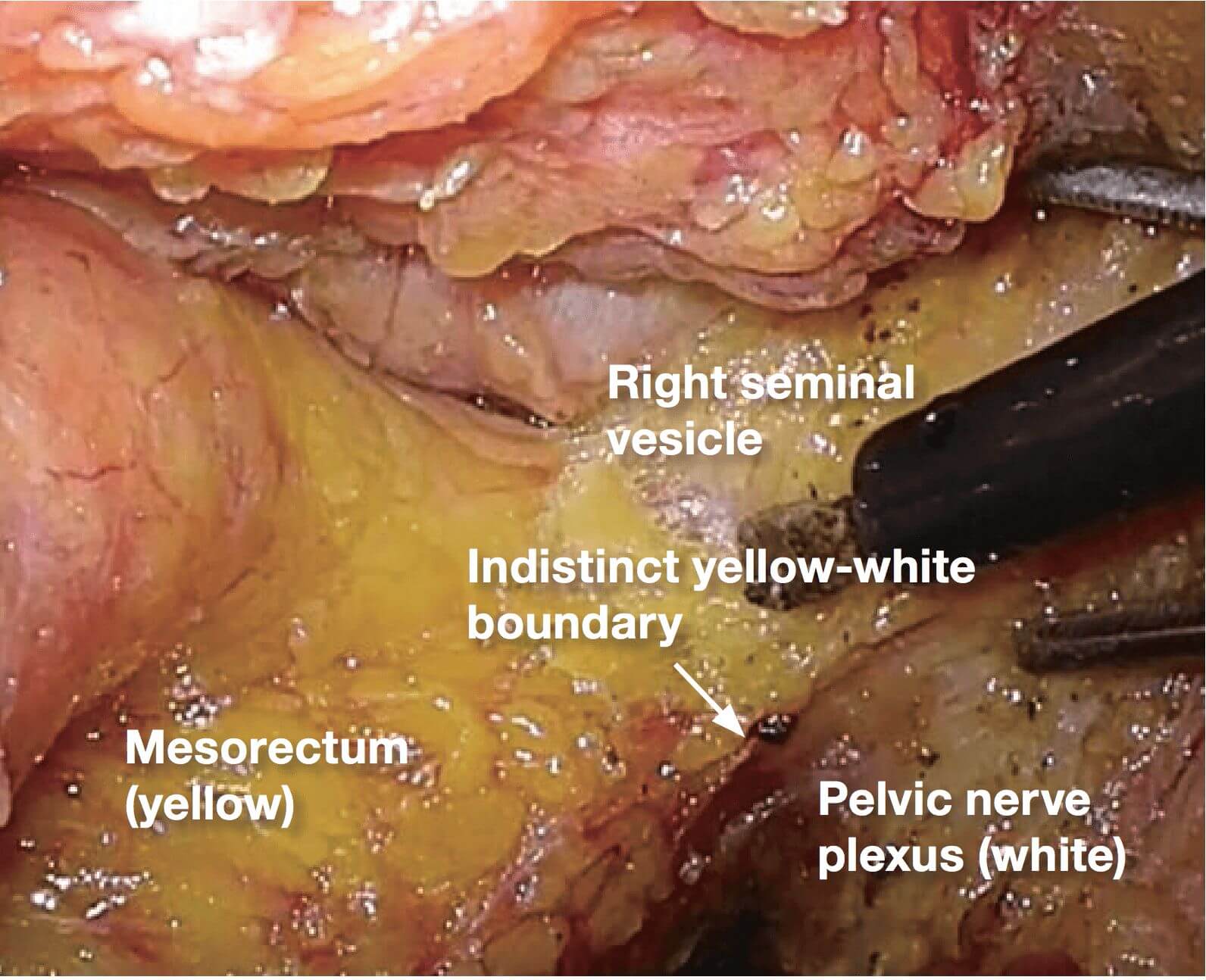
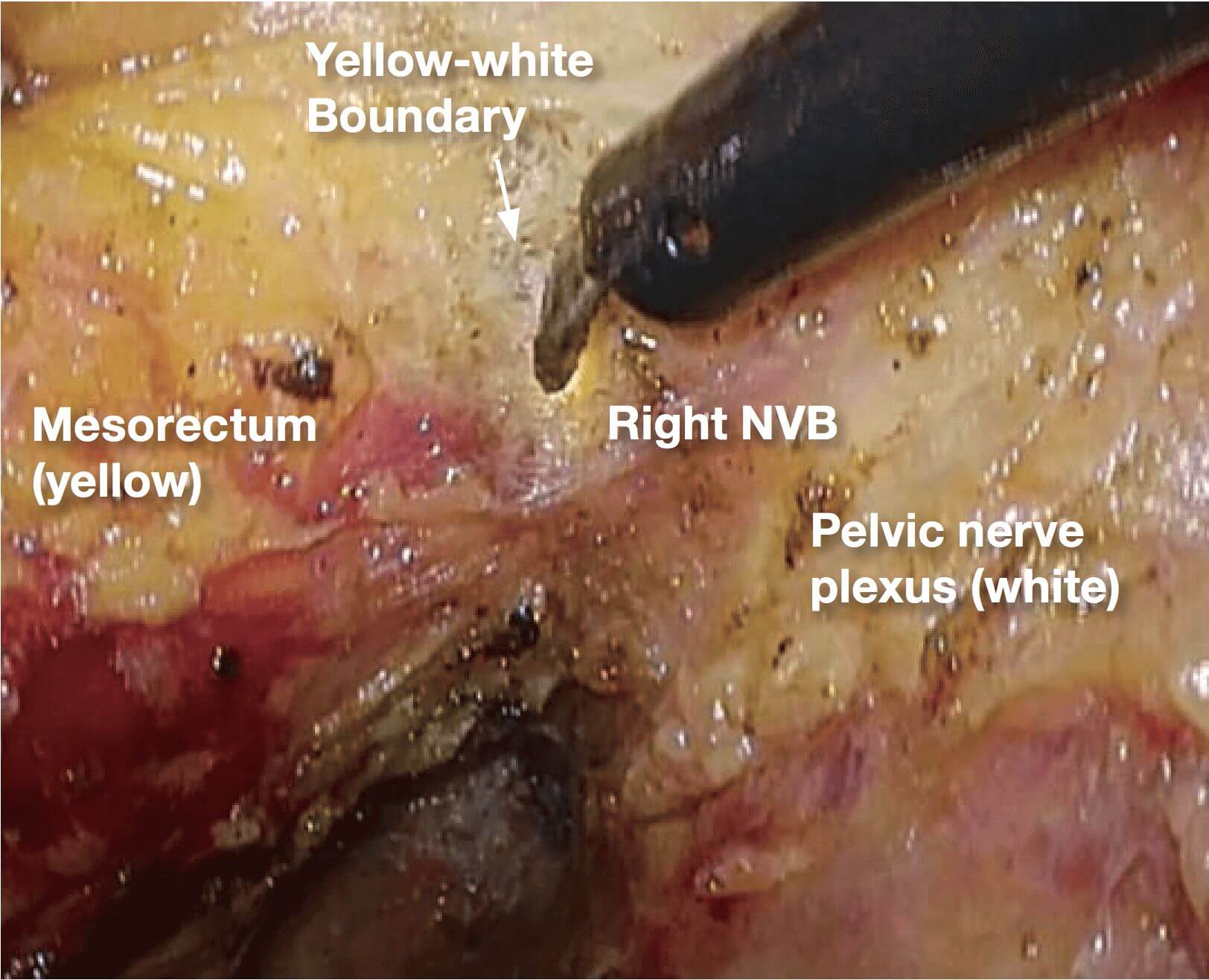
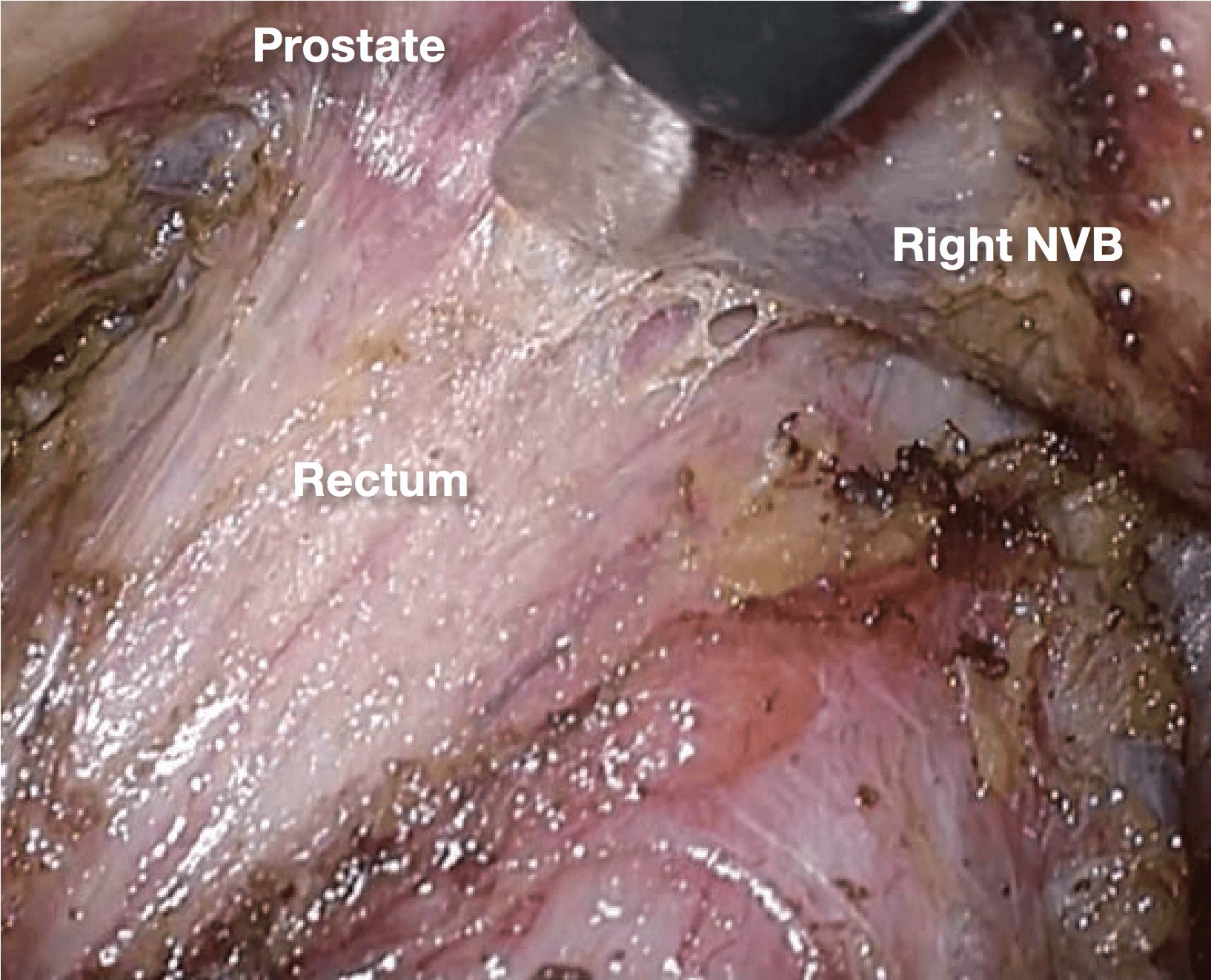
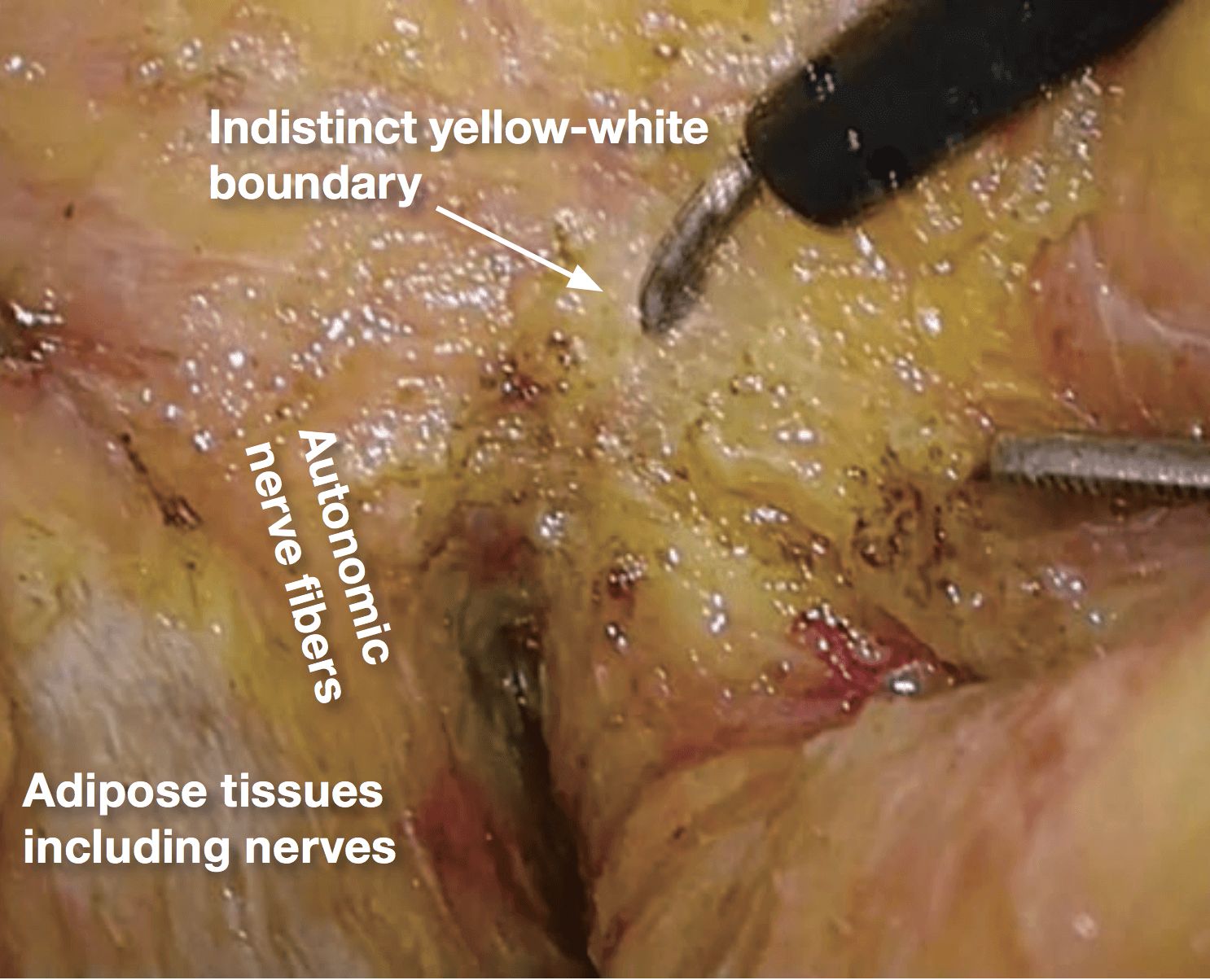
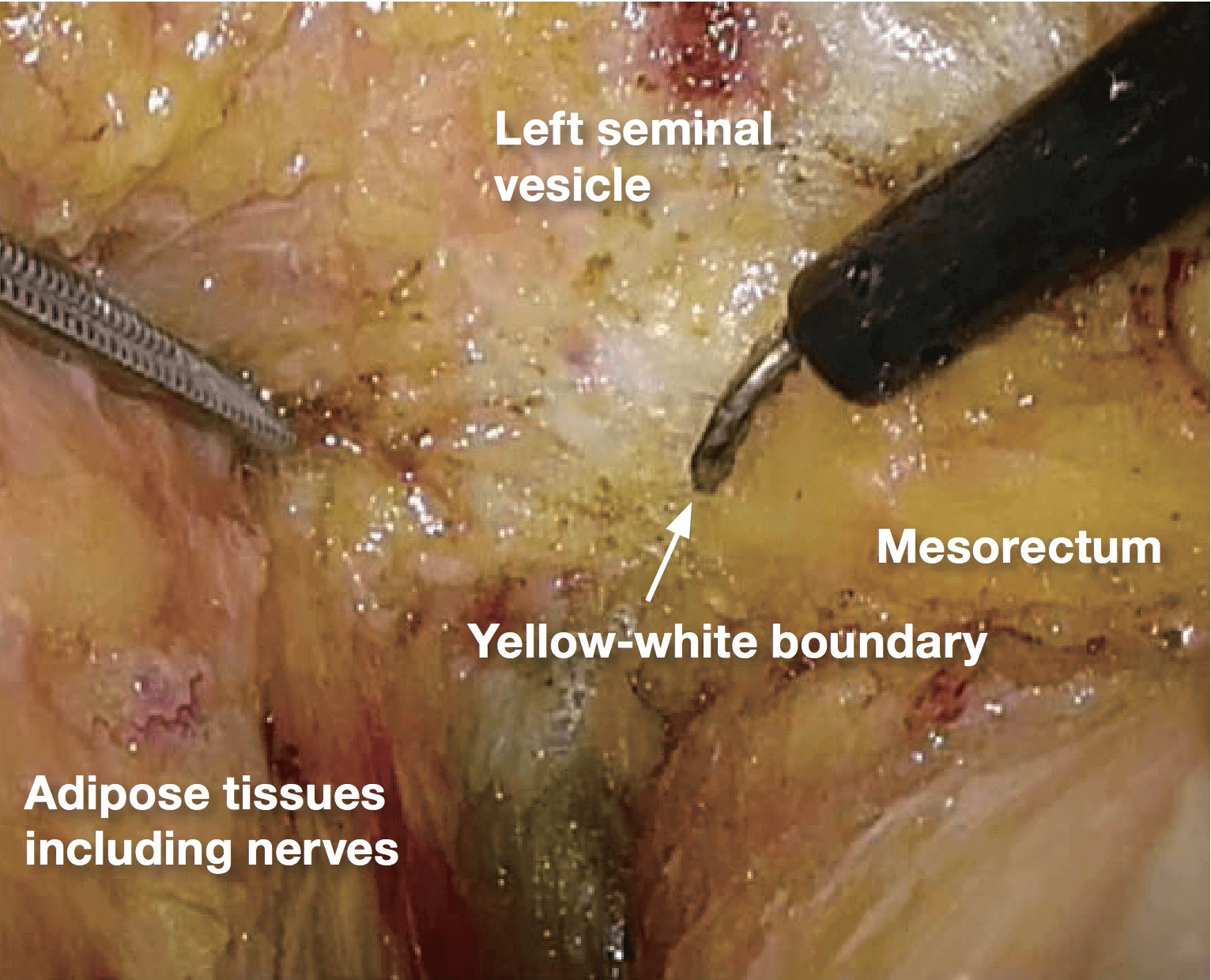
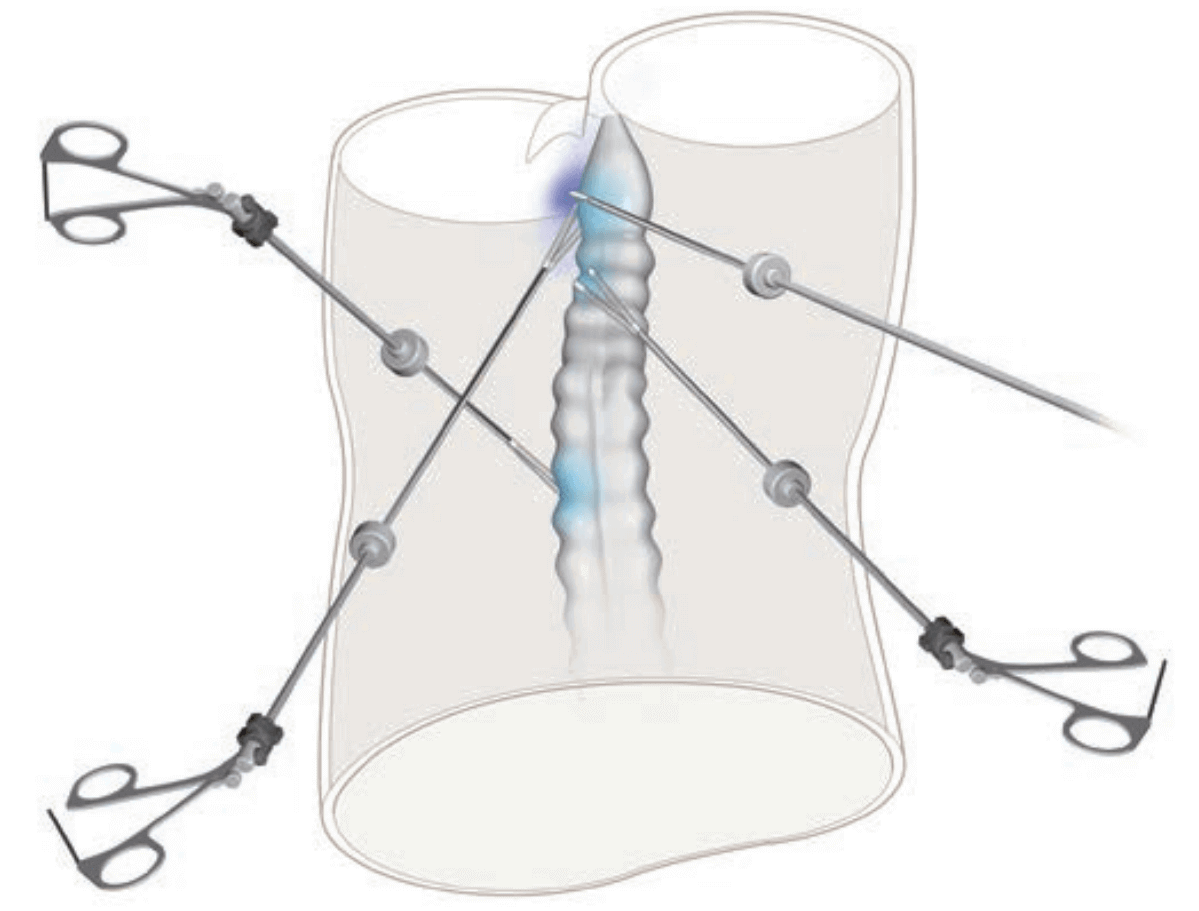
1.Starting posteriorly, dissection of layer A is continued. The nerve bundles are whitish, and the mesorectum is yellowish; therefore, the boundary (yellow-white boundary) can be a landmark of dissection for autonomic nerve preservation. However, the boundary commonly becomes indistinct in the anterolateral direction.
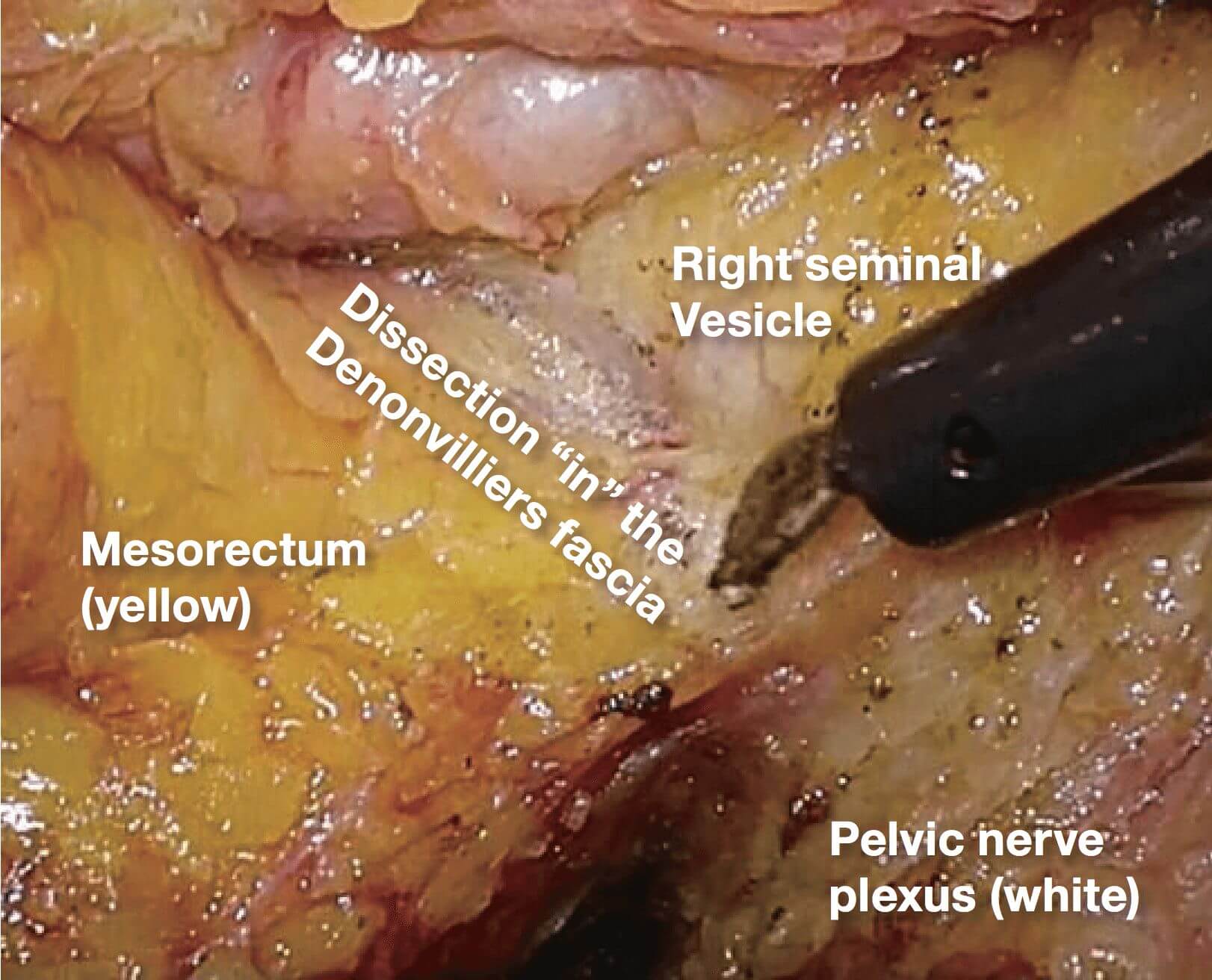
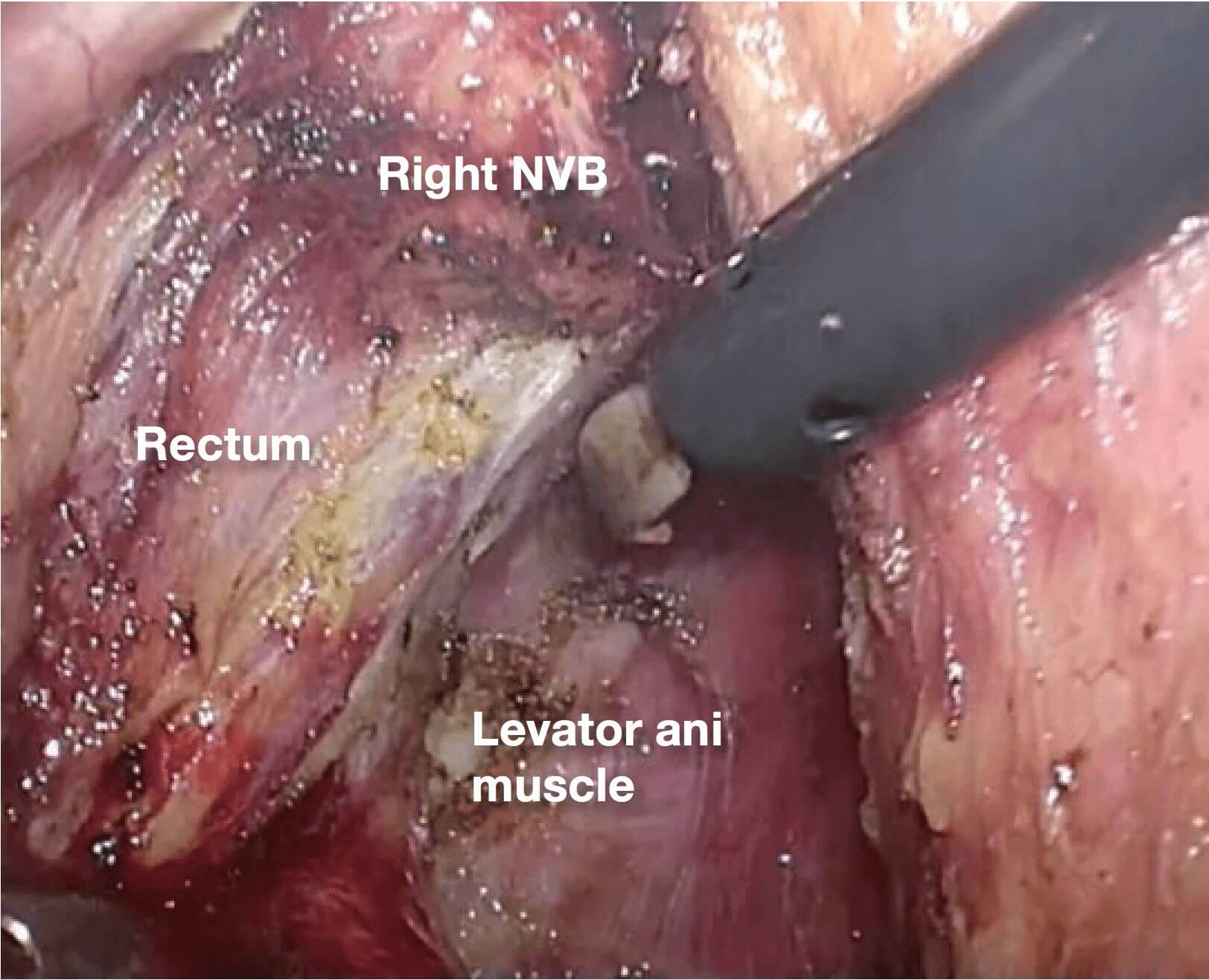
2.(Photographs 2 – 5)
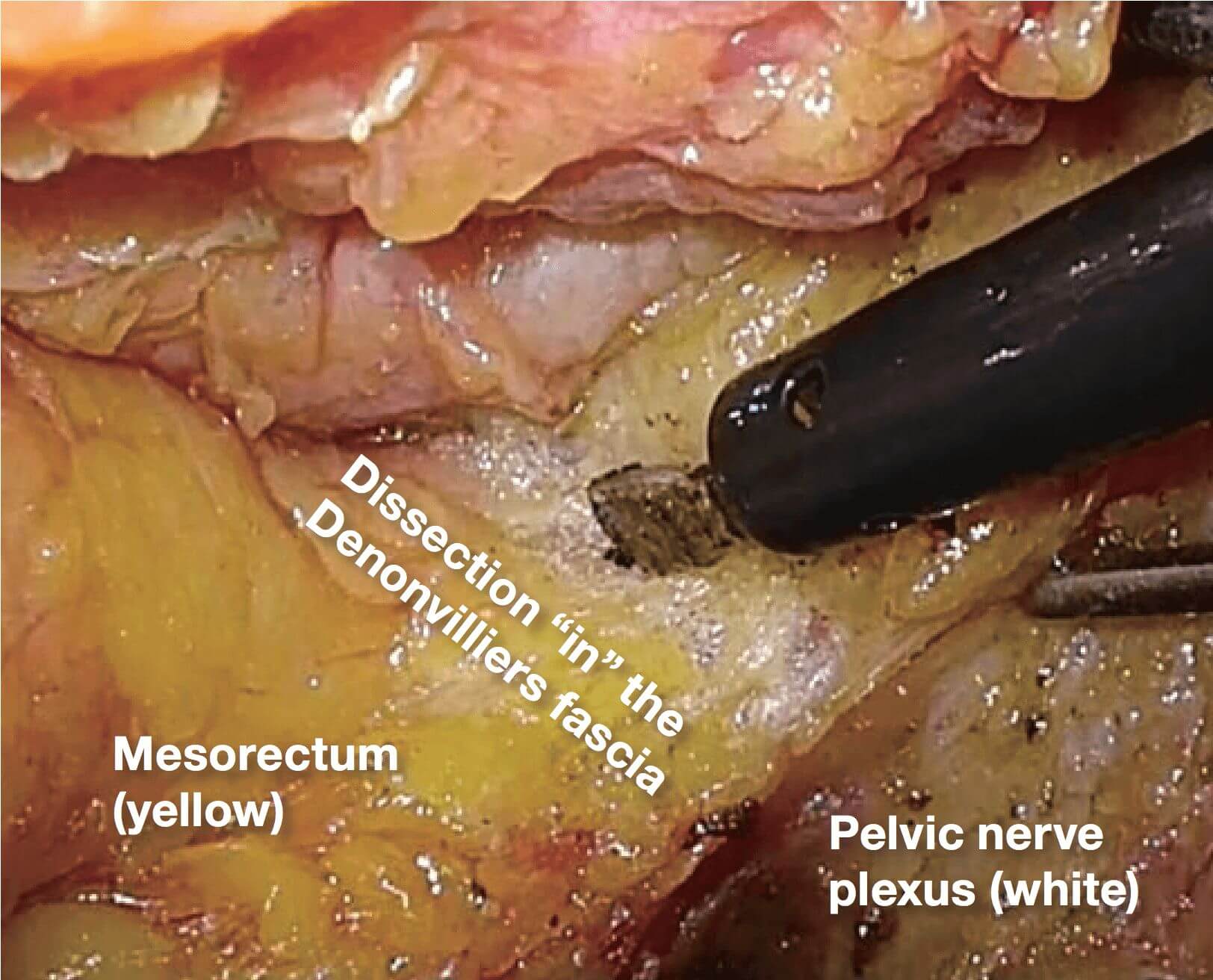
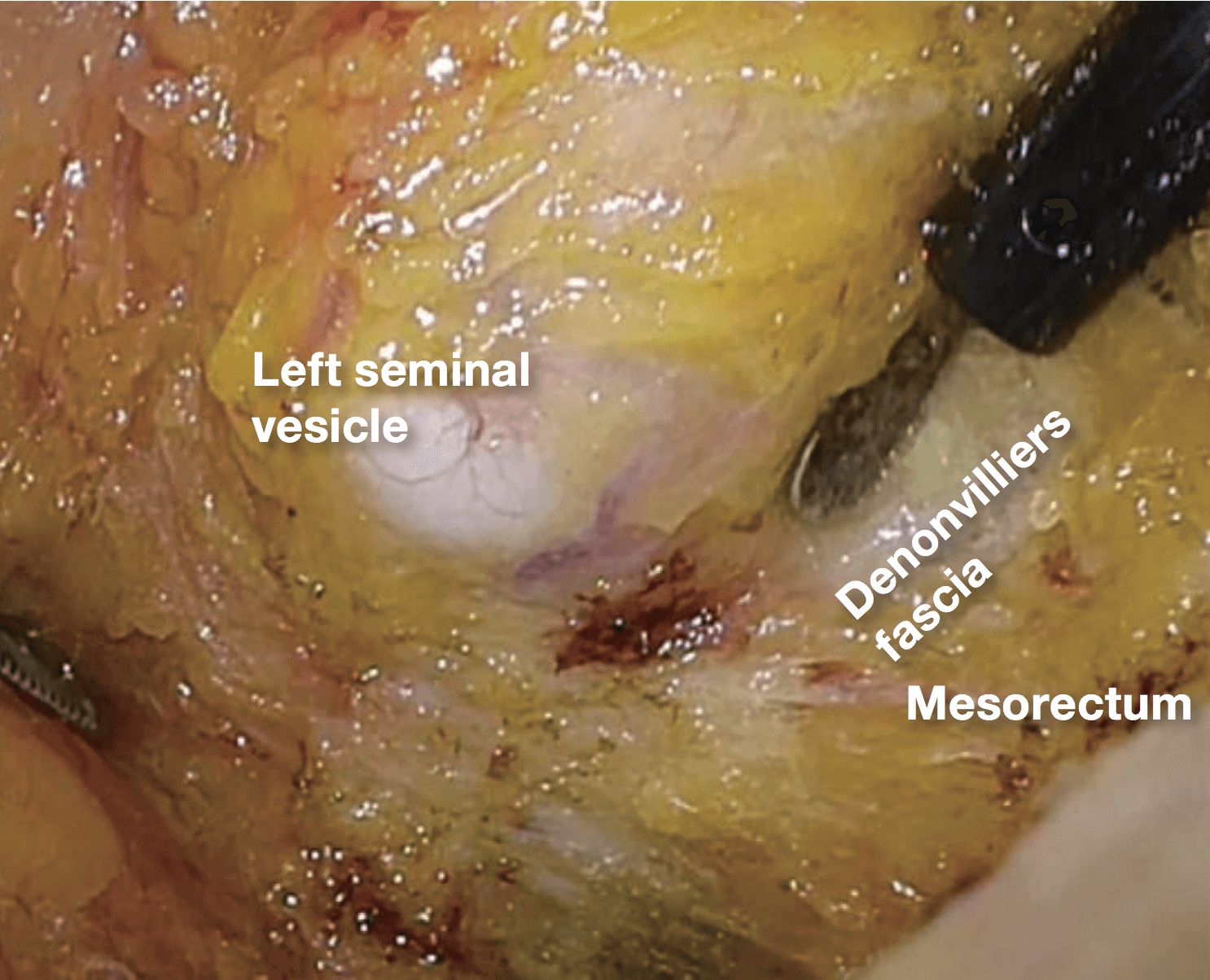
If it becomes difficult to discern the yellow- white boundary, further dissection should not be advanced forcefully. In such a situation, seminal vesicles are good landmarks to confirm dissection layer on the anterior. The Denonvilliers’ fascia lies between seminal vesicles and the mesorectum. Once seminal vesicles are identified, dissection can be made between seminal vesicles and the mesorectum, leaving a small amount of connective tissue around seminal vesicles. In other words, this dissection is advanced “in” the Denonvilliers’ fascia. If the seminal vesicles are excessively exposed, tension may be inadvertently applied to the neurovascular bundles (NVB) medially, that may cause injury to NVB. During this process, the yellow (mesorectum)-white (seminal vesicle, NVB) boundary becomes easy to identify.
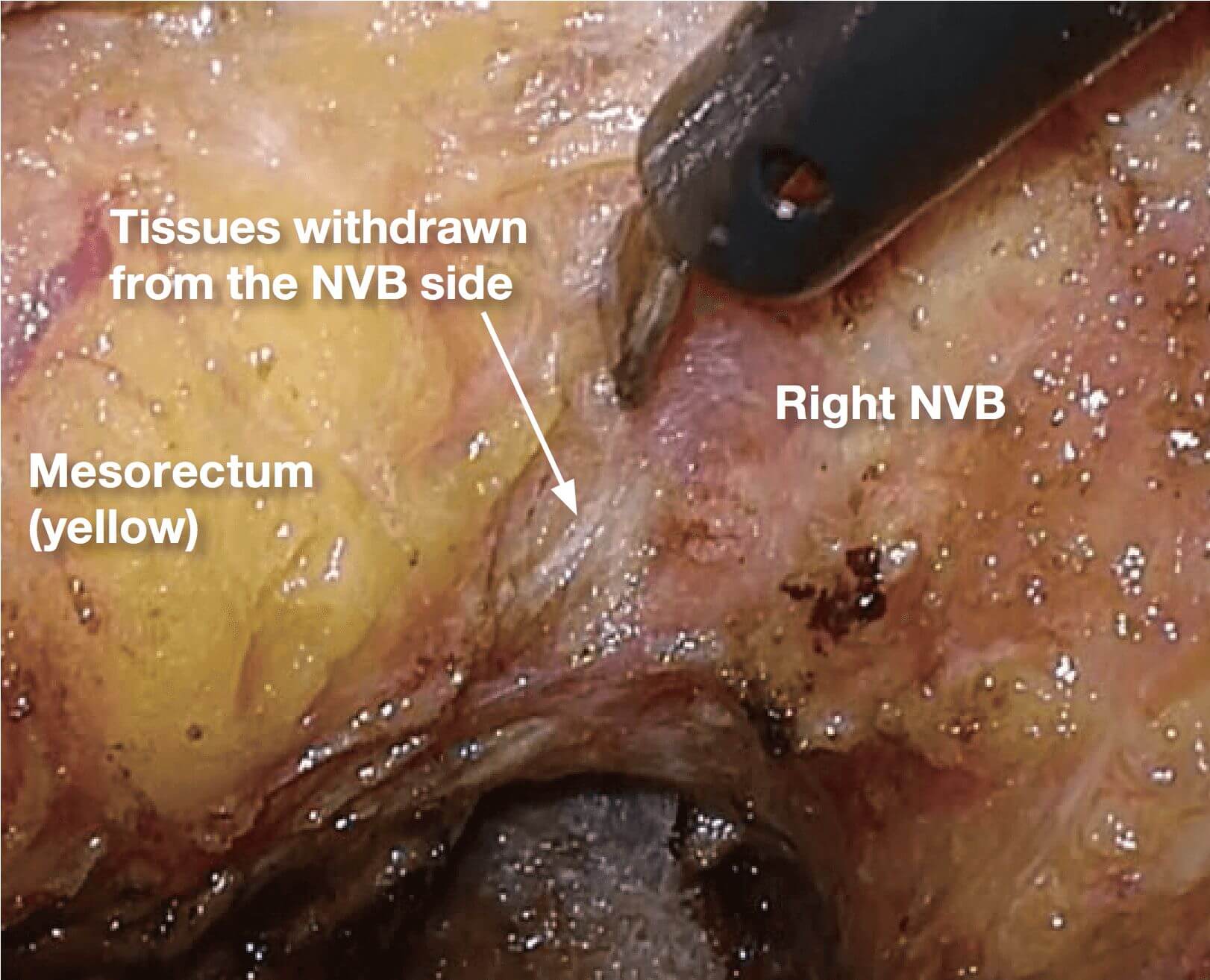
6.Depending on the site and depth of cancer invasion, some adjustment is required for the dissecting plane to move laterally and medially in order to obtain sufficient circumferential resection margin, even during surgery that preserves the autonomic nerves (layer A dissection). If the dissection is made beyond the yellow-white boundary, a part of the NVB is inadvertently pulled out, making the dissection layer difficult to identify. In such a situation, the withdrawn part of NVB should be incised, so that the dissection plane can return layer A (photo 7). It is important to predict the point of return when extended dissection is applied.
7.(Photographs 7 – 8)
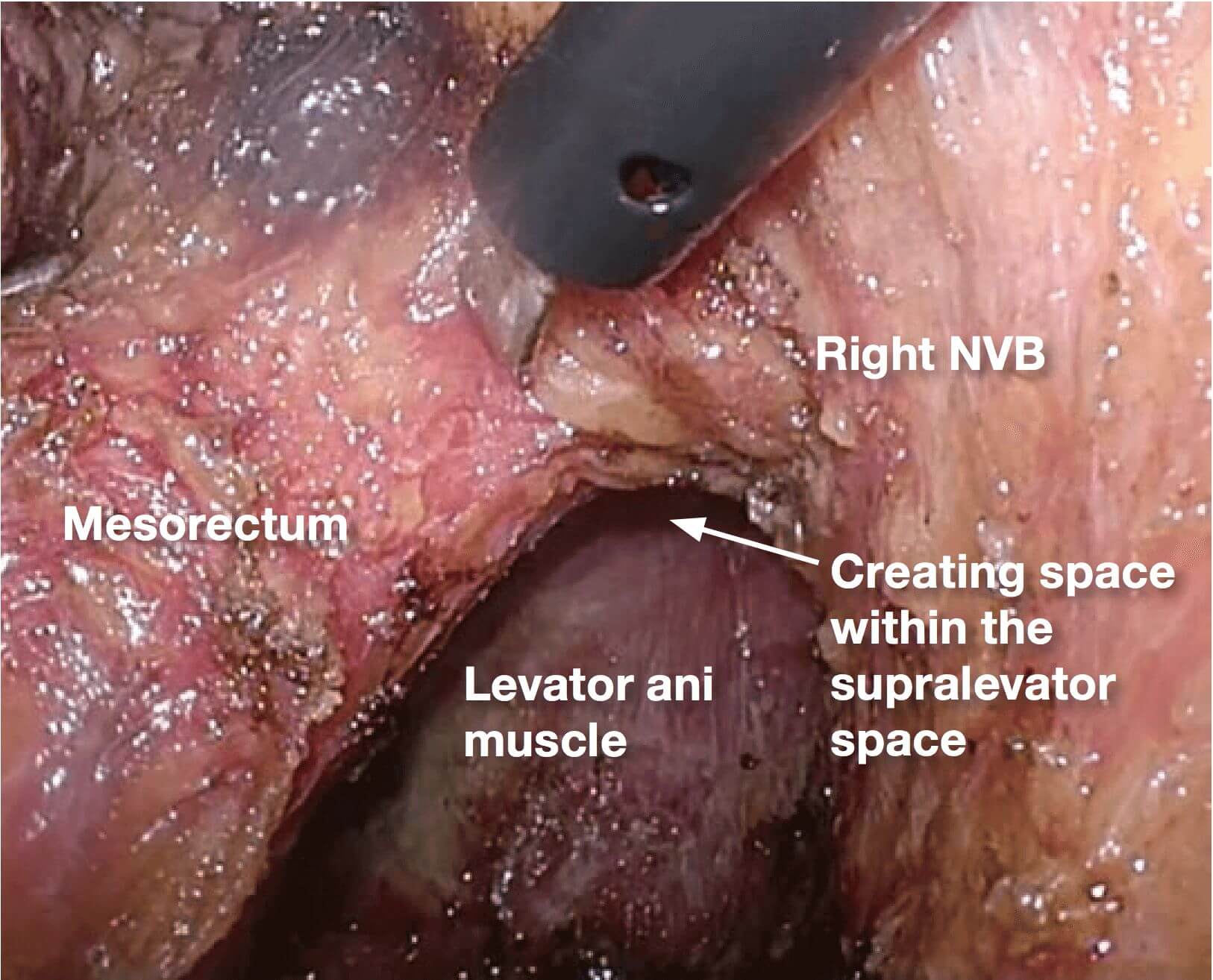
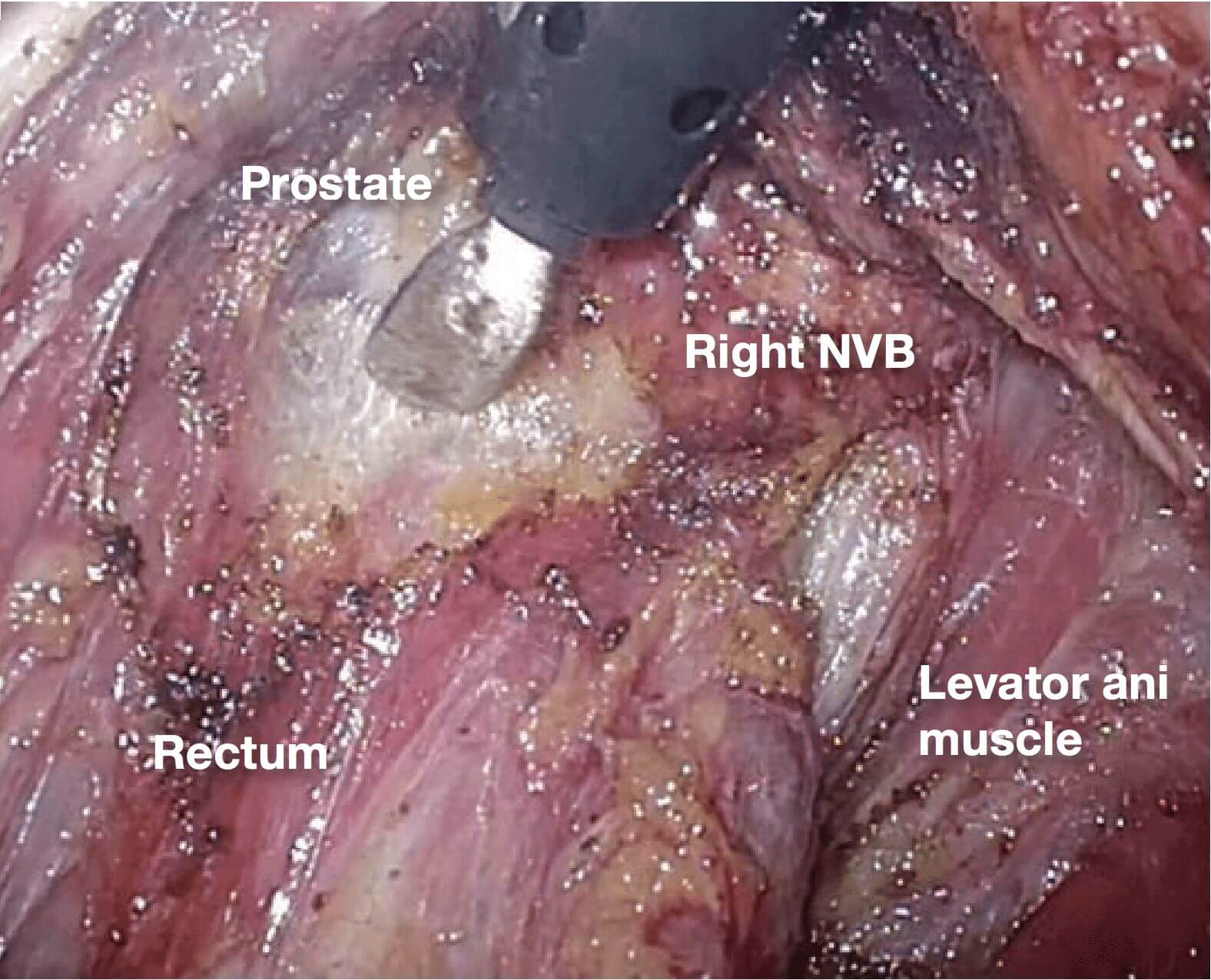
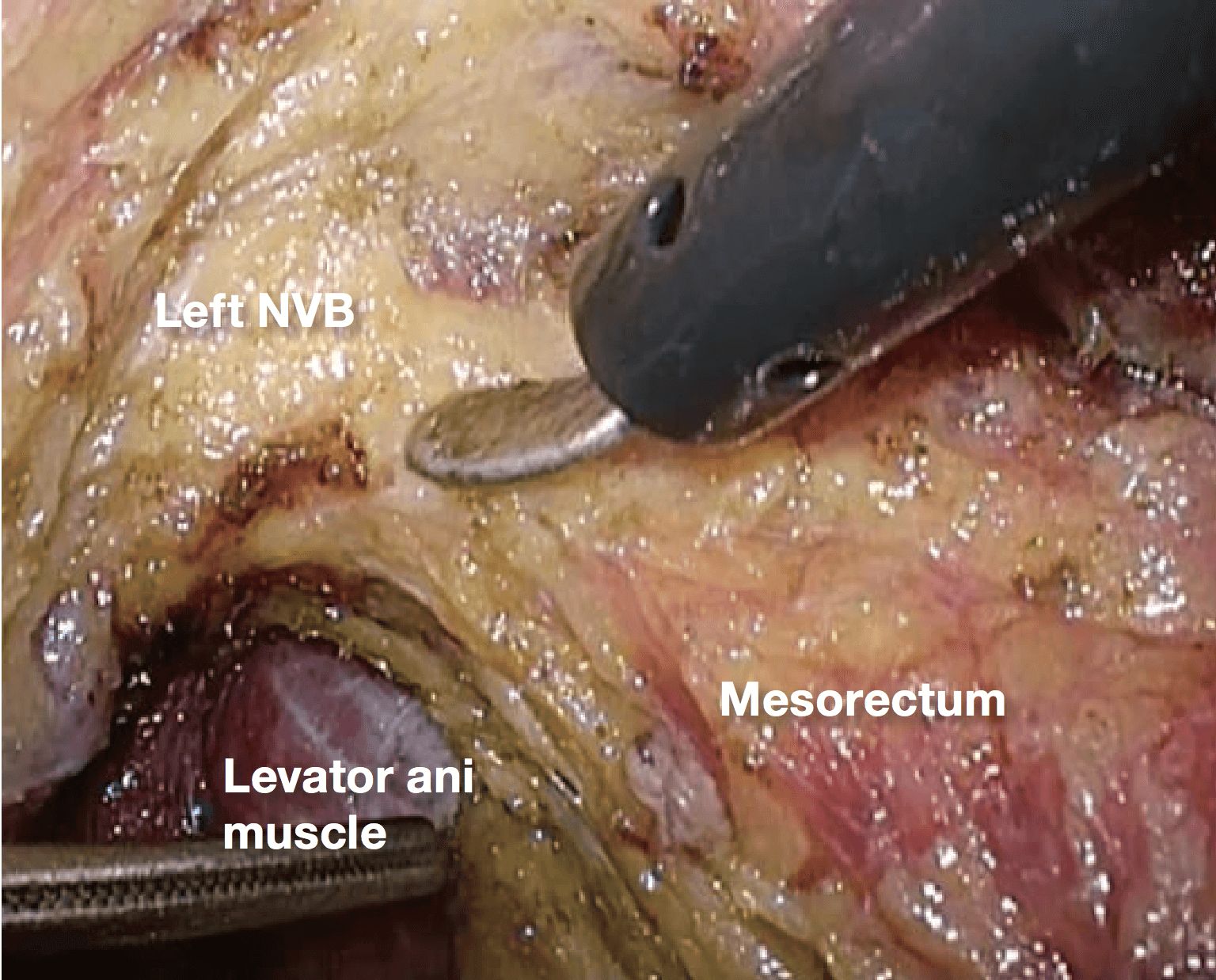
The dissection is advanced into the
supralevator space, and the muscle bundles of the levator ani are exposed. After this dissection, the anatomy between the mesorectum and NVB becomes three dimensional, and dissection is actually simplified because the endpoint of dissection can be recognized.
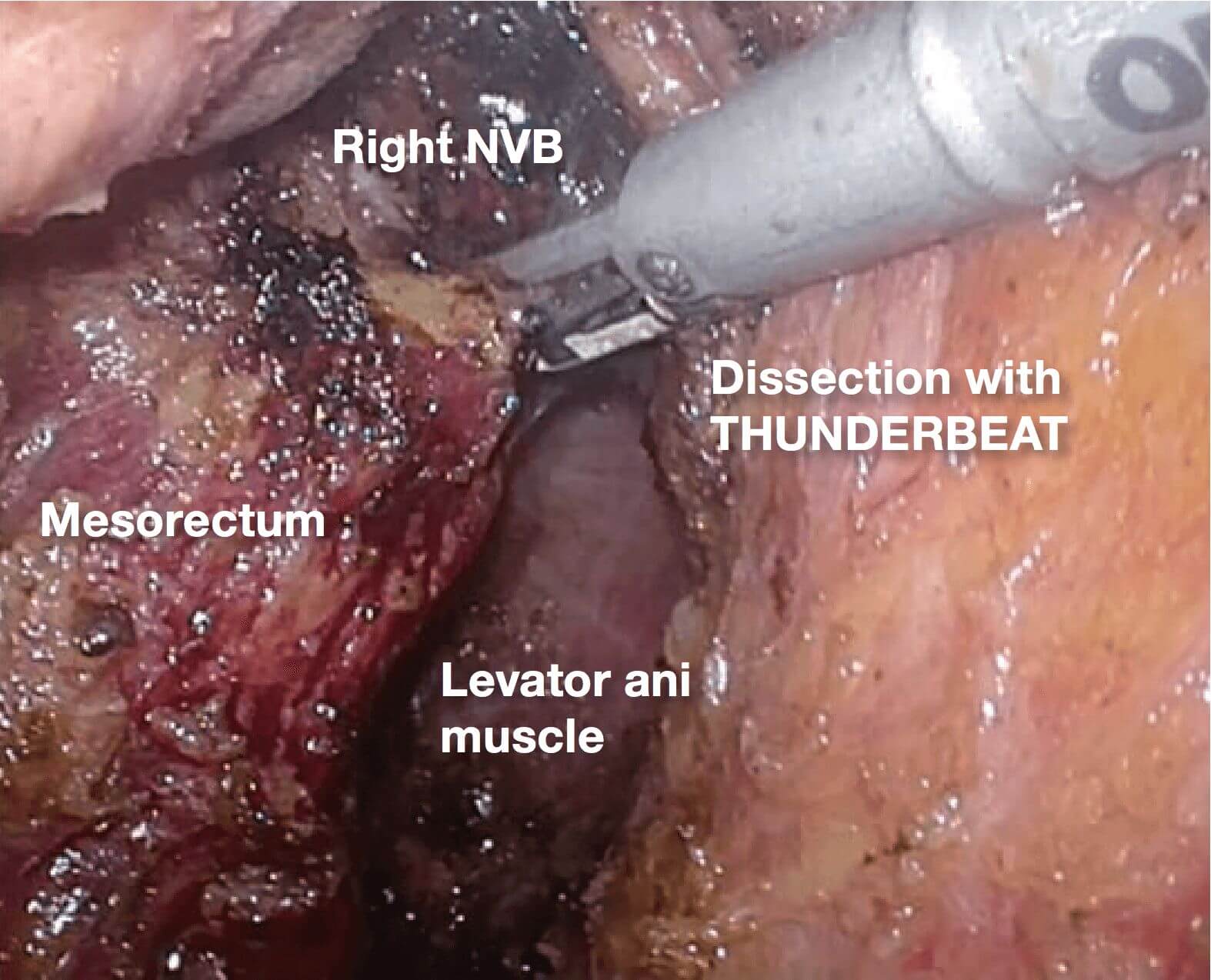
9.The withdrawn NVB is easy to bleed and once bleeding occurs, it is difficult to stop only with electrocautery coagulation. An ultrasonic coagulator is usually used for the hemostasis, but the mist produced often obscures the operating field. The THUNDERBEAT™ device used here produces a small amount of mist, and it is capable of coagulation and incision in a short period of time; therefore, it is exceptionally useful.
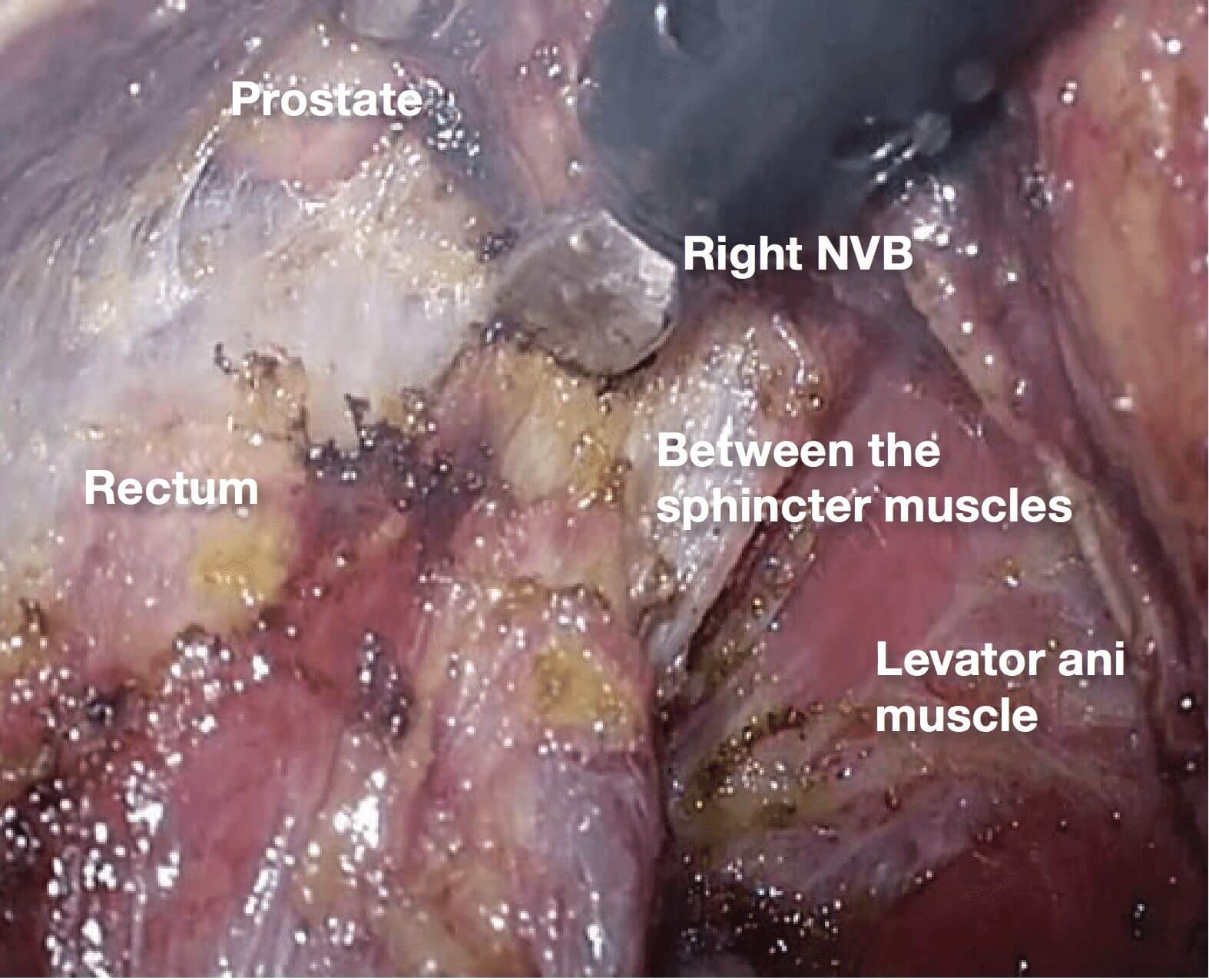
10.(Photographs 10 – 13) 13 The endpoint of dissection here is between the rectum and the levator ani
muscle. The thick vein that runs within the NVB toward the dorsolateral prostate appears. Because hemorrhage occurs readily, the THUNDERBEAT™ device is useful here.
3.Dissection on the left side | (1) Posterior to lateral
How to make an operating field
The operator applies traction to the rectum, and the assistant exposes the pelvic side. When the sigmoid colon is long, it is useful for the assistant to use the left hand for levering, straightening the sigmoid colon, in order to make operating field.
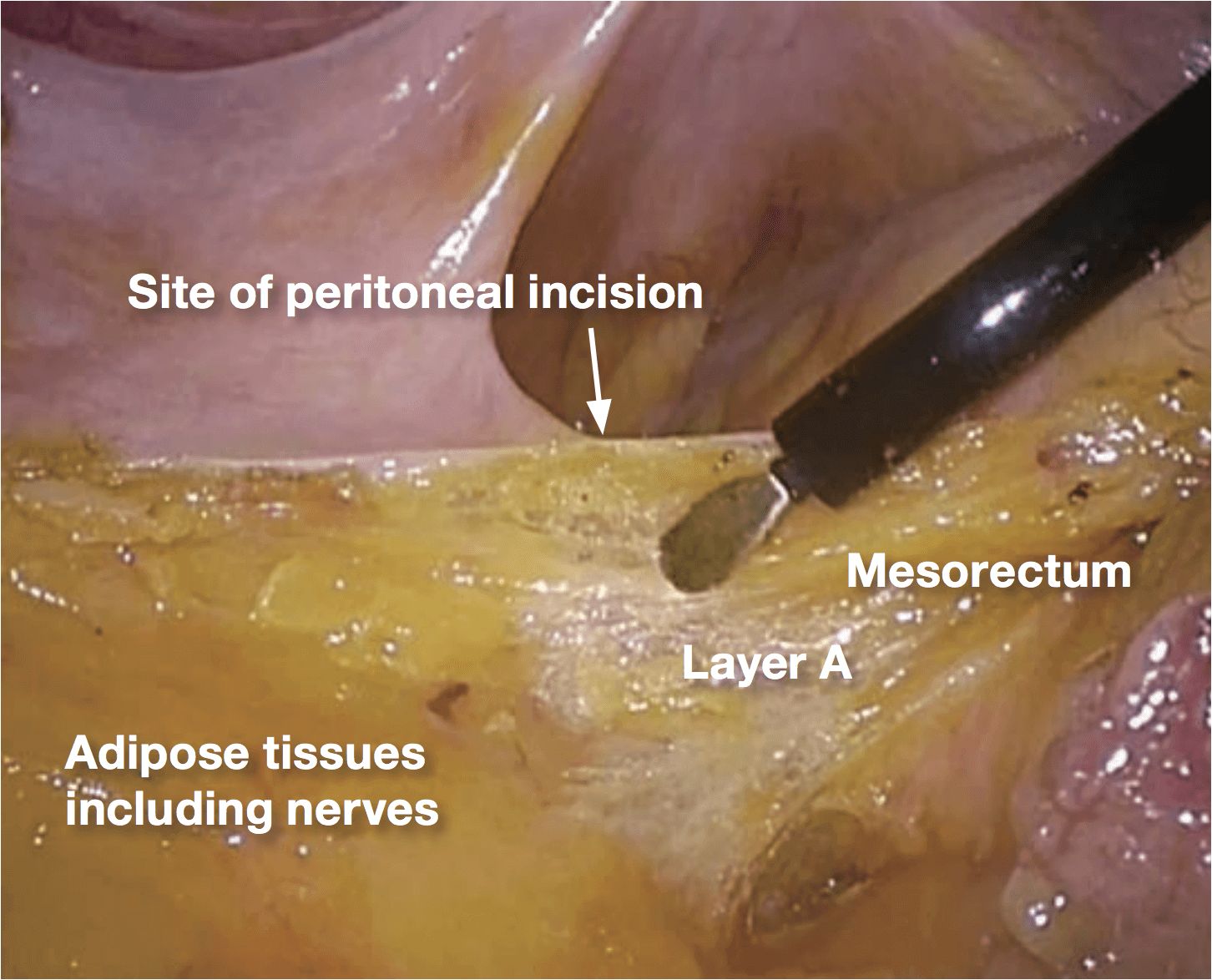
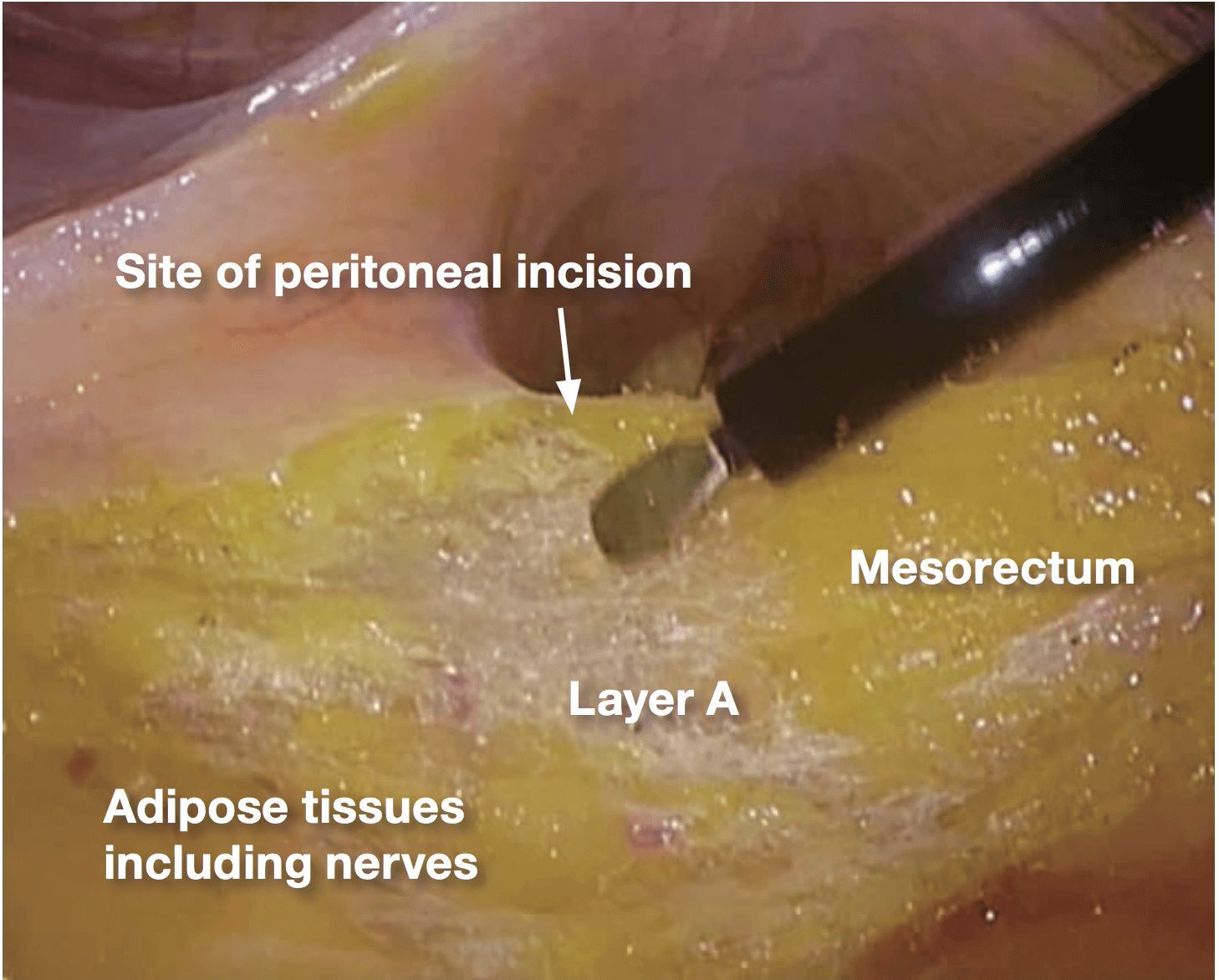
1.(Photographs 1 – 2)
After confirming layer A, the boundary be- tween the mesorectum and the adipose tissue containing the NVB, the peritoneum should be incised just above this boundary. If peritoneal incision is preceded, it may be inaccurate to lead the following dissection to the wrong direction.
3.After dissection is advanced in layer B posteriorly, the A-B boundary tissue, i.e., the lateral ligament, is easily identified.
4.The medial surface of the pelvic nerve plexus is a landmark of the A-B boundary. Posteriorly, the autonomic nerve branch arising from the sacral nerves is also a good landmark.
3.Dissection on the left side | (2) Lateral to anterior
How to make operating field
Exposure is the same as in the posterior direction.
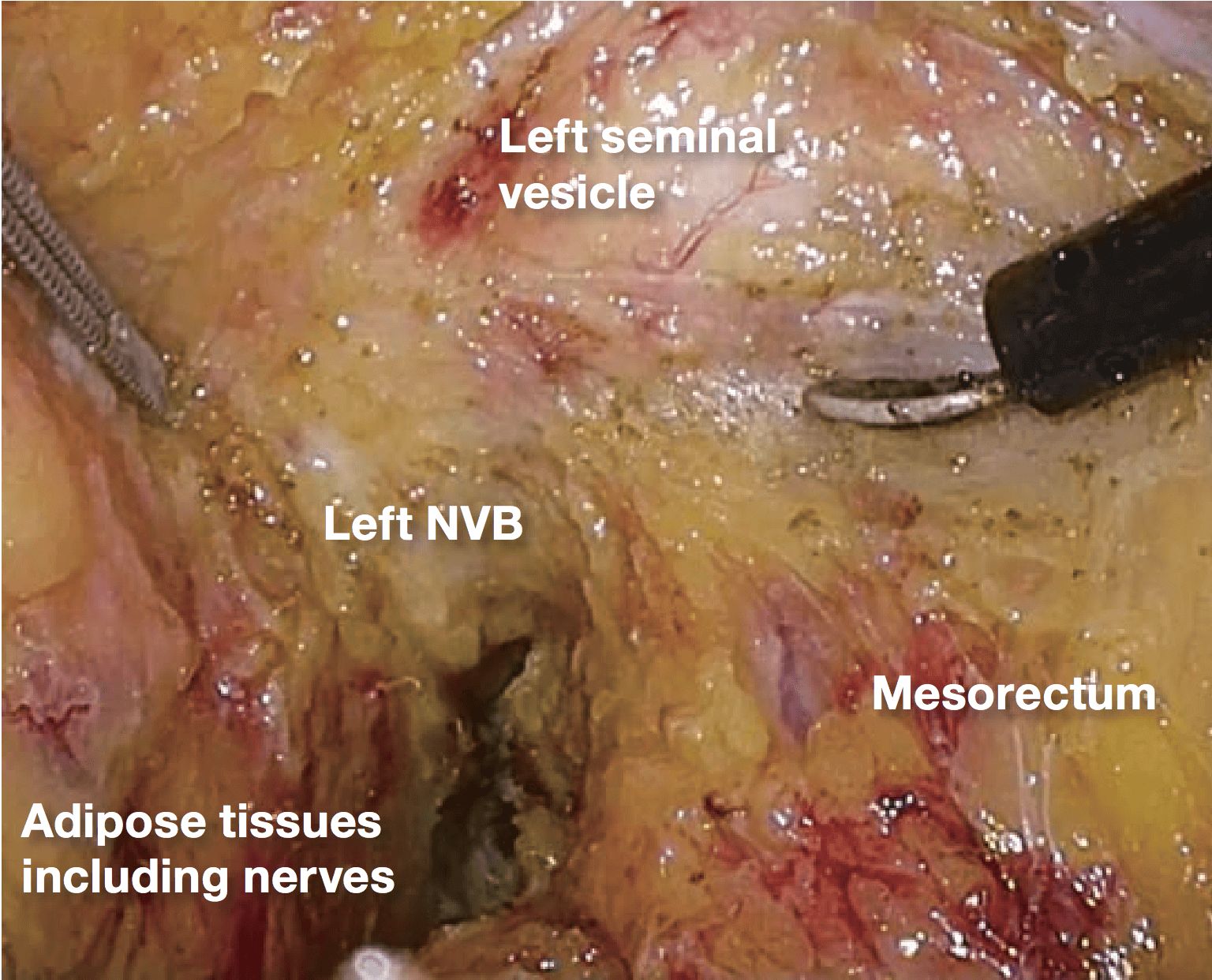
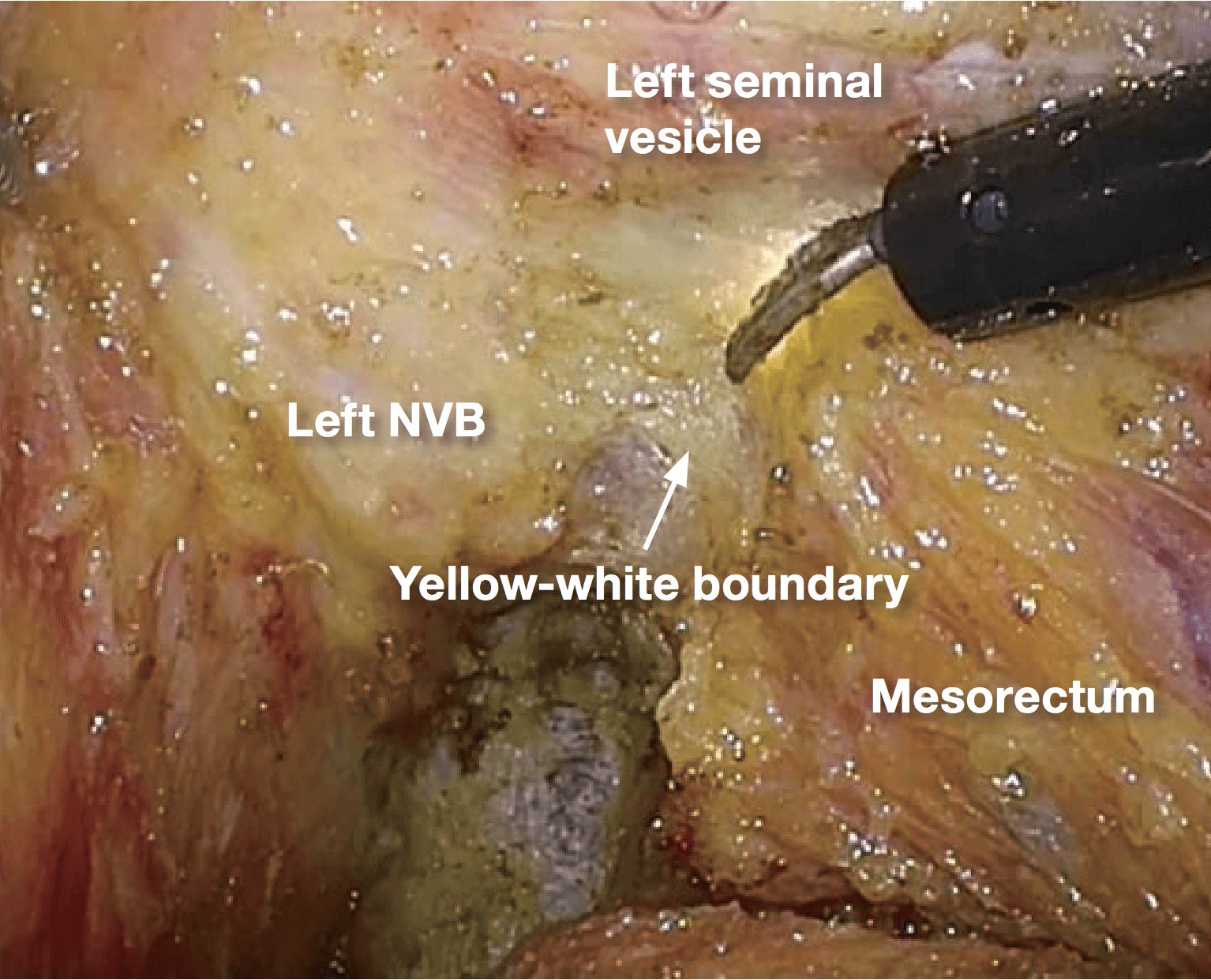
1.As on the right side, the yellow-white 4 boundary usually becomes indistinct in the
anterolateral direction.
2.(Photographs 2 – 5) 5 As on the right side, the seminal vesicle is
confirmed on the left, and the dissection “in” the Denonvilliers’ fascia is advanced, until the yellow-white boundary appears anterolaterally, that can be connected to the posterior dissection already done. With continuing this process in a caudal direction to the pelvic floor, the dissection between the mesorectum and the NVB can be completed.
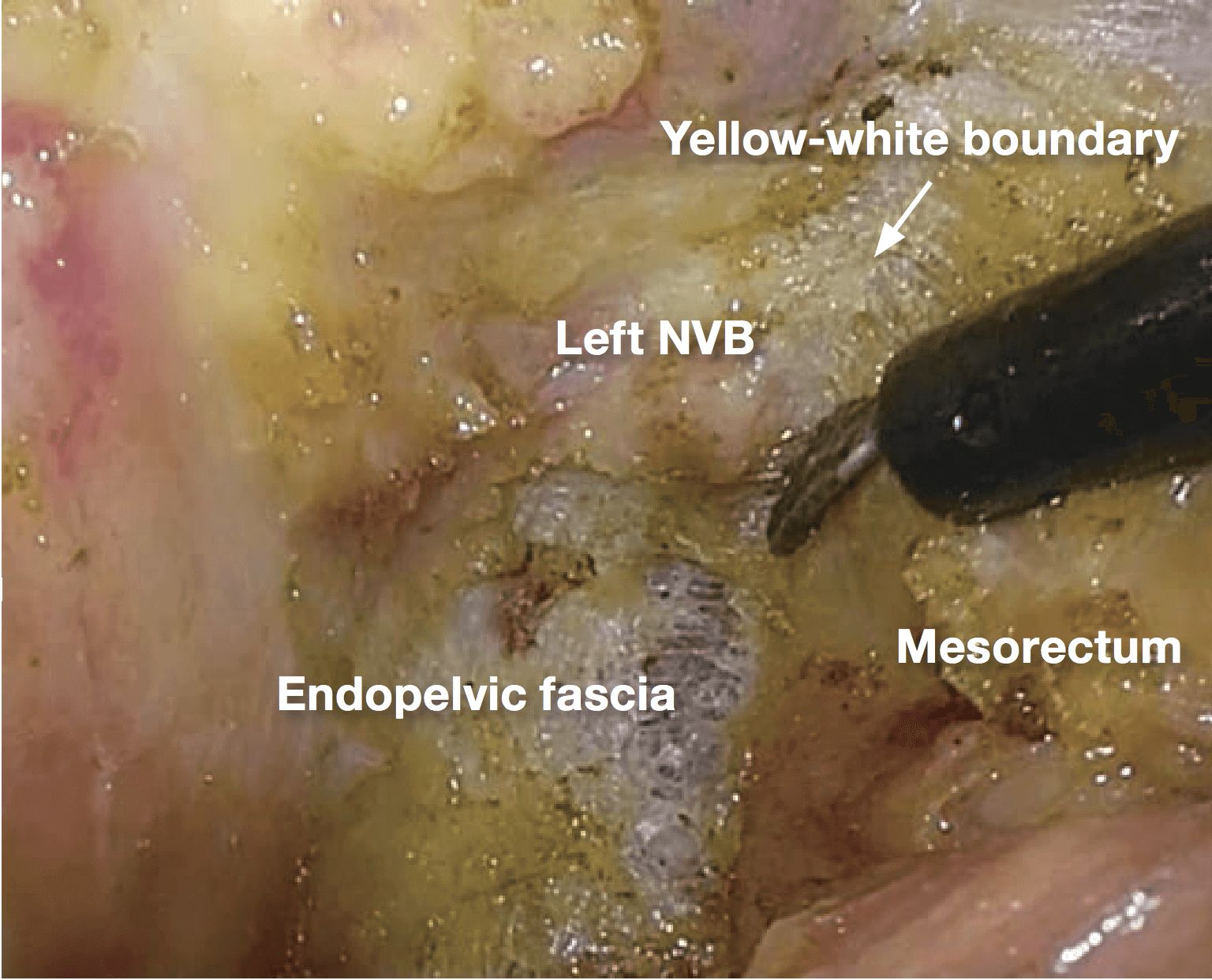
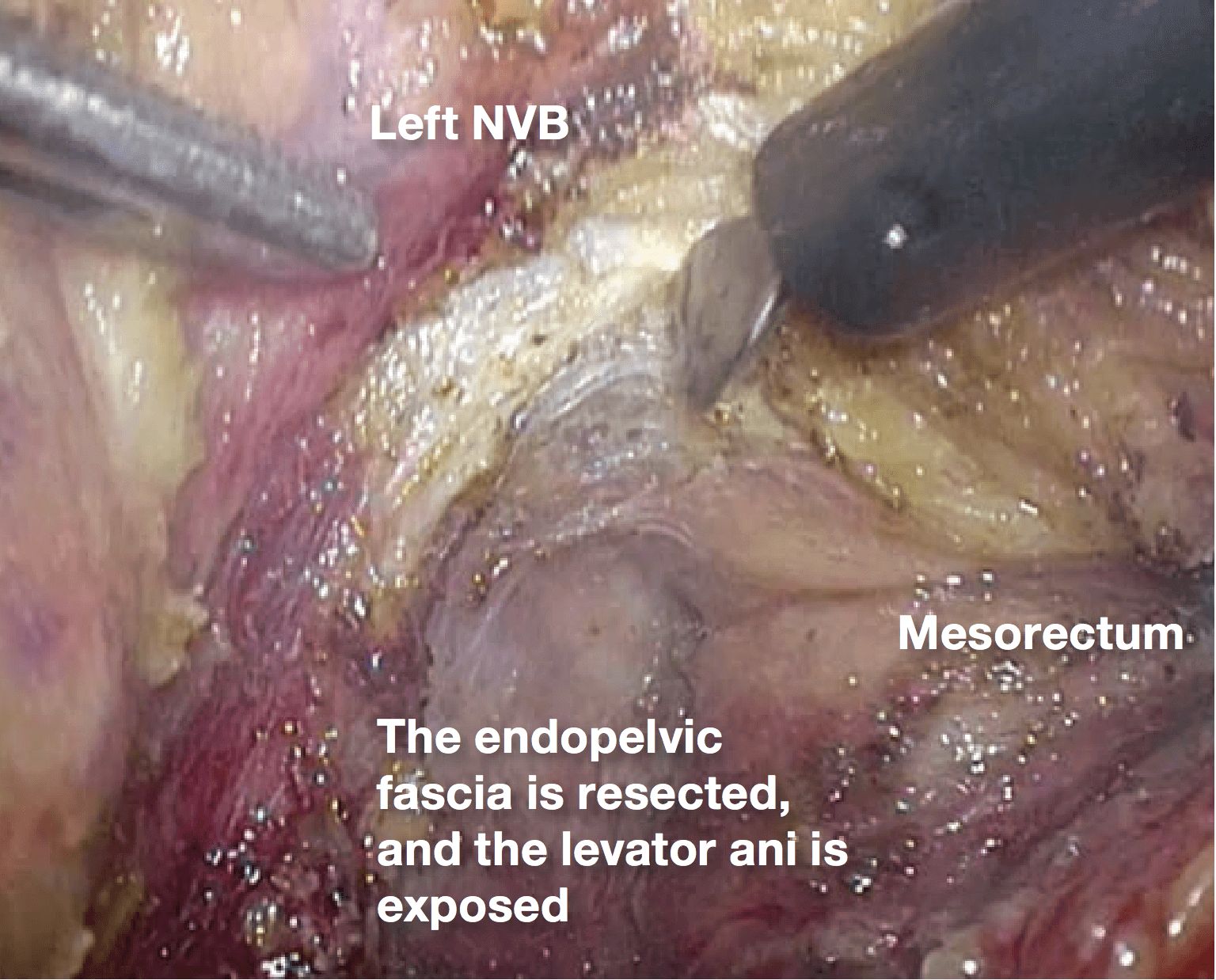
6.(Photographs 6 – 8)
The endopelvic fascia covering the levator ani is incised and resected with mesorectum. This makes it possible to secure a circumferential resection margin and to identify the boundary between the mesorectum and the NVB easily.
9.Thick blood vessels run within the endopelvic fascia, and these are coagulated and dissected with the THUNDERBEAT™ device.
Conclusion
According to my personal experience, the intrapelvic anatomy was not easily understood when laparotomy was performed, but by using a laparoscope, it became possible to gain a clear understanding of the intrapelvic anatomy. It has become even more precise thanks to such advances as high-definition video systems. In the case illustrated, we used a 3D videoscope, which allows for true three-dimensional visualization of the surgical field. Combined with our refined understanding of the anatomy, this technology continues to enhance the surgical experience. The depth perception it provides remains a valuable and engaging advancement for surgeons. It is highly regrettable that the images provided herein are not three-dimensional, but I strongly recommend that surgeons try out a 3D system as there will be many opportunities to come into contact with the 3D scope in various situations, such as academic lectures.
July 2014
Dr. Hiroya Kuroyanagi
Department of Surgery
Toranomon Hospital
- Content Type