Prof. Suh, Kyung-Suk
Department of Surgery
Seoul National University College of Medicine
Seoul National University Hospital
1. Introduction to Liver Transplantation in Korea
More than 1,500 liver transplants are performed in Korea annually and approximately 80% of them are living donor liver transplantations (LDLTs). According to the International Registry in Organ Donation and Transplantation, the number of LDLTs performed in Korea in 2017 was 19.9 per one million people, which was the highest in the world.
Laparoscopic liver resection is quickly becoming widespread in Korea. A recent comparative study using propensity score matching analysis showed similar oncological outcomes for both Laparoscopic and traditional open approaches to liver resection for hepatocellular carcinoma, even for patients with cirrhosis. However, due to concerns about donor safety, laparoscopic donor hepatectomy, especially right hepatectomy, is still classified as one of the most difficult laparoscopic procedures. For this reason, there have been attempts to use laparoscopic-assisted hybrid methods for donor hepatectomy. With the development and introduction of the 3-dimensional (3D) flexible scope (ENDOEYE FLEX 3D DEFLECTABLE VIDEOSCOPE, OLYMPUS LTF-190-10-3D, Olympus Medical Systems Corporation, Tokyo, Japan), it is now possible to have the same surgical field of vision in a laparoscopic procedure as in an open one. Several centers are now performing pure laparoscopic donor hepatectomies.
Currently, approximately 60%–70% of all liver surgeries at Seoul National University Hospital are performed with a pure laparoscopic method.
2. What is LDLT?
LDLT is a viable alternative to deceased donor liver transplantation when there is a donor organ shortage. Once a donor candidate is found for a patient, the patient can receive the liver from that particular donor. In these cases, the organ is not considered a public resource, but it is dedicated only to the matched patient. However, LDLT surgery poses some risks for the donor patients. While it is important to guarantee donor patient safety, it is also important to address their cosmetic and functional outcomes. Pure laparoscopic donor hepatectomy (PLDH) is a new option that considers these issues. PLDH was first performed in Europe in 2001. Since then, it has spread to Eastern countries and the graft can now be both the left or right liver. A PLDH program was first started at Seoul National University Hospital in November 2015. As of June 2019, more than 300 PLDHs have been performed, most of which result from a pure laparoscopic donor right hepatectomy (PLDRH). According to our previous reports, PLDRH had less blood loss and a shorter hospital stay in both the donor and recipient postoperative outcomes.
3. PLDH Surgical Challenges and Solutions
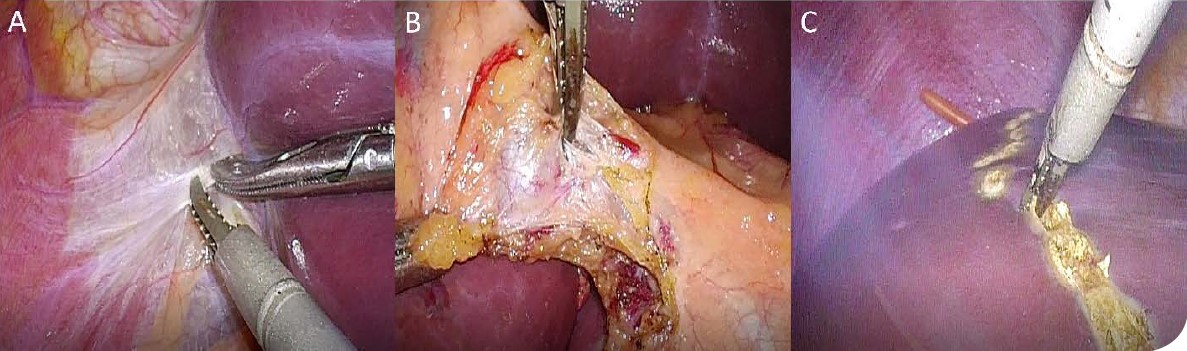
3-1. Dissection and bleeding control Dissection
The application of the THUNDERBEAT (THUNDERBEAT Front-Actuated Grip Type S; Olympus Medical Systems Corporation, Tokyo, Japan), an integrated bipolar and ultrasonic energy device is useful because it naturally dissects the exact, appropriate surgical plane.
The THUNDERBEAT has an advantage over the conventional electrosurgical unit during dissection as it can be used similarly as having two jaws. Moreover, the jaws of the THUNDERBEAT are more accurately controlled by hand movements than any other energy device, so it can assist with fine tissue dissection. It also has strong coagulation power, which makes it easy to control minor bleeding generated during dissection.
When dissecting around major structures like the hepatic hilum, surgeons can dissect only the desired structure without transferring heat when facing the upper jaw.
It can also be used as a liver parenchymal transection device in the place of an ultrasonic aspirator. Since the principle of ultrasound is the same, surgeons can use the active blade of the THUNDERBEAT in the similar manner as the tip of the ultrasonic aspirator. It can also perform the similar function as the Kelly crushing method that is used in an open hepatectomy by generating energy when clamping small sections of tissue. The surface can be cut cleanly with less bleeding by applying energy to transect the liver parenchyma. In my case, the THUNDERBEAT is being used to seal any small bile duct openings exposed at the cut surface, reducing the possibility of bile leakage. However, unlike ultrasonic aspirators, it has no suctioning function. Thus, it is helpful to use the THUNDERBEAT with a suction device.
Bleeding control
Bleeding control is important in all surgeries. However, it may be not easy to control bleeding in laparoscopic surgeries and inexperienced surgeons may be concerned about bleeding in a major hepatectomy.
PLDRH requires dissection around the hilum and inferior vena cava (IVC), both of which have a potential risk of causing major bleeding. Small venous bleeding can also be problematic because it can be masked by pneumoperitoneum. Careful dissection while controlling bleeding from all vessels is important. THUNDERBEAT has a sharp tip and, with the help of the 3D flexible scope, enables precise dissection in a small space.
Gentle opening and closing of THUNDERBEAT jaws may serve as a dissector. Large vessels can be ligated with intracorporeal ties or clips but small vessels can be ligated with THUNDERBEAT and save time in surgery. It may also be useful with liver mobilization, hilum dissection, and small short hepatic vein division.
It is always important not to injure surrounding tissues with thermal energy. The working jaw should face away from important tissues such as the bile duct during hilum dissection and the IVC during short hepatic vein division. The liver capsule and superficial parenchyma can be sufficiently transected with THUNDERBEAT while minimizing blood loss.
Combined with THUNDERBEAT, the 3D flexible scope is also very helpful for bleeding control. Three-dimensional vision provides better depth perception for surgeons to focus on bleeding areas. Surgeons should be able and ready to use intracorporeal sutures whenever necessary due to unexpected events and depth perception is especially essential for this. The 3D flexible scope provides surgeons with a good view while working in small spaces. The 3D flexible scope can provide a bird’s eye view, low angle view, and lateral view. Bird’s eye and lateral views are especially useful in mobilizing the right liver. With these views, the surgeon is able to see all structures clearly and avoid accidentally injuring any surrounding tissues or vessels. The low angle view is often used for inferior liver mobilization and dissecting the liver from the IVC. Safe dissection of both short and inferior hepatic veins in a small space without injuring any structures around them is possible using the low angle view.
Demarcating and transecting the exact midplane of the liver can minimize blood loss. There is no need to ligate or clip the inflow structures in the small intrahepatic Glisson branches if transecting the exact midplane of the liver. It may also reduce surgery time.
3-2. Difficulty of anatomic identification
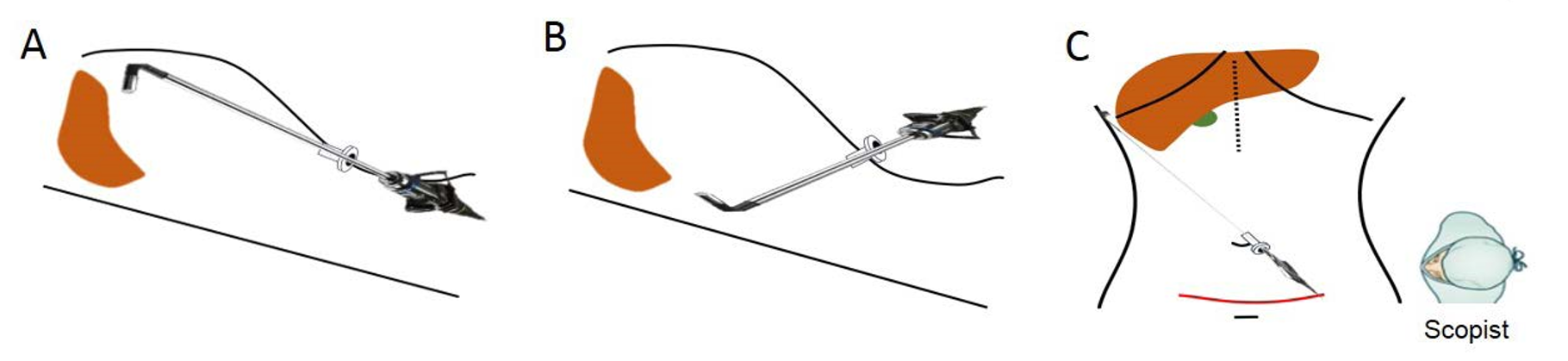
One of the reasons laparoscopic hepatectomy is difficult is because the surgical field is wide and the organ is large, so there are many hidden areas. By using the 3D flexible scope, it is possible to get a similar surgical view as in an open method or, occasionally, an even better view. Right liver mobilization is required for the right hepatectomy. It is difficult to see the posterior surface of the liver with a 2-dimensional 30° rigid scope, making mobilization difficult. The posterior surface of the liver can easily be checked using the 3D flexible scope, making mobilization easier. Because of this, a surgeon who is familiar with the open method can easily change to the laparoscopic method. The 3D flexible scope provides surgeons a better anatomical understanding by having the advantage of depth perception and an angulated view. The 3D flexible scope can guarantee easier movement in a small space.
The 3D flexible scope provides three types of laparoscopic view: bird’s eye view, low angle view, and lateral view. The bird’s eye view is used during the mobilization of the upper portion of the IVC, coronary and triangular ligaments, hilar dissection, and parenchyma transection. The bird’s eye view is the standard view used throughout the entire procedure. The low angle view is used during mobilization of the inferior part of the liver, dissection of the liver from the IVC, and transection of the caudate lobe. Alternating the bird’s eye view and the low angle view is necessary during dissection and division of the right hepatic artery and the right portal vein to ensure that important surrounding structures are not damaged. The lateral view is helpful during the mobilization of the lateral portion of the liver. The lateral view can also be combined with other views during liver parenchymal transection to minimize interference between the scope and other instruments.
4. Procedural Steps for Pure Laparoscopic Donor Right Hepatectomy
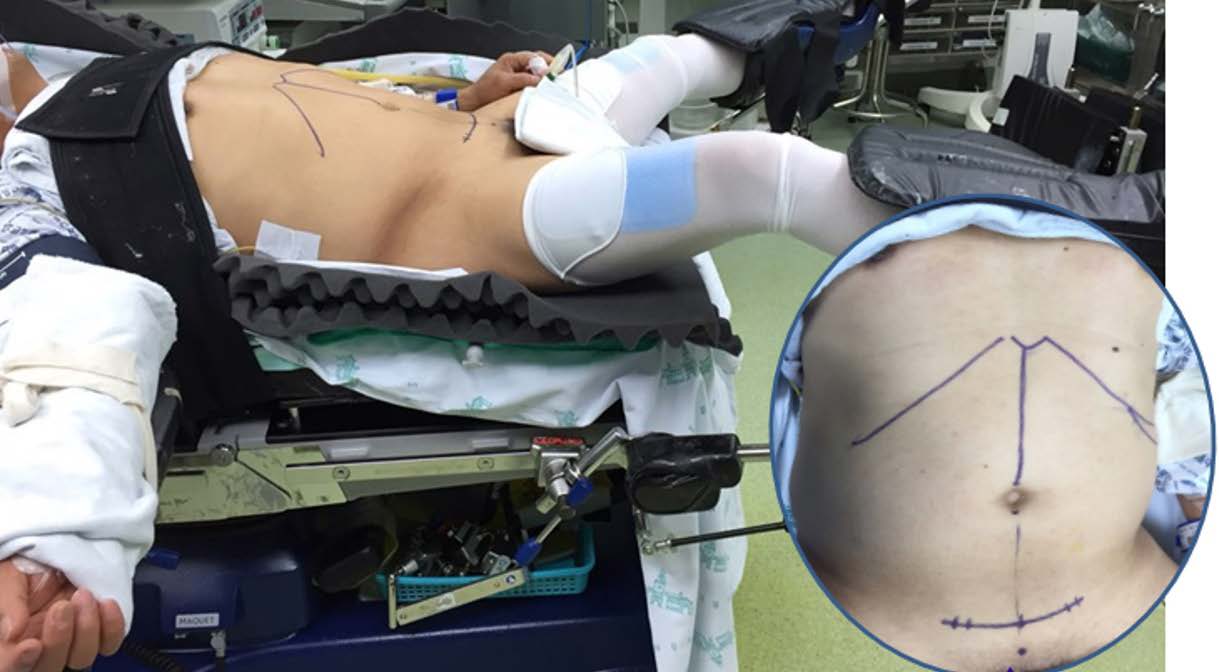
4-1. Patient and port position
The donor is placed in the reverse Trendelenburg position with the left side at a downward tilt with the legs apart. To enable an adequate bird’s eye view, the knees should not be bent too much. Three monitors are placed in front of the surgeon: one laparoscopic main monitor, one monitor showing simultaneous vital signs, one monitor showing preoperative computed tomography or magnetic resonance cholangiopancreatography (according to the step of the procedure). A second laparoscopic view monitor is placed on the right side of the donor. A liver doppler is also prepared in case it is needed. Five ports are used with the umbilical port being the camera port. The main working port is placed just below the right subcostal margin and above the gallbladder fossa, targeting the midplane of the liver and the liver hilum.
4-2. Mobilization of the liver (with THUNDERBEAT)
First, the falciform ligament is divided in the direction of the upper part of the IVC using THUNDERBEAT and then the right coronary and triangular ligaments are divided. Next, using the low angle view, the inferior liver is mobilized. Bleeding during dissection from the right adrenal gland can be minimized by following the correct dissection plane and using THUNDERBEAT. The right side of the caudate lobe is mobilized from the IVC by dividing small branches using THUNDERBEAT, clips, or intracorporeal ties. The large right inferior vein can be transected later using a stapler or Hem-O-Lok clips.
Dissection of the liver and IVC is performed as high as possible using THUNDERBEAT or clips to make a safe space to insert the nelaton tube. The 3D flexible scope and THUNDERBEAT are especially useful in this step because the procedure only needs a small space. A nelaton tube is carefully inserted into the space between the liver and IVC and the distal end is pulled out between the right and middle hepatic vein. This nelaton tube is used later for the hanging maneuver.
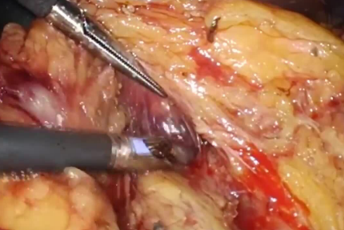
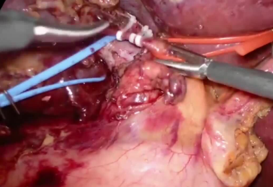
4-3. Vessel and Glisson handling
After dividing the cystic duct and cystic artery, the gallbladder is partially divided from the liver for further retraction during the later procedure. By pulling the gallbladder and cystic duct apart, the right side of the hilum is well exposed and dissected. The right hepatic artery and portal vein are identified by gentle dissection using a dissector or THUNDERBEAT. Surgeons should always use caution not to injure surrounding tissues with thermal energy since the surrounding structures are the hepatic artery, portal vein, and bile duct. Vessel loops are placed around the right hepatic artery and the right portal vein. After completing the cholecystectomy, the right hepatic artery and the right portal vein are temporarily clamped with laparoscopic bulldog clamps.
Surgeons can identify the demarcation line by checking the color change at the surface. The demarcation line is marked with an electronic coagulator.
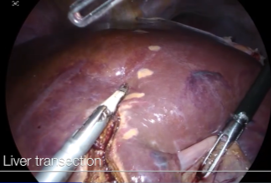
4-4. Parenchyma transection
Stay sutures are placed for traction on both sides of the demarcation line. The liver capsule and the superficial layer of the liver parenchyma are transected using THUNDERBEAT. Deeper parenchyma is transected using a laparoscopic ultrasonic aspirator. When following the exact midplane of the liver, blood loss is minimal and there is no need for division of the vascular structure using clips. The Pringle maneuver is not routinely used. The venous branches of the anterior section are ligated with clips, cut or ligated with Hem-O-Lok clips, and cut for possible reconstruction on the back table.
After double clipping the remnant bile duct side, the bile duct is cut and divided. Then, the caudate lobe is transected using the low angle view and the nelaton tube is repositioned to the front of the right Glisson pedicle. By lifting both ends of this nelaton tube, the deeper portion of the remnant liver parenchyma can easily be transected. After completing the parenchyma transection, the liver is attached only to the vascular structures.
4-5. Graft removal
A suprapubic incision is made without opening the peritoneum. An endo-bag is inserted to lift the liver up. The remnant hepatic artery is ligated with Hem-OLok and metal clips and cut. The portal vein is divided using a bilateral stapler. It is important to double check the area using an alternative bird’s eye view and lowangle view for any problems at the hepatic artery and bile duct. To prevent torsion of the remnant portal vein, stapling is performed vertically. The right hepatic vein is divided using a unilateral stapler. The endo-bag is retrieved though the suprapubic incision after opening the peritoneum.
5. Summary
THUNDERBEAT is routinely used in pure laparoscopic donor hepatectomy and it is an essential instrument in our center. The small and relatively sharp jaws are useful for dissecting as well as controlling bleeding when necessary. Using this instrument with the 3D flexible scope is helpful when working in a small space.
Better depth perception and a variety of views essential in PLDRH, including a bird’s eye view, low-angle view, and a lateral view, can be provided with the 3D flexible scope.
- Content Type