Eun Ji Nam, MD, PhD
Professor, Chief of Women’s Cancer Center, Severance Hospital
Division of Gynecologic Oncology, Chairman of Department of Obstetrics and Gynecology, Yonsei University College of Medicine, Seoul, Korea.
Biography:
Dr. Eun Ji Nam graduated from Yonsei University College of Medicine in 2001, where she also earned her PhD degree in 2011. She completed her surgical residency training of Obstetrics and Gynecology in Severance Hospital in 2006. She finished visiting scholar at Moores Cancer Center, UC San Diego, USA in 2019. She is currently a member of the International Gynecologic Cancer Society (IGCS), American Association for Cancer Research (AACR), Korean Society of Gynecologic Oncology, Korean Society of Obstetrics and Gynecology, and Korean Society of Gynecologic Endoscopy and Minimally Invasive Surgery. In 2013, she won the top cited article during 2011-2012 in Journal of Gynecologic Oncology for the subject of “Robotic single-port transumbilical total hysterectomy: a pilot study”.
1. Introduction
Hysterectomy is the second most commonly performed surgery in women worldwide, next only to cesarean section.1 Laparoscopic hysterectomy has been associated with reduced postoperative pain, shorter recovery time, reduced adhesion formation, and improved short-term quality of life compared with traditional abdominal hysterectomy.2 Conventional electrosurgery comprises unipolar and bipolar diathermy methods.2 There have been constant attempts to devise newer, more efficient energy sources and techniques, with a desire to come up with the most perfect device which can incorporate multiple functions into one, to reduce surgical time and instrument traffic without compromising on the quality of surgery and overall patient well-being.1 Conventional monopolar electrosurgery remains a popular modality in laparoscopy because of its low cost, easy availability, and diverse range of available tissue effects. However, it has its own limitations, involving the need for a dispersive electrode, the relatively high power settings, the possibility of stray current injuries, and the inability to seal vessels larger than 1–2 mm diameter.3 Conventional bipolar electrosurgery needs increased time for coagulation due to a low power setting, which leads to charring and tissue adherence with incidental tearing of adjacent blood vessels.3 The great disadvantage of the conventional bipolar system is that the electrodes cannot cut tissue.3 Also, bipolar instruments can possibly cause lateral thermal damage, and the jaws can potentially stick to the tissue, which is then difficult to remove after coagulation.2 The Advanced bipolar system provides more consistent and reliable hemostasis with significantly less lateral thermal damage associated with conventional bipolar systems.3
2. Key Procedure Steps
TLH using POWERSEAL is presented here. In this case, we performed surgery to resect only the uterus with preservation of the ovaries.
Preparation
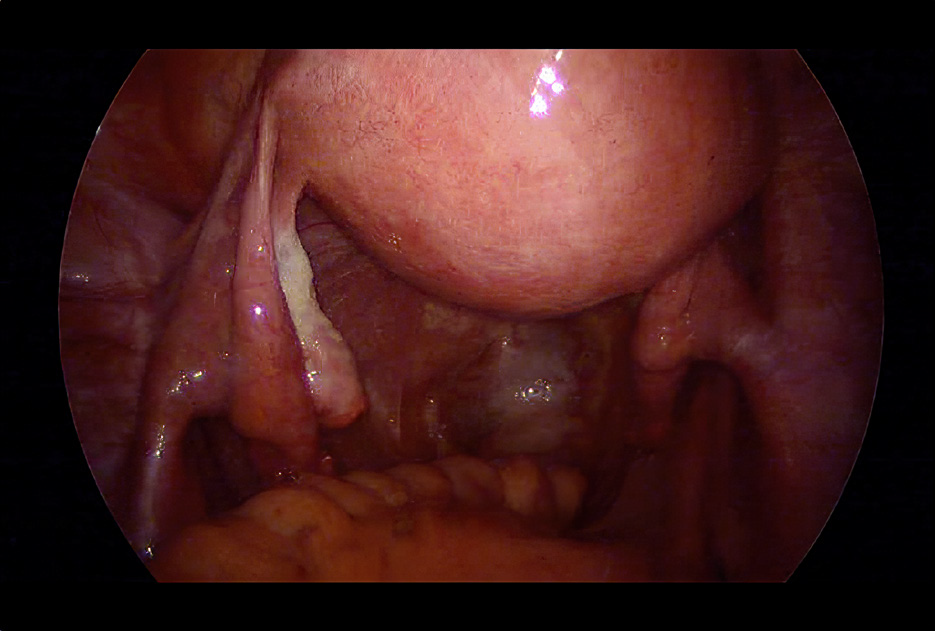
As a preparation step, a uterine manipulator combined with a preoperative KOH ring was fixed to the uterus. When choosing a KOH ring size, it is important to select the correct size as small rings may not differentiate between vaginal fornices and large rings may increase the risk of ureteral injury. TLH used the pneumoperitoneum, in which the skin at the navel is incised and CO2 gas was injected into the abdominal cavity to inflate the belly. To reduce organ damage, a laparoscope was inserted into the abdominal cavity to view the organs and drill three small holes in the lower abdomen and insert a 5 mm trocar. (Fig 2).
Treatment of the adnexa
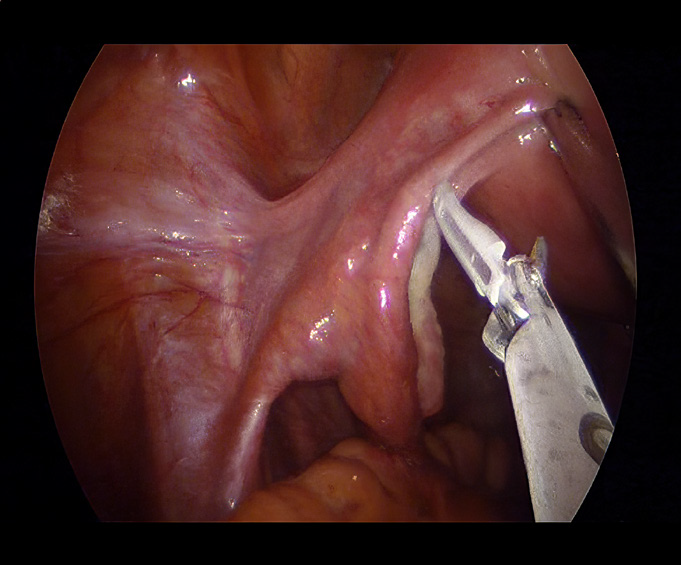
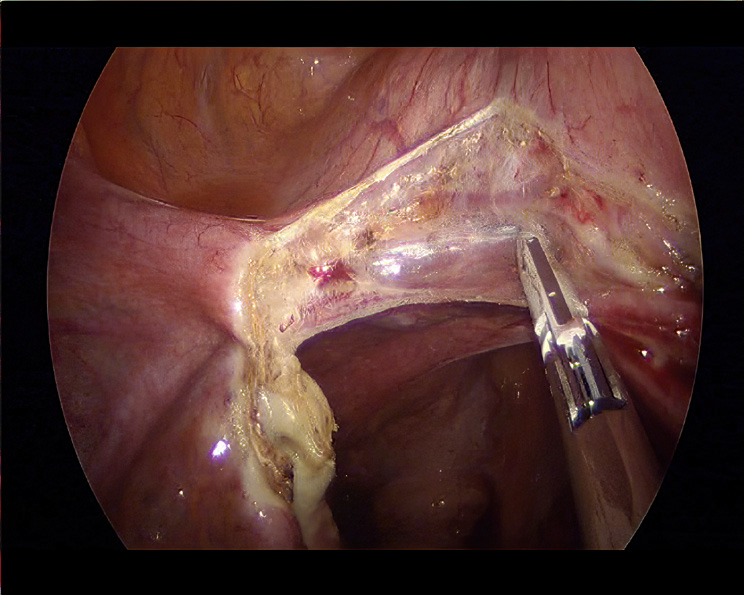
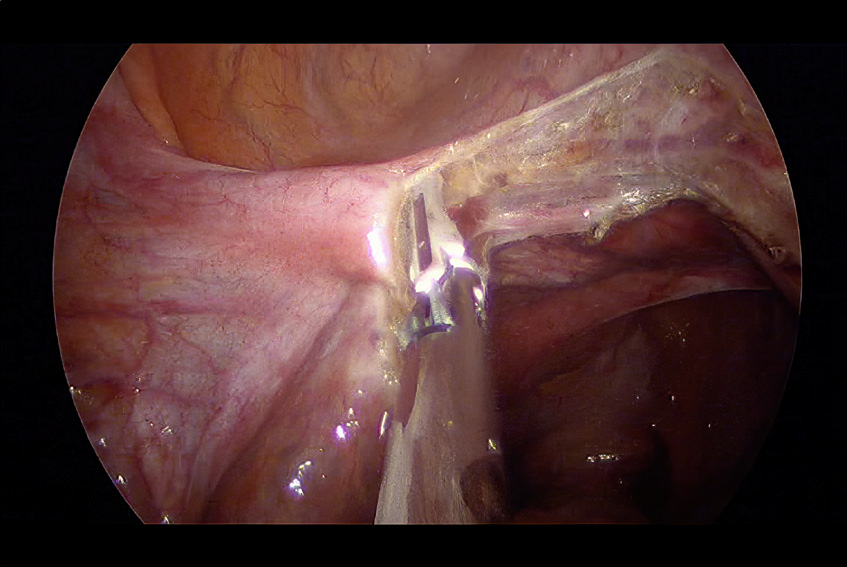
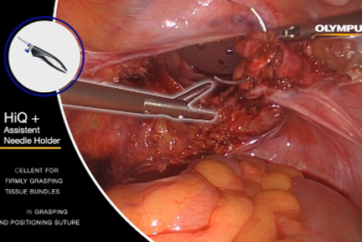
Hysterectomy basically requires coagulation of four blood vessels (two uterine arteries, two utero-ovarian vessels) and coagulation & dissection of three adnexa (round ligament, fallopian tube, ovarian ligament). The operation started from the left cornual region. The fallopian tube and ovarian ligament were coagulated and dissected using POWERSEAL (Fig 3A,B). We used POWERSEAL to coagulate and dissect the fallopian tube and ovarian ligament (Figure 3A,B). The waveform for POWERSEAL generated from eletrosurgical generator continually responds and adjusts to changing tissue conditions resulting in reliable sealing throughout the surcial procedure.5 After sealing, the tissue was cut by pulling the cut trigger to send the blade out.
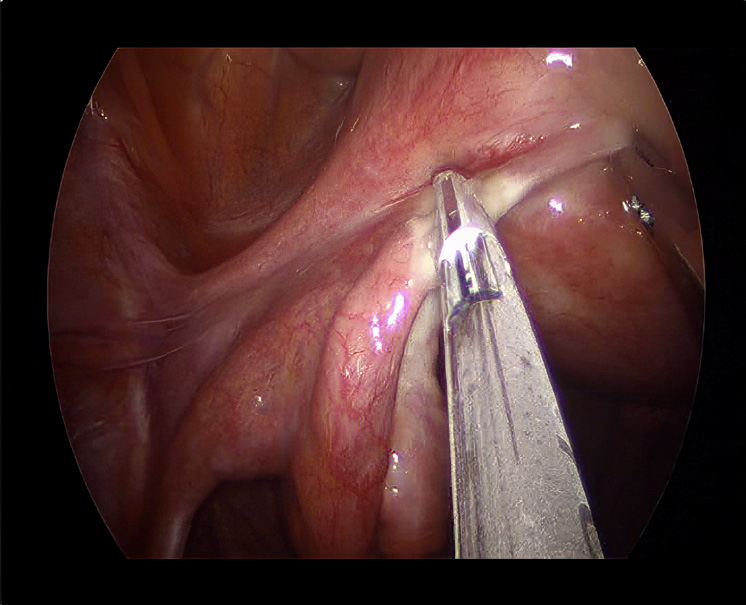
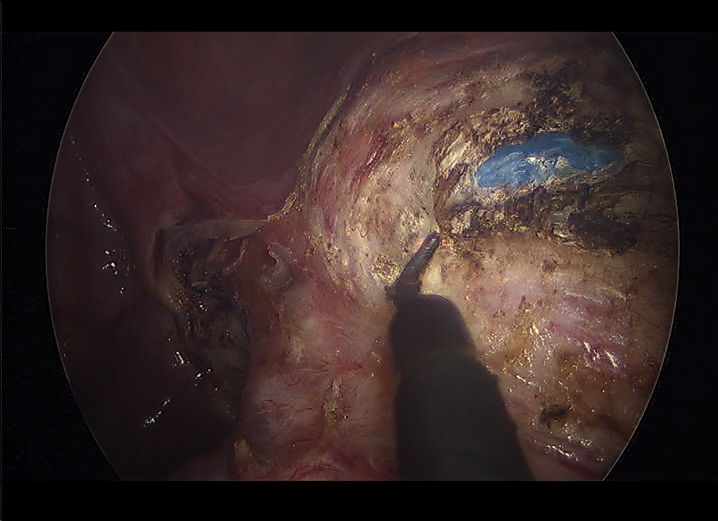
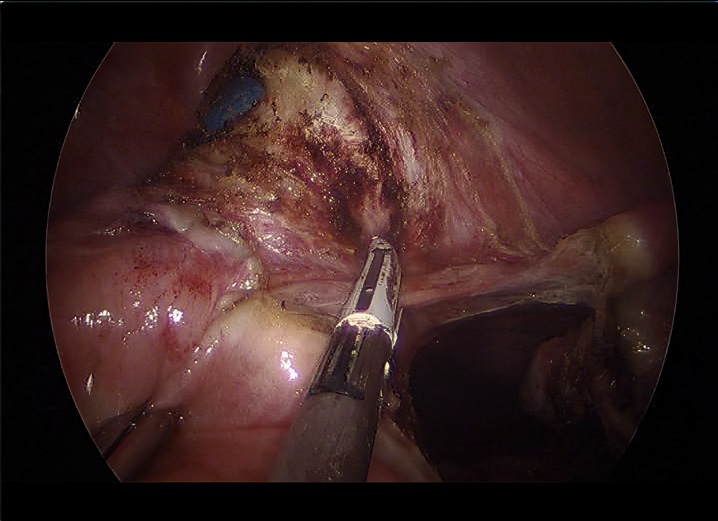
Coagulation and dissection of the round ligament (1 cm from the uterine insertion) is recommended to be performed at the avascular triangle of the broad ligament, which is surrounded by the iliac vessels and the adnexa vessels (Fig 3A). This is to avoid retrograde bleeding of the uterine vessels that retract into the uterus during dissection. If bleeding does occur, it’s important to get it under control quickly. With POWERSEAL, it is simple to spot coagulate localized bleeding on the surface of the tissue. After adnexa dissections, broad ligament was coagulated and dissected, paying attention to ureteral injury. Proceeded with the coagulation and dissection of the right adnexa in the same processing (Fig 3C). A small bleeding occurred during the peeling from the fallopian tube, but we were able to coagulate it using POWERSEAL (Fig 4).
Uterine vessels ligation
The anterior vaginal wall was cut first to reduce bladder and ureteral injury in patients with benign conditions.
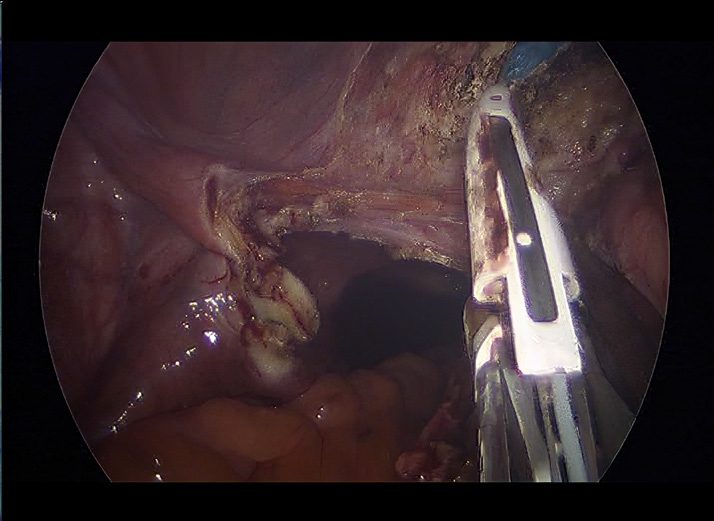
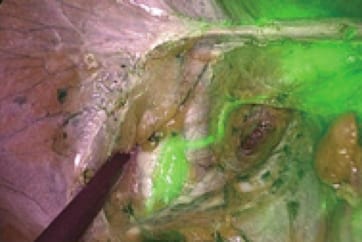
After identifying the location of the uterine ligament and cervix, the peritoneum and bladder were detached from the uterus. To avoid contaminating the detached layer with blood, the connective tissue was dissected without bleeding and the bladder was separated until the uterine arteries were visible (Fig 5A).
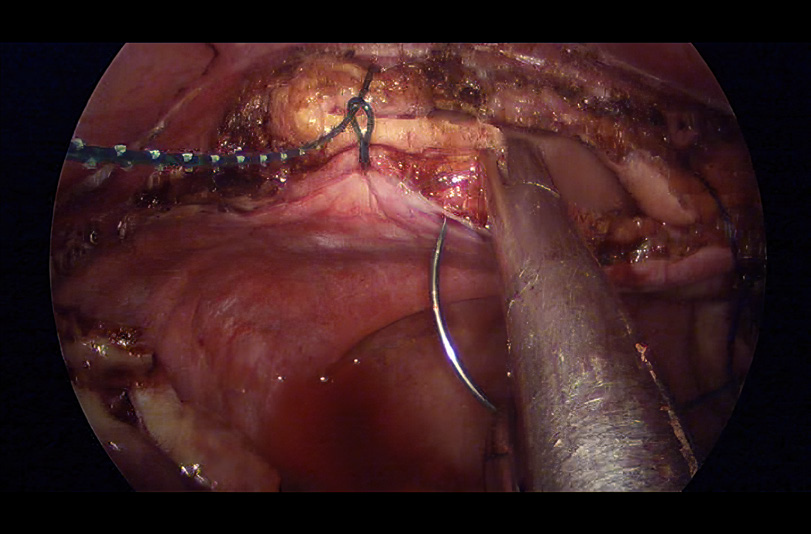
If mobilization was performed after bladder dissection, vaginal artery and vein was isolated and ligated. The connective tissue and peritoneum around the left uterine vein were then incised to isolate and coagulate the vein (Fig 5A). The POWERSEAL’s longer jaws made it easier to grasp and cut the vaginal arteries and veins. The POWERSEAL has both latch on and off feature, which can provide the selection to surgeons. Latch on helps reduce hand fatigue by eliminating the need to constantly pull the jaw lever while sealing. Latch off is a non-locking feature that can be used efficiently when dissecting tissue by utilizing the force of the jaws opening to either side. By having this feature, POWERSEAL is able to use as a dissector and this can reduce the number of changing instrument. Therefore, the POWERSEAL advantage shown in vaginal artery and vein can enhance the efficiency of the surgical procedure. Similarly, proceeded with isolated ligation of the right uterine artery, and coagulation of the right basal ligament vessels (Fig 5B,C).
Removal of the Uterus & Vaginal Closure
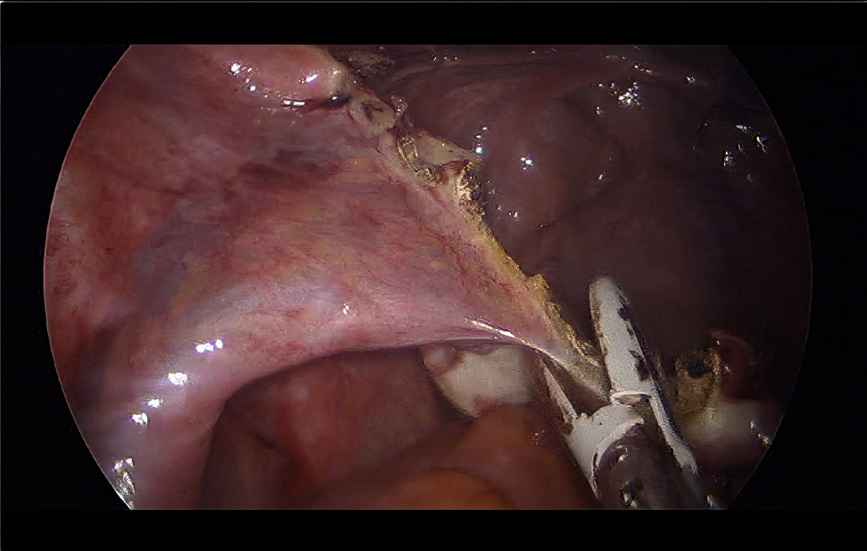
Continued with the posterior vaginal wall incision, observing from the right side. After sufficient dissection of the anterior and posterior vaginal walls, the left basal ligament was finally coagulated and cut.
The detached uterus was wrapped in an in bag morcellation and taken out through the vagina. The surgical site was irrigated and carefully examined to rule out possible bleeding. The vascular pedicles, vaginal vault, ureters, and bladder were checked for damage to surrounding structures. Performed a vaginal closure to restore pneumoperitoneum. The vaginal closure included a sufficient width of vaginal mucosa and fascia (Fig 6A). Finally, the residual fallopian tube was removed (Fig 6B). Waveform of electrosurgical generator and TiN coated jaw combine to yield equivalent tissue sticking resistance compared to existing products. This allows the jaw to remain relatively clean throughout the long operation, reducing jaw cleaning time.
3. Benefits of using POWERSEAL
- POWERSEAL delivers the optimal amount of energy at the right time resulting in reliable sealing throughout the surgical procedure.5
- The ergonomic design of the POWERSEAL allowed for a grip and less hand fatigue, making it more efficient for surgery.6
- The long length of the jaws was beneficial in ovary removal and adnexectomy, allowing for effective coagulation and ligation.
- Double-action jaws are designed to facilitate grasping of thick tissue and efficiently dissecting the tissue.6
- POWERSEAL provides the selection of latch on / off, which can be chosen by user preference.
- TLH using POWERSEAL requires fewer jaw cleaning, allowing for reducing jaw cleaning time.
References
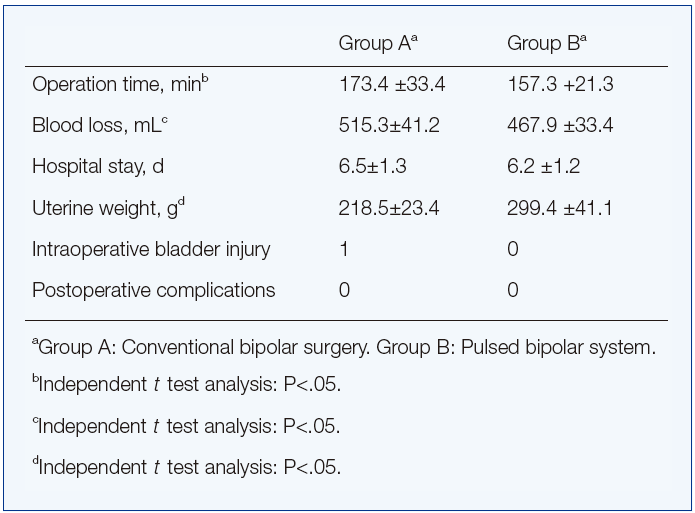
1. Batra S, et al. Comparative Analysis of Peri-Operative Outcomes Following Total Laparoscopic Hysterectomy with Conventional Bipolar- Electrosurgery versus High-Pressure Pulsed LigaSure Use. Gynecol Minim Invasive Ther. 2022;11(2):105-109.
2. Cho HY, et al. Comparison of two bipolar systems in laparoscopic hysterectomy. JSLS. 2012 Jul-Sep;16(3):456-60.
3. Pandey D, Yen CF, Lee CL, Wu MP. Electrosurgical technology: Quintessence of the laparoscopic armamentarium. Gynecol Minim Invasive Ther. 2014;3:63–6.
4. Working group of ESGE. Surgical steps of total laparoscopic hysterectomy: Part 1: Benign disease by the European Society for Gynaecological Endoscopy (ESGE) 1.
Facts Views Vis Obgyn. 2019;11(2):103-110.
5. Based on Internal Design Verification tests – DN0044249, DN0044289
6. Internal test report DN0046457
- Keyword
- Content Type