3.1 Perform En Bloc Resection | Dome Lesion
Transurethral PLASMA En Bloc Resection of NMIBC
Description
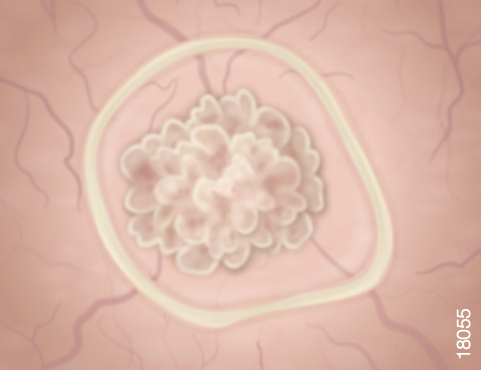
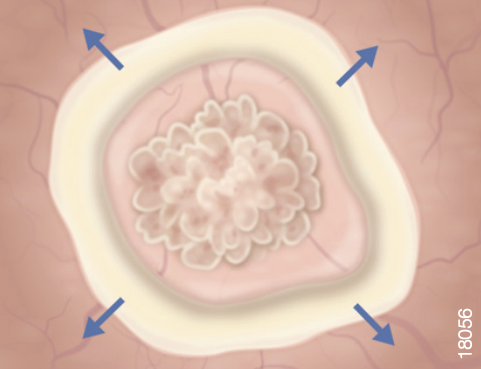
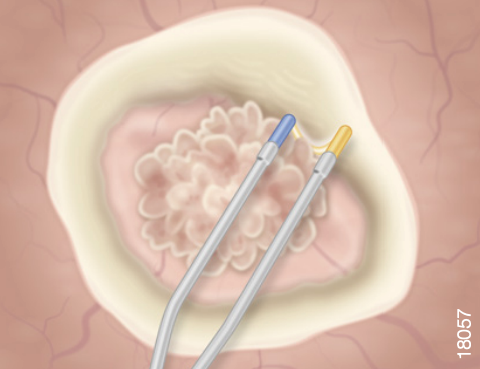
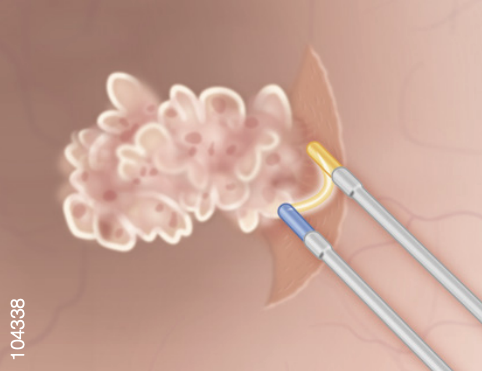
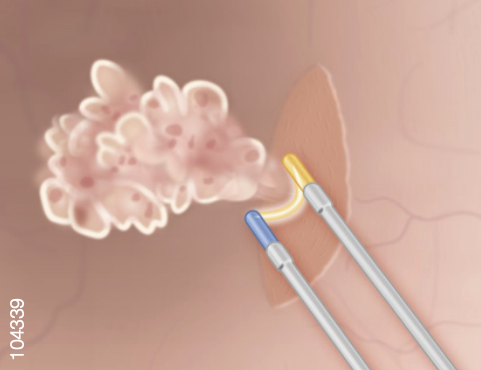
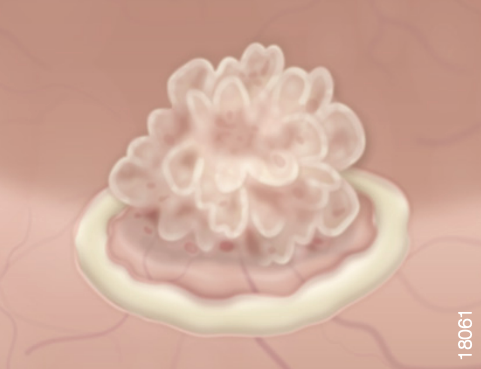
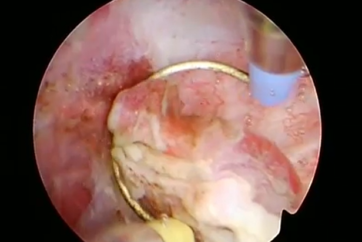
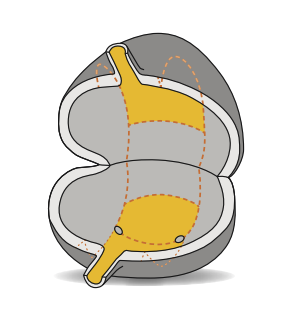
- Circumscribe the lesion at low bladder pressure (40-50 mmHg) with a coronal movement using the loop electrode.
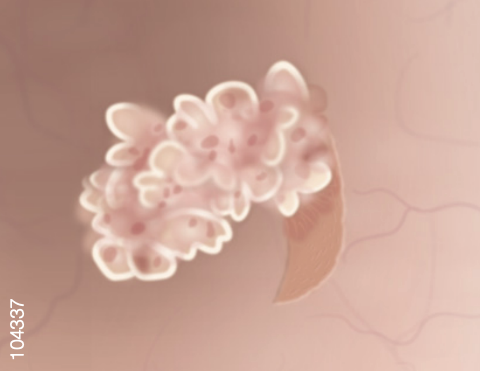
- Use the effect of hydro-dissection by filling the bladder. Then perform the final resection by sharp and blunt transverse dissection.
Key Insights
- To reduce the risk of perforation, avoid overdistension of the bladder.
Recommended Electrode:
45° angled PLASMA Loop or
PLASMA Needle Electrode.
3.2 Perform En Bloc Resection | Lateral Wall Lesion
Transurethral PLASMA En Bloc Resection of NMIBC
Description
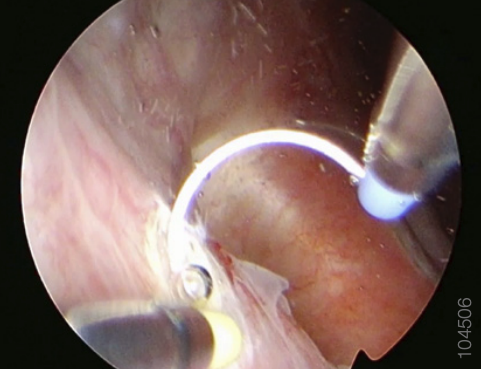
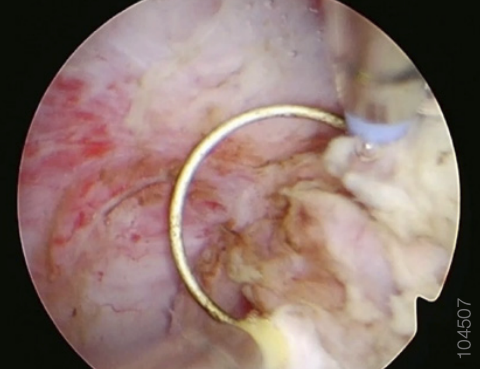
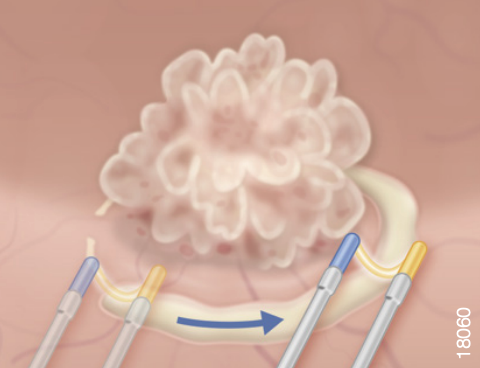
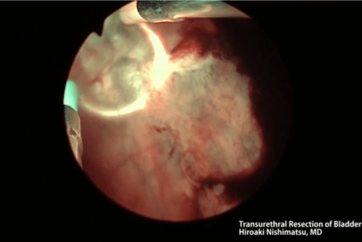
- The dissection of lateral tumors begins at the point closer to the bladder neck. Under direct vision, the plane of dissection is selected and followed with axial movements of the loop. It is helpful to lift the tumor by inserting the beak of the outer sheath underneath.
- Move the loop sideways in a lateral direction by a mix of axial and transverse movements. This will free the lateral insertion of the tumor, which will then fall down toward the media line.
- Move medially to complete the dissection by axial and transverse movements. The final steps will be to sever the last lateral attachments before retrieving the specimen.
Key Insights
- There may be a risk of obturator nerve stimulation that can be reduced by avoiding overdistension of the bladder and prevented by preoperative or perioperative obturator nerve block. Even though the use of intermittent “burst resection” cannot wholly prevent the stimulation, it helps control the extent of leg contraction.
- To reduce the risk of perforation, it may be helpful to rotate the loop so that only one prong and half of the loop cutting edge are in contact with the bladder wall.
Recommended Electrode:
PLASMA Loop or PLASMA Needle Electrode.
3.3 Perform En Bloc Resection Trigone, Anterior and Posterior Wall Lesion
Transurethral PLASMA En Bloc Resection of NMIBC
Description
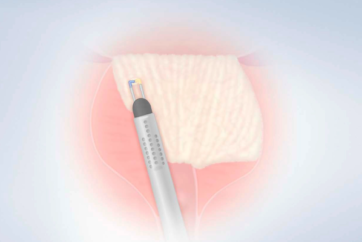
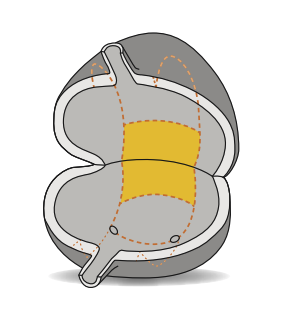
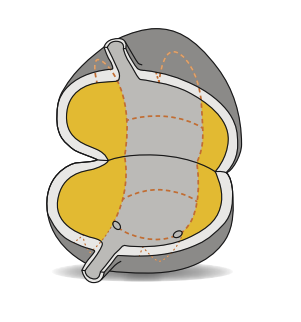
- For lesions smaller than 1.5 cm, you may first circumscribe the tumor by incising the bladder wall at the adequate depth.
- While this is readily performed for tumors located at the trigone and posterior wall, it is rarely feasible for lesions of the anterior wall, whose access by the resectoscope is hindered by the bladder neck. Using the 30° telescope there is a nice expedient to improve direct visualization of the lesion.
- Prograde dissection is then performed by successive axial movements of the loop.
Key Insights
- It is often helpful for large tumors to lift the lesion with the beak of the resectoscope in order to highlight any smooth muscle fibers attached that can then be sectioned under direct vision. In the case of the anterior wall the lesion tends to fall down, which facilitates the dissection.
- By order of difficulty, lesions located at the trigone are less challenging than those at the posterior wall. Those of the anterior wall can be even more challenging in terms of access when they arise in a large bladder or when they are close to the bladder neck and in terms of safety, as the bladder wall is thin and distensible and can be perforated in the event of overdistension.
Recommended Electrode:
PLASMA Loop or PLASMA Needle Electrode.
- Content Type