Dr. Darren Foreman

Dr. Darren Foreman is a Urologist from Adelaide, Australia. After graduating from the University of Adelaide in 1998, he completed surgical training with the Royal Australasian College of Surgeons in 2006. His private practice is South Terrace Urology and he is a senior visiting specialist at Flinders Medical Centre. He has performed flexible cystoscopy for more than 15 years and shares his experience and techniques here.
Flexible vs Rigid Cystoscopy
Better comfort for the patient
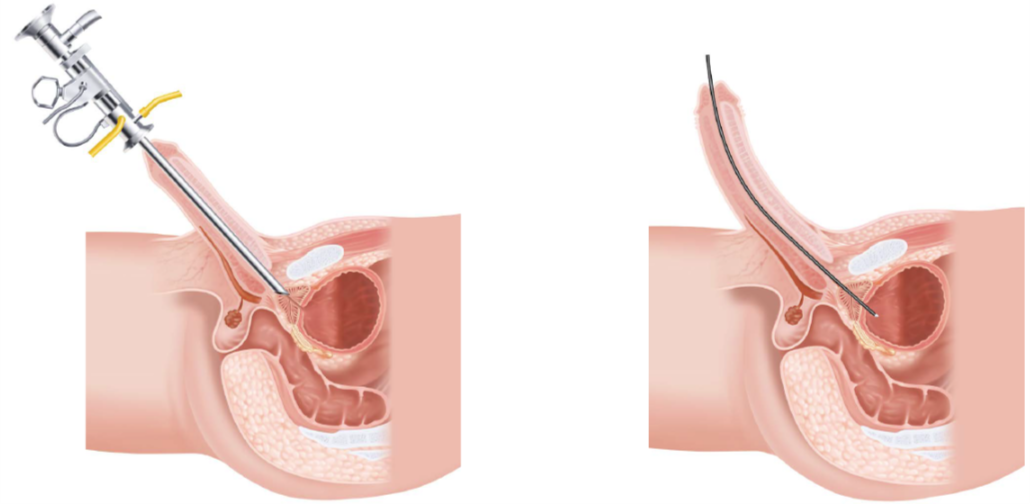
Flexible cystoscope can be inserted into the bladder without forcing the urethra to be straight unlike a rigid cystoscope. Thin and soft surface of the flexible cystoscope enables the Health Care Practitioner to practice a virtually painless and more comfortable cystoscopy.
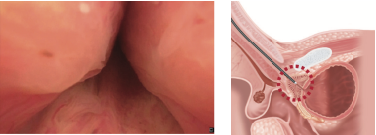
Clearer view of the trigone, bladder neck, and the prostate in men
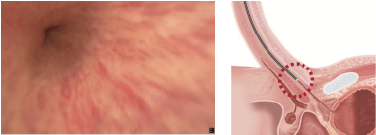
By retroflexing the scope, you get a very clear view of the trigone and bladder neck area, and the prostate in men. This area can be difficult to fully inspect using a rigid cystoscope, particularly if there is a large median lobe of prostate present.
Easier stent removal

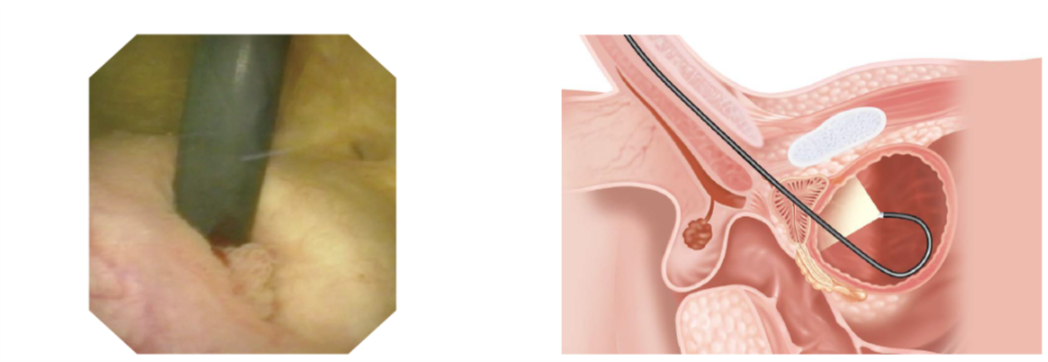
Stent removal is faster and more comfortable with a flexible cystoscope.
Procedure Highlights
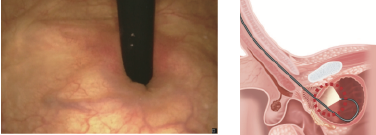
Gently hold the penis upright with your left hand, and insert the tip of the scope.
If it is difficult inserting the tip into the urethral meatus, ask nurse to support the scope by holding the light lead while using right thumb and index finger to hold the scope tip and this allows slightly more pressure to advance the scope.
Turn on the irrigation and inspect the anterior urethra as you advance the scope.
Patient needs to be relaxed and not breath holding when the scope passes through the pelvic floor.
For male patient, inspecting the prostate as the scope passes is often uncomfortable, therefore inspect this area after finishing the bladder inspection as you are retracting the scope.

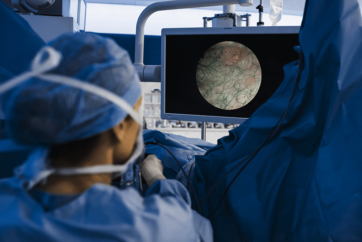
Wait for the bladder to adequately distend, turn off the irrigation and then systematically inspect each wall, the dome and ureteric orifices.
Use a combination of thumb movement to deflect the scopes tip, with rotation of the wrist to turn the scope to each side.
Advance the scope towards the dome and pull down your thumb all the way to retroflex it.
This allows excellent visualization of the trigone and bladder neck, and the prostate in men. This is a view you don’t see when using a rigid cystoscope.
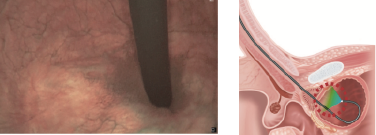
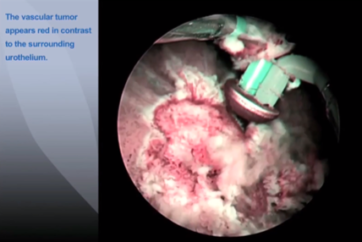
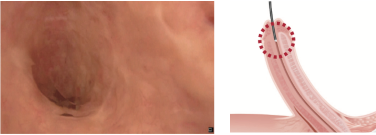
For patients with a history of bladder transitional cell carcinoma, change to NBI™ technology mode and repeat the procedure.
Particularly look for surface structures with fine capillary patterns which may represent small tumors.
Disclaimer: NBI™ technology is not intended to replace histopathological sampling as a means of diagnosis.

Turn the irrigation back on as retracting the scope into the prostatic urethra. Once inspected, have a final review of the anterior urethra as the scope is withdrawn fully.
- Keyword
- Content Type