Author

Dr. Jun Miki, Department of Urology, Jikei University Kashiwa Hospital
Biography
Graduated from Jikei University School of Medicine in March 1998. Worked for the International Medical Center of Japan and Jikei University Hospital, then moved on as a postdoctoral fellow at the Center for Prostate Disease Research, Maryland, USA for three years starting in 2004. Since 2012, Dr. Miki has worked in the Department of Urology, Jikei Kashiwa Hospital, and has been serving as an associate professor since January 2018. Specializes in laparoscopic surgery of urological malignancies, including prostate cancer, bladder cancer, and renal cancer.
Extended Lymph Node Dissection and Sentinel Lymph Node Identification in Prostate Cancer
Extended pelvic lymph node dissection (ePLND) has been recommended in various guidelines for cases where there is a certain possibility of lymph node metastasis in intermediate and high risk localized prostate cancer. However, even in past studies showing diagnostic significance, the specific scope, classification, and techniques of dissection have not been standardized. In fact, ePLND can be said to be a difficult surgical technique as it treats the complicated anatomical structure of the pelvic region, such as the iliac vessels and the obturator nerve. Furthermore, with concerns about extensive operation time and increased complications, it is undeniable that ePLND may have different indications and quality of surgery depending on facilities and surgeons.
The mainstream approach to examining the sentinel lymph node (SLN) in prostate cancer has been to use radioactive isotopes, of which the significance has not been established, and which can hardly be said to be widely used due to complicated techniques and equipment issues. The fluorescence coloring method of exciting indocyanine green (ICG) with infrared (IR) has already been used to identify SLN in breast cancer and malignant melanoma in actual clinical use. In recent years, its use in prostate cancer has also been occasionally reported.
Target and ICG Administration Method
Our institution targets ePLND in laparoscopic total prostatectomy for intermediate or high risk localized prostate cancer cases. After the introduction of general anesthesia, about 3 mL of ICG 0.25 mg/mL is injected into the prostate using a 23 G needle under transrectal ultrasound guidance in a lithotomy position.
Regardless of tumor location, ICG is injected evenly from the apex to the base of the peripheral zone of the prostate. IR observation is performed before radical prostatectomy since observation would be difficult if the lymph flow is disrupted by a surgical operation.
Operative Procedure
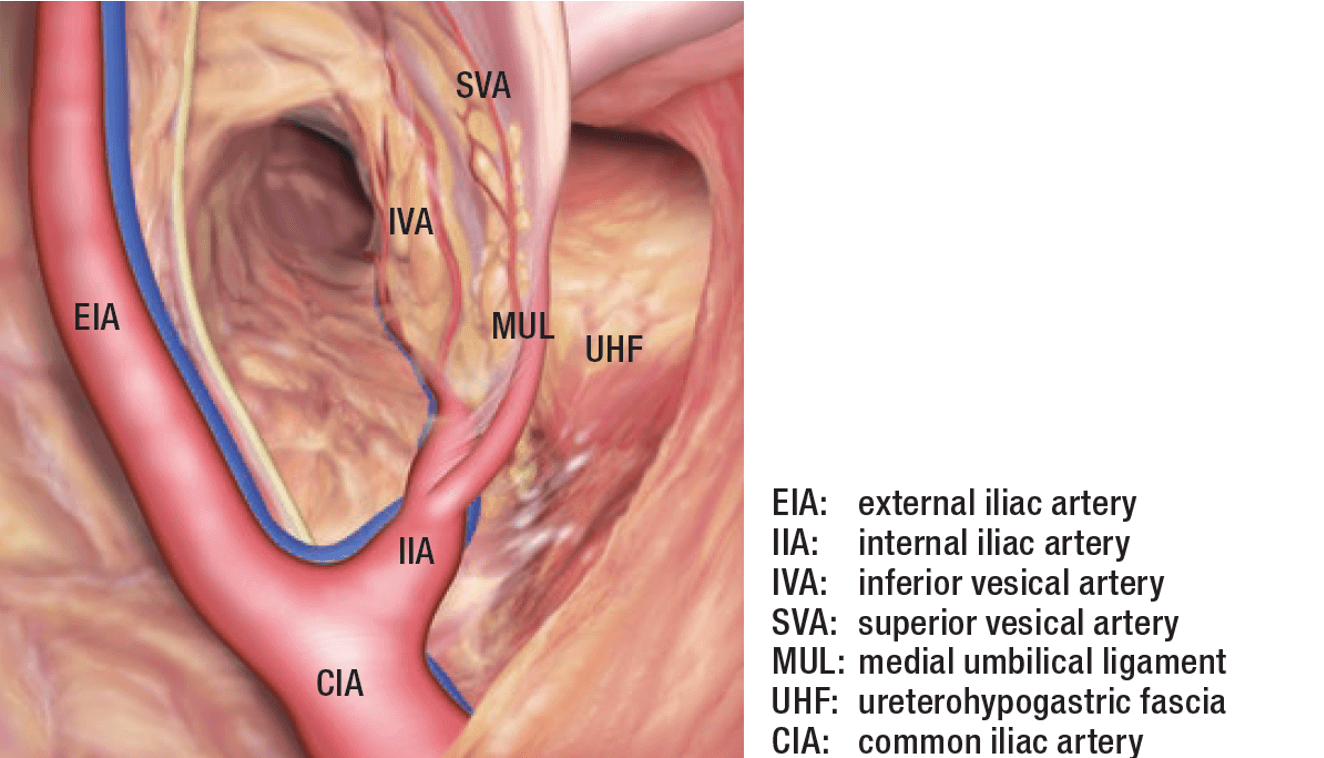
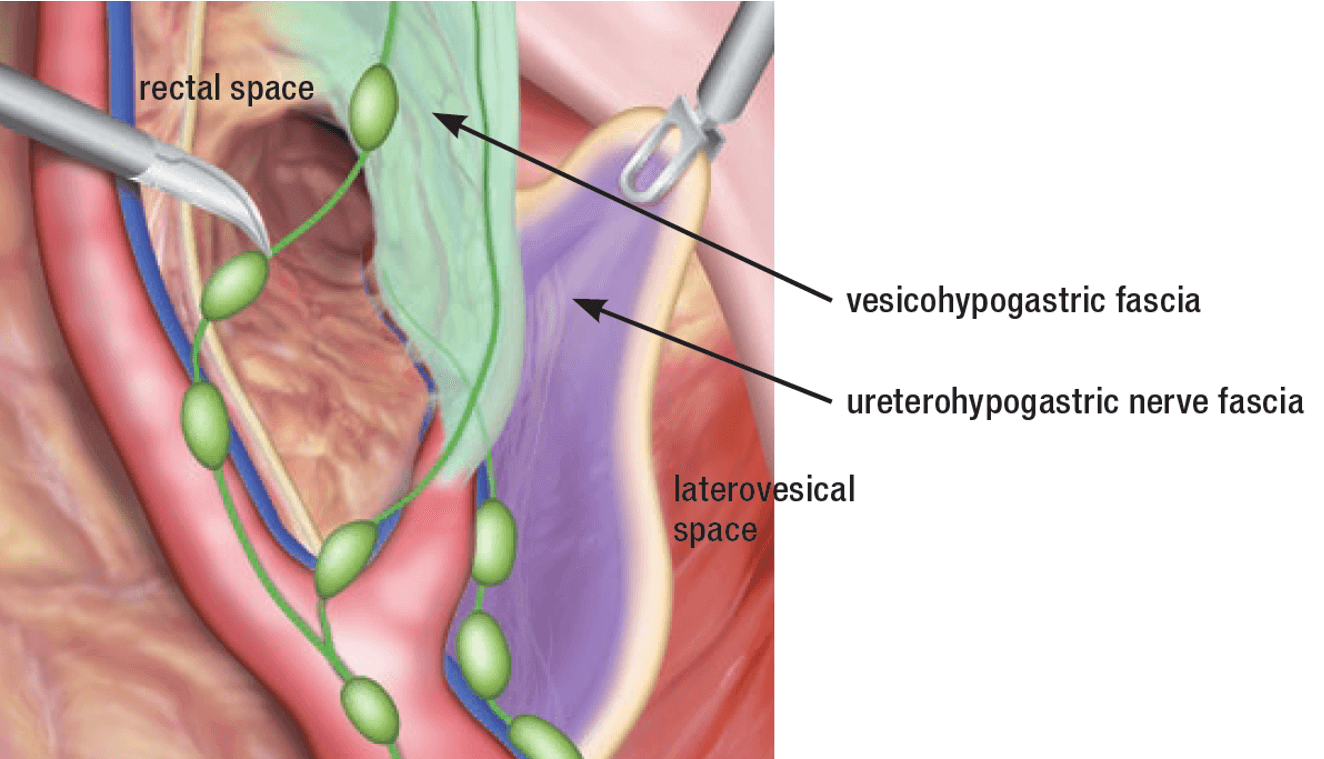
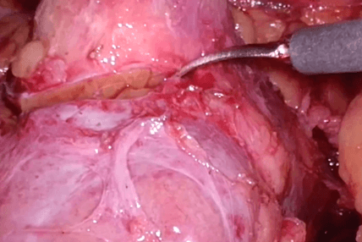
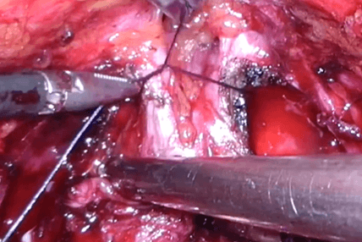
We consider the identification of SLN and the securing of an optimal surgical field for ePLND(Figure 1) are important to the procedure. To achieve this, layer dissection and development of the space based on pelvic membrane anatomy are required. First, the laterovesical space is developed at the proper layer. The medial umbilical ligament, which is the first branch of internal iliac artery, is surrounded by vesicohypogastric fascia, forming the partition-like inner wall of the laterovesical space(Figure 2). The latervesical space is developed just outside the medial umbilical ligament, which can be seen through the peritoneum, as a merkmal. At the deepest part, the internal iliac bifurcation can be found. By ligating and dissecting the spermatic cord and widely developing the laterovesical space, the space between obturator region and internal iliac region can be developed, and obturator nerve and external iliac vein injuries can be prevented.
Next, just inside the origin of the medial umbilical ligament from the internal iliac artery, the rectal space is developed at the ureter covered by ureterohypogastric nerve fascia as a boundary. The ureter can be completely freed while covered by the ureterohypogastric nerve fascia and the ePLND region will be outside the fascia since the pelvic nerve plexus is located medially and ventrally from the ureteral hypogastric nerve. Therefore, the outside of the rectal space and the inside of the laterovesical space will be the internal iliac region where basically all the prostate lymph flows pass through.
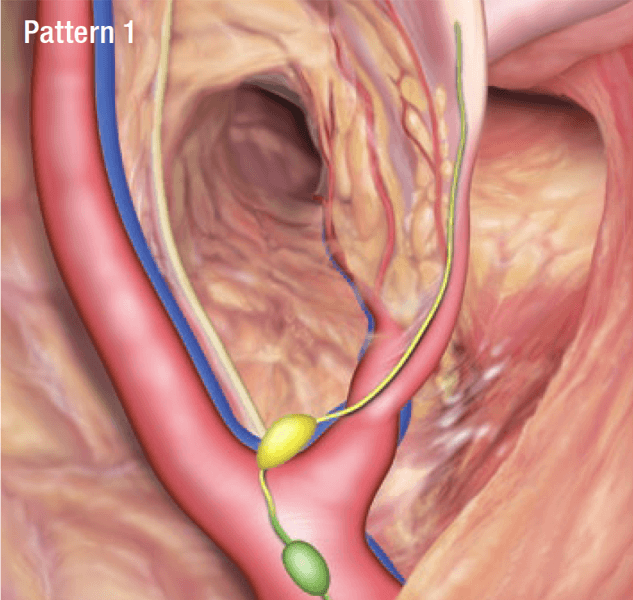
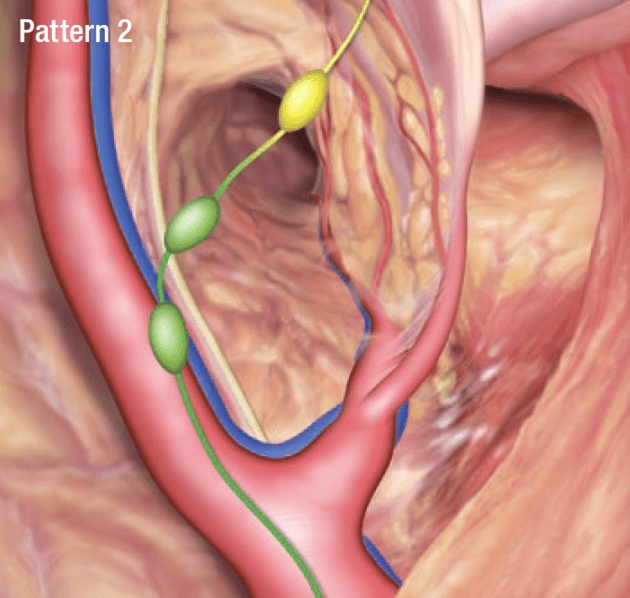
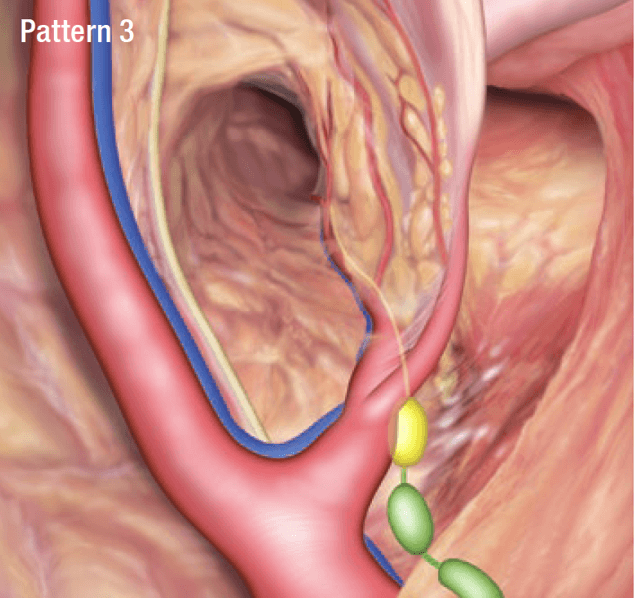
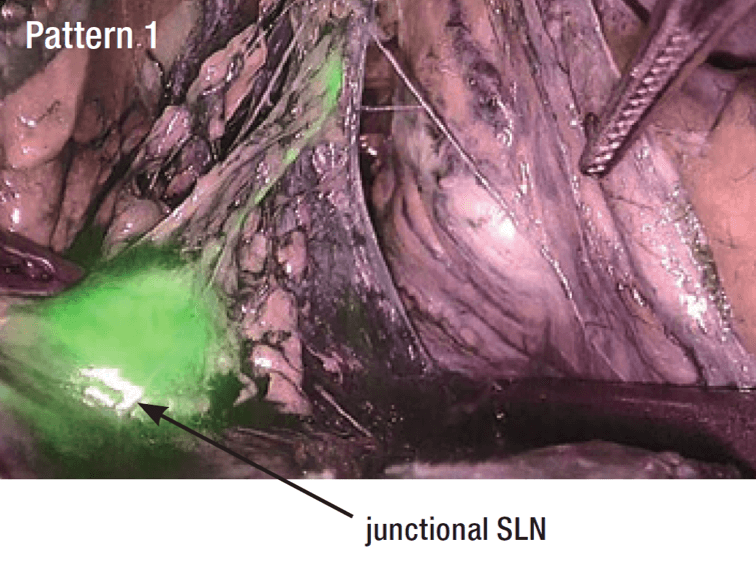
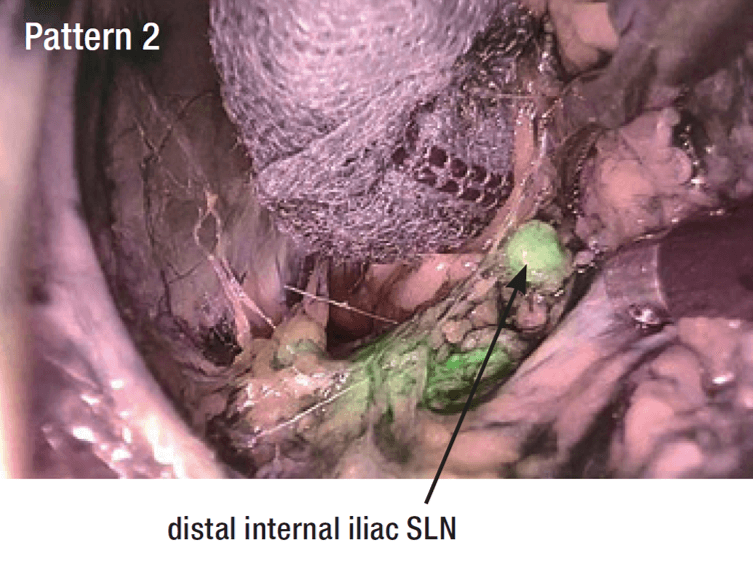
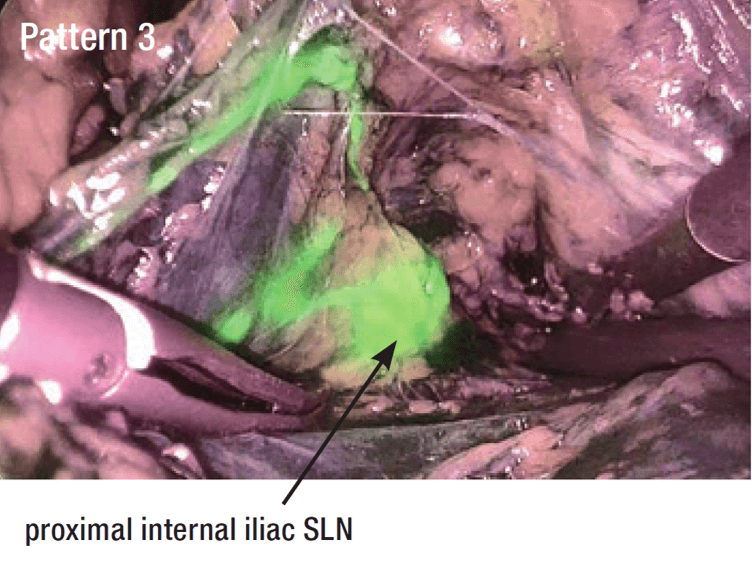
Prostate Lymph Flow Patterns and by IR Observation (Figures 3 and 4)
As a result of our study, three prostate lymph flow patterns were identified.
In pattern 1, the lymph flow runs and descends laterally alongside the medial umbilical ligament, via SLN in the vicinity of the internal iliac artery bifurcation (junctional SLN) as the first SLN, and continues laterally and cranially.
In pattern 2, the lymph flow runs from the dorsal side of the prostate alongside the inferior vesical artery, via the distal internal iliac SLN in the vicinity of the origin of the inferior vesical artery, and continues through the obturator region laterally and cranially.
In pattern 3, unlike patterns 1 and 2, the lymph flow runs and ascends alongside the medial internal iliac artery (internal pudendal artery) via the proximal internal iliac SLN in the vicinity of the origin of the medial umbilical ligament, and continues ascending alongside the medial common iliac artery to the presacral region.
The actual IR observations using an IR observation system features lymph flows and lymph nodes that can be clearly identified by fluorescence with a good field of view in which normal structures, such as blood vessels and nerves, and forceps can be fully confirmed (Figure 4).
Conclusion and Cautions
The region of ePLND has been cranially expanded in terms of scope from obturator-only localized dissection to the internal, external, and common iliac regions. In our study, the main prostatic lymph flow passes through the internal iliac region lymph nodes, and those SLN in the vicinity of the prostate such as junctional SLN, distal internal iliac SLN were considered as the most frequent sites of metastasis. However, this study found varied frequency in lymph flow patterns, requiring further examination in consideration of patient selection bias, ICG injection techniques, and cancer condition.
The SLN identification method using IR enabled visual identification of lymph flow and lymph nodes, suggesting possibilities for establishing surgical techniques based on anatomical structure, which may avoid unnecessary lymph node dissection.
As of March 2018, it should be noted that the use of ICG for fluorescent imaging to identify sentinel lymph nodes in prostate cancer is currently off-label use in some countries including Japan.
- Content Type