Pancreatobiliary case 5

Dr. Haruka Toyonaga
Chief physician of the Gastroenterology Center at Teine Keijinkai Hospital, Keijinkai Medical Corporation, Japan
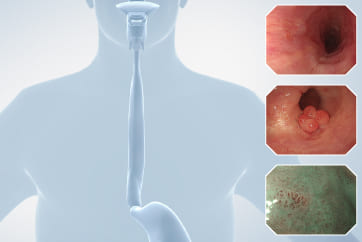
Image processing techniques applicable to biliopancreatic endoscopy: TXI and RDI
TXI and RDI can be used with the 290 series and later models.* TXI is compatible with the TJF-Q290V side-viewing endoscope, while RDI can be used with the SIF-H290S single-balloon enteroscope.
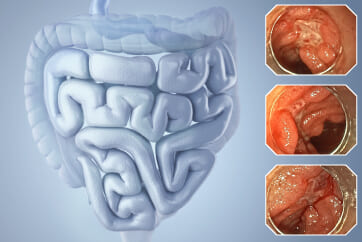
TXI is an image processing technology that enhances visibility by emphasizing structure (texture), brightness, and color tone. It offers Mode 1, which emphasizes all three elements, and Mode 2, which reduces emphasis on color tone (Fig. 8). Mode 2 provides a more natural color tone closer to WLI, allowing comfortable use over extended periods without discomfort. We typically switch to Mode 1 after using Mode 2 when they need to further emphasize color tones.
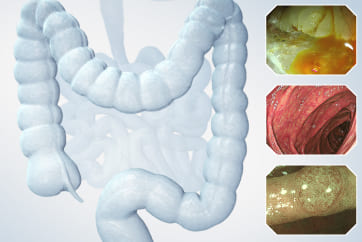
RDI is an IEE that RDI utilizes differences in the reflection and absorption characteristics of hemoglobin at light wavelengths to enhance visibility by providing contrast for blood and blood vessels. Three types of light sources ・Red (630nm), Amber (600nm), and Green (540nm) ・are used, and Modes 1-3 are available depending on the degree of color enhancement (Fig. 9).1 In areas where the blood concentration is low, both Red and Amber light are reflected, resulting in an orange appearance. However, in areas with higher blood concentration, the reflection of Amber light is reduced, making these areas appear red. This contrast makes it easier to identify the presence and location of active bleeding. To make bleeding points more visible, Mode 2, which emphasizes Red more, is primarily used.
*and 190 series.
Clinical Applications of TXI
TXI enhances visibility by emphasizing structure, brightness, and color tone. In general endoscopic procedures, understanding anatomy and structure is crucial, and TXI is believed to be a significant aid in this regard. In normal papilla, it is also useful for identifying the bile duct orifice, identifying the bile duct orifice during precutting, and identifying stenosis at the biliary-enteric anastomosis. Furthermore, in tumors of the papilla, enhanced visibility of lesion boundaries and bile duct orifice is expected.1
1) Recognition of the Bile Duct Orifice
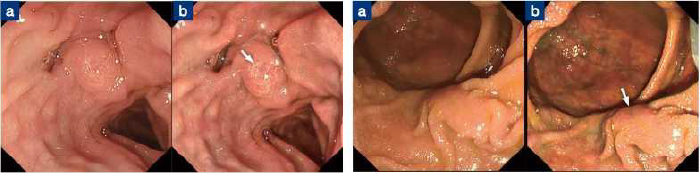
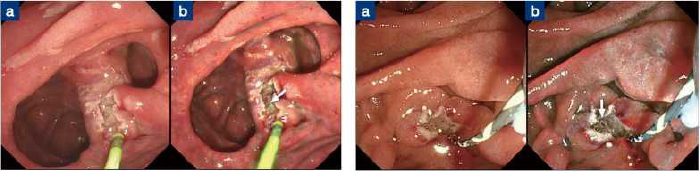
The recognition of the bile duct orifice becomes easier with the emphasis on the depressions and elevations of the bile duct opening, facilitating the identification of papillary shape and opening. Especially in cases like flat-type papillae (Fig. 10) and intraductal papillae (Fig. 11, Video)2 in Case 1, even when the bile duct opening is not clearly visible under white light (WLI), TXI enables clearer visibility.
Fig. 11: Insertion into intraductal papilla using TXI Mode 2
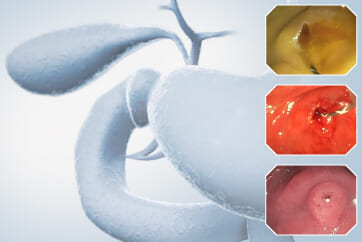
2) Needle knife precut
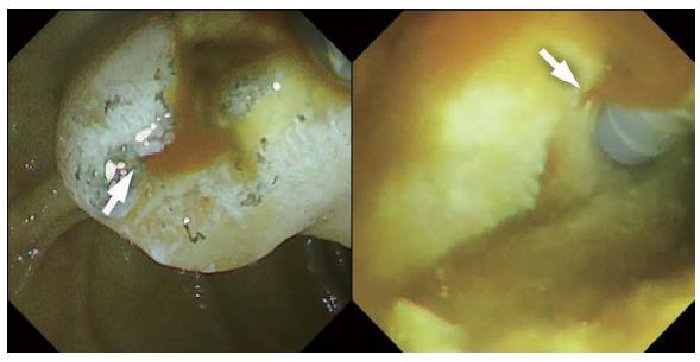
In cases of difficult bile duct cannulation, there are also cases that require Needle-knife precut. First, incise the duodenal mucosa at the enlarged papillary portion to expose the submucosal layer, and identify the white, band-like elevation believed to be the Oddi sphincter. Next, gradually extend the incision around the Oddi sphincter, exposing the red-colored bile duct mucosa believed to be the bile duct orifice, and place a catheter to facilitate drainage. After precut, the incision site often has poor visibility, making identification of the bile duct orifice difficult. However, TXI enhances visibility of structures such as elevations and depressions, as well as color tones, making it useful for recognizing the Oddi sphincter and bile duct orifice (Fig. 12, 13, Video).2,3
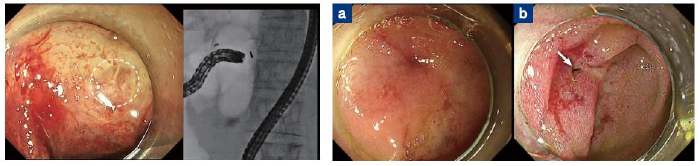
a. Performing Precut after bile duct stent placement under WLI, b. TXI Mode 2 emphasizes the irregularities on the post-Precut incision surface, clarifying the bile duct orifice (arrow)
[Fig. 13] Precut under challenging conditions with restricted scope position due to cancer at the pancreatic head
a. Performing Precut with the bile duct guide wire in place under WLI, b. TXI Mode 1 emphasizes the bile duct orifice (arrow) for improved visibility
Fig. 13: Recognition of the bile duct orifice on the precut incision surface using TXI Mode 1
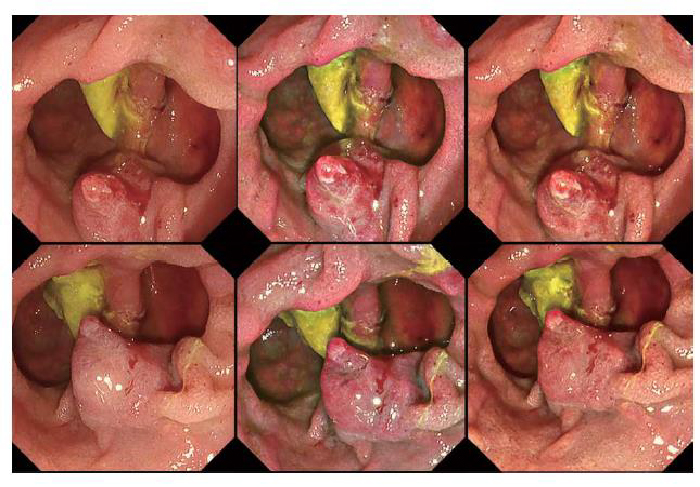
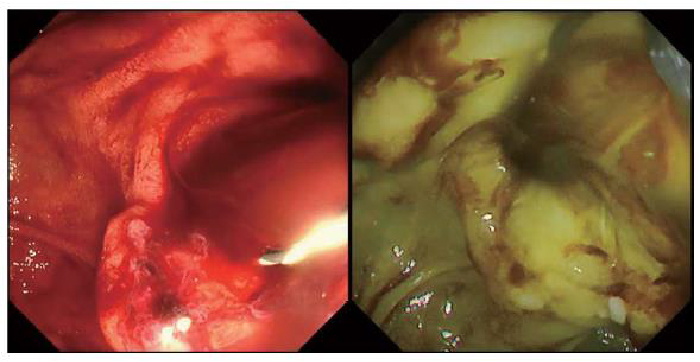
3) Biliary-enteric anastomosis/Pancreatico-enteric anastomosis
Narrowing of the biliary-enteric anastomosis/pancreatico-enteric anastomosis associated with cholangitis and pancreatitis has been reported to benefit from balloon endoscopic therapy, but identification of the anastomotic site is often challenging. In cases where the anastomotic site is small or occluded, it is important to identify subtle mucosal structures and changes in color tones. The SIF-H290S allows the use of TXI, which enhances imaging and enables clearer visualization of mucosal structural changes suggesting an anastomotic site. Referring to CT/MRCP, cases where the biliary-enteric anastomosis could not be identified for over 30 minutes using WLI alone were successfully identified using TXI (Fig. 14, Video).4 Moreover, in cases where the pancreatico-enteric anastomosis was buried in folds and difficult to visualize, TXI enabled clearer visibility (Fig. 15, Video).4
Inserted with the SIF-H290S, but not visible with WLI despite prolonged exploration. Switching to TXI Mode 2 enabled identification of the anastomotic site (circle)
[Fig. 15] a.Pancreatico-enteric anastomotic stenosis under WLI, b. Enhanced visibility of the anastomotic site with TXI Mode 1 (arrow)
Fig. 14: Identification of the biliary-enteric anastomosis using TXI Mode 2
Fig. 15: Identification of the biliary-enteric anastomosis using TXI Mode 2
4) Recognition of Tumor Boundaries in Duodenal Papilla Tumors
In exposed papillary tumors, predicting malignancy from surface structures, diagnosing the extent of lateral spread, and identifying the bile duct orifice during cannulation are crucial. Additionally, in cases such as intradiverticular papillary tumors or extensive lateral spread, it can be challenging to visualize the extent of lateral spread. TXI enhances imaging, making it easier to evaluate the boundaries and structure of lesions (Fig. 16).5 Since the spread into the diverticulum was not extensive, and EUS confirmed no invasion into the bile/pancreatic ducts or duodenum, endoscopic papillectomy was performed.
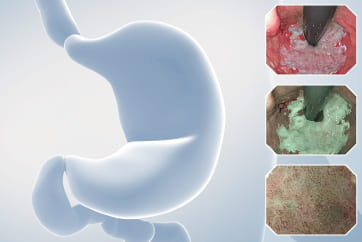
Clinical Applications of RDI
Under WLI, blood appears uniformly red, making it difficult to distinguish between bleeding points and pooled blood. However, with RDI, the contrast between different shades of blood between red and orange makes it easier to identify bleeding points and determine whether bleeding is ongoing. Additionally, reducing the overall redness on the screen decreases the psychological burden on the operator.1
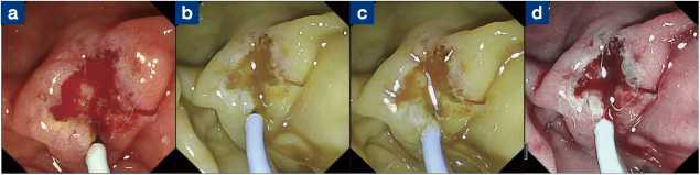
1) Identification of Bleeding Points
In post-EST bleeding, visibility is often obscured by pooled blood, but using RDI helps differentiate pooled blood, which appears as light orange, from actively bleeding blood, which appears as dark red. This allows for pinpoint identification of bleeding points, and effective hemostatic treatment can be administered at the same site. (Fig.17, Video)6
Furthermore, combining the Gel immersion technique by filling the lumen with gel helps maintain a clear field of view without blood diffusion, facilitating clearer identification of bleeding points. (Fig.18, Video)7
Fig. 17: Identification of post-EST bleeding sites using RDI Mode 2
Fig. 18: Identification of post-EST bleeding sites using RDI Mode 2 and the gel immersion method
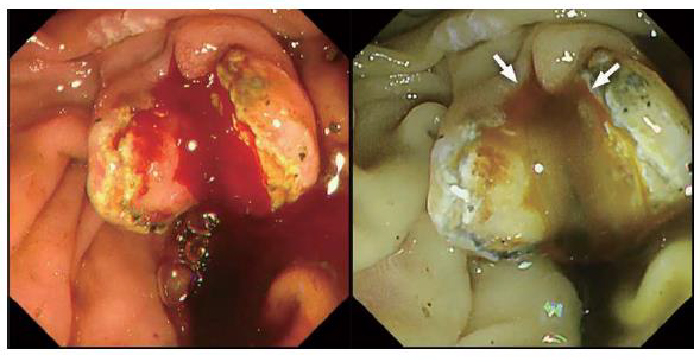
2) Confirmation of Hemostasis
Sometimes it can be difficult to determine whether “bleeding is ongoing” or if it has stopped with blood components adhering. By using RDI, attention can be focused on whether there is sustained orange-colored flow indicating fresh blood, allowing for determination of the presence of bleeding. With WLI, continuous red fluid leakage suggested ongoing bleeding. However, RDI identified the fluid as brown in color, indicating it was old blood mixed with bile accumulated in the bile duct rather than fresh blood (Fig. 19, Video).1,6
Fig. 19: Confirmation of hemostasis post-EST bleeding using RDI Mode 2
Future of TXI/RDI
This report introduces the features and improvements of the TJF-Q290V along with the utility of TXI and RDI in biliary and pancreatic endoscopic treatment, illustrated with case examples. The TJF-Q290V incorporates various functions and its high performance allows for successful completion of procedures even in challenging cases. As an IEE enhancing visibility during procedures, TXI/RDI has been integrated into EVIS X1, contributing to improved clarity during procedures. TXI is particularly beneficial for beginners in understanding the structure of the duodenal papilla and remains useful for experts during complex cases and precut procedures. RDI has emerged as a specialized IEE that alters color tones to reduce psychological stress and enhance visibility of bleeding points, making it valuable in hemostasis. Future reports are expected to demonstrate its clinical effectiveness, aiming to enhance safety and efficiency in the challenging field of biliary and pancreatic endoscopic therapy, ultimately providing optimal medical care for patients.
References
1. Toyonaga H, Hayashi T, Hama K et al. Recent advancements in image-enhanced endoscopy in the pancreatobiliary field. DEN Open 2024; 5: e382.
2. Toyonaga H, Kin T, Hayashi T et al. The application of texture and color enhancement imaging in transpapillary biliary cannulation. Endoscopy 2022; 54: E786-7.
3. Toyonaga H, Kin T, Yamazaki H et al. Visibility of the biliary orifice after precut papillotomy : Comparison between white light imaging and texture and color enhancement imaging. J Hepatobiliary Pancreat Sci. 2024. doi: 10.1002/jhbp.12005. [Online ahead of print]
4. Toyonaga H, Kin T, Nakamura R et al. Successful detection of choledochojejunal and pancreaticojejunal anastomotic strictures using a novel form of texture and color enhancement imaging. Endoscopy 2022; 54: E1062-3.
5. Toyonaga H, Hayashi T, Katanuma A. Usefulness of texture and color enhancement imaging in the endoscopic management of duodenal ampullary tumors. Digestive Endoscopy 2023; 35: e109-10.
6. Nakamura R, Toyonaga H, Katanuma A. Feasibility of red dichromatic imaging in hemostasis for post-endoscopic sphincterotomy bleeding. Digestive Endoscopy 2022; 34: e157-8.
7. Toyonaga H, Hayashi T, Nakamura R et al. Effective application of self-assembling peptide matrix with the gel immersion technique and red dichromatic imaging for hemostasis of postendoscopic sphincterotomy bleeding. Endoscopy 2023; 55: E72-3.
Any content or information (“Content”) presentedherein is illustrative in nature and does not guarantee or represent specific information, outcomes, or results. Olympus Medical Systems Corp. and its parents, subsidiaries, affiliates, directors, officers, employees, agents, and representatives (collectively “Olympus”) does not represent to or warrant the accuracy or applicability of the Content. Under no circumstances shall Olympus be liable for any costs, expenses, losses, claims, liabilities, or other damages (whether direct, indirect, special, incidental, consequential, or otherwise) that may arise from, or be incurred in connection with, the Content or any use thereof.
- Keyword
- Content Type