Disclaimer:
- TXI™, RDI™, and BAI-MAC™ Technologies are not intended to replace histopathological sampling as a means of diagnosis
- The positions and statements made herein by Dr. Tam are based on Dr. Tam’s experiences, thoughts and opinions. As with any product, results may vary, and the techniques, instruments, and settings can vary from facility to facility. The content hereof should not be considered as a substitute for carefully reading all applicable labeling, including the Instructions for Use. Please thoroughly review the relevant user manual(s) for instructions, risks, warnings, and cautions. Techniques, instruments, and setting can vary from facility to facility. It is the clinician’s decision and responsibility in each clinical situation to decide which products, modes, medications, applications, and settings to use.
- The BF-H1200 used in this case is not available in the US market at this time nor is there an established time for its release. The safety and effectiveness of this product and or the use of these products has not yet been established in the United States market.
- The EVIS X1™ endoscopy system is not designed for cardiac applications. Other combinations of equipment may cause ventricular fibrillation or seriously affect the cardiac function of the patient. Improper use of endoscopes may result in patient injury, infection, bleeding, and/or perforation. Complete indications, contraindications, warnings, and cautions are available in the Instructions for Use (IFU)
- Dr Tam, the authoring physician(s) of this presentation, are/ is a paid consultant(s) to Olympus Corporation.
Scope: BF-H1200
Patient information: Male, 78 years old
Medical history: Known metastatic NSCLC and concomitant mycobacterium abscessus colonization near the primary at lingular segment. On second-line line gemcitabine-platinum doublet with good response.
Reason for bronchoscopy:
Differential radiological responses to chemotherapy over lingular shadows. Bronchoscopy was arranged to differentiate between disease progression vs. mycobacterium infection.
Known LMB orifice tumor partially covering the LLL opening.
New tumor nodule noted over LC (between LB1+2 & LB3) – biopsied
Foreign body seen inside LB3a (between LB3ai & LB3aii) – removed
LB3c pEBUS-GS TBBX performed according to pre-procedural planning.
Diagnosis:
LC (between LB1+2 & LB3) EBBX biopsy – Suspicious of malignancy
LB3a (between LB3ai & LB3aii) foreign body analysis – Consistent with bone, foreign in nature
LB3c TBBX biopsy – Suspicious of malignancy
Culture (BAL & LB3c TBBX): No growth of Mycobacterium
Treatment:
Continue with chemotherapy treatment
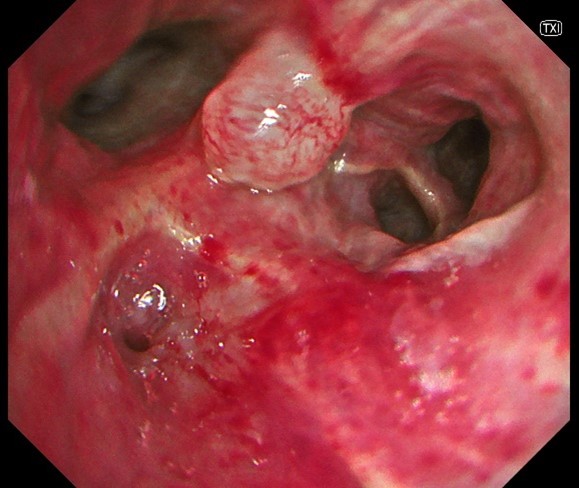
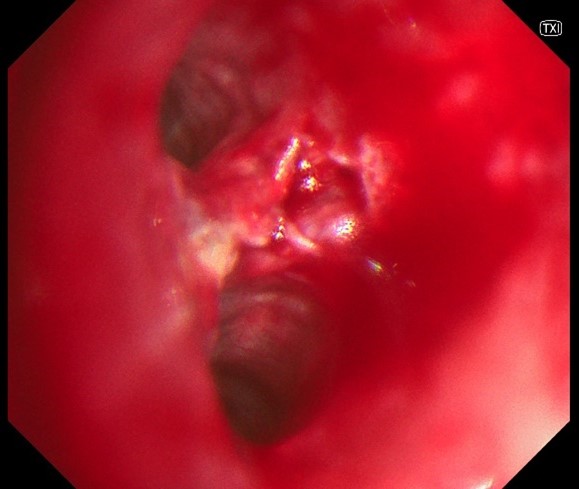
1. WLI vs. TXI™ technology observation
Generalized mucosal changes at 6 o-clock position over this short segment of LUL bronchus extending to the orifice of LB1+2c. The irregularities were much more appreciable with the use of TXI™ technology imaging.
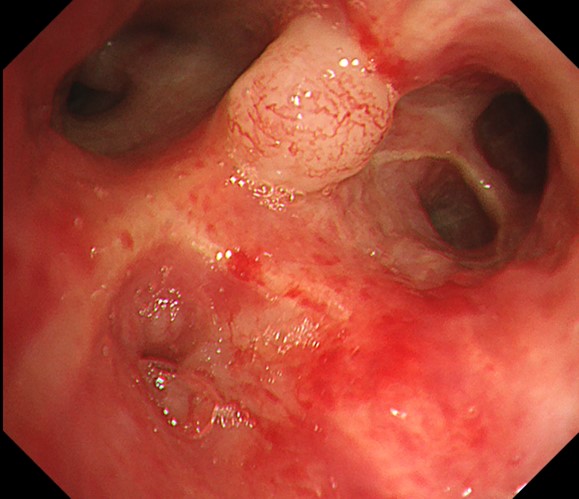
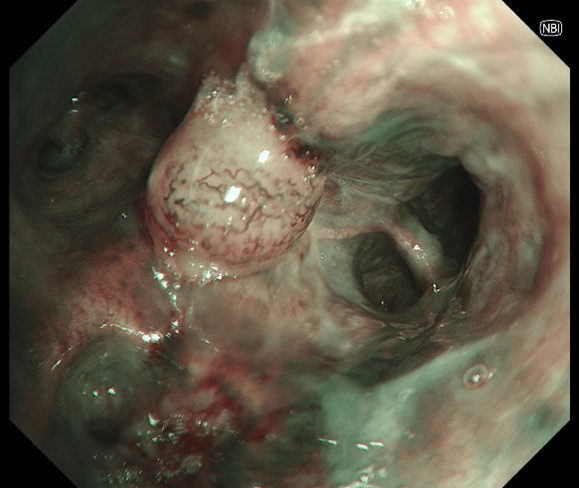
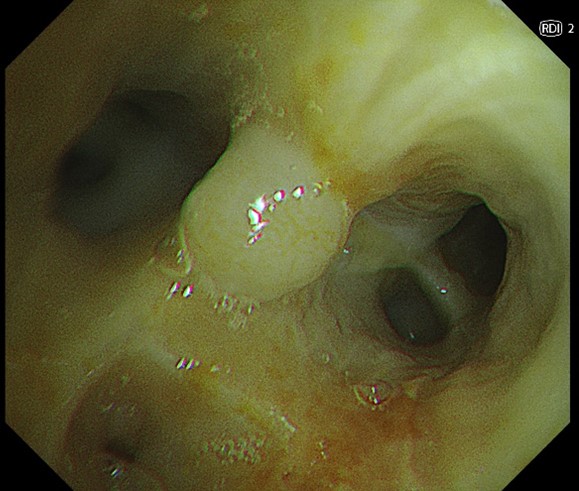
2. NBI™ vs. RDI™ technologies observation
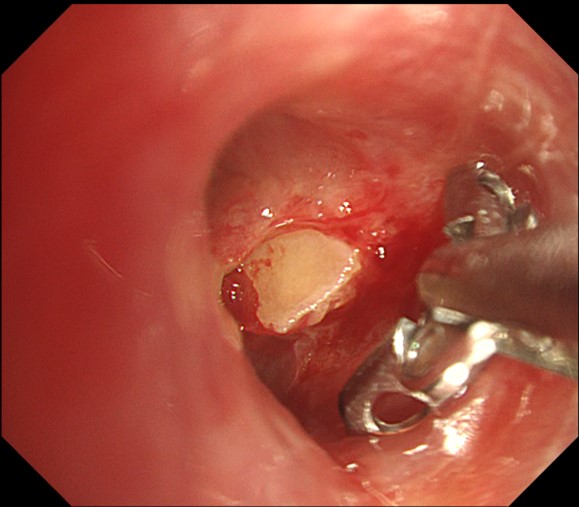
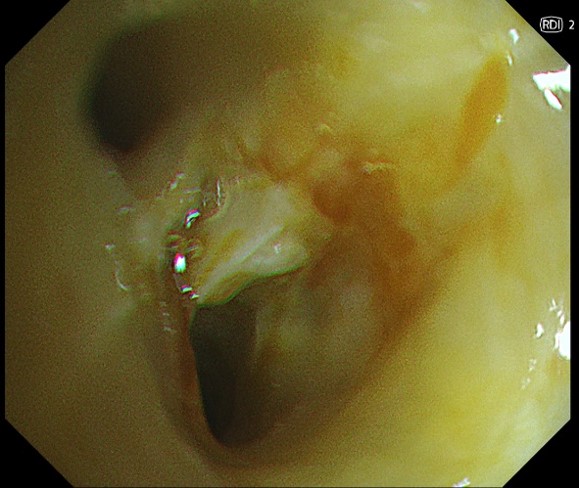
New tumor nodule over LC (between LB1+2 & LB3). NBI™ technology showed significant neo-vascularization, but the lack of deeper mucosal vessels on RDI™ technology over the central part of the nodule help assure that EBBX is safe.
3. WLI vs. RDI™ technology observation
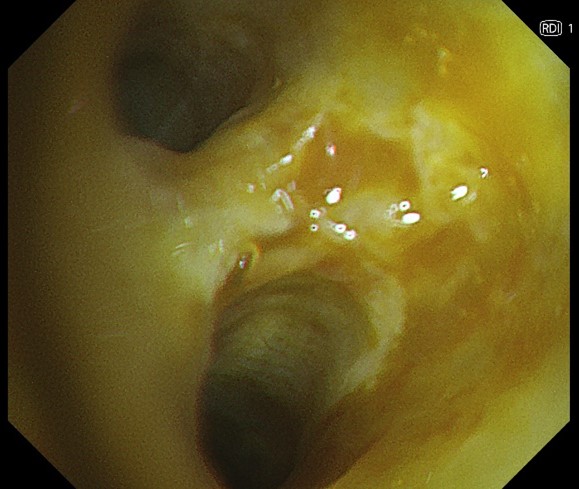
Foreign body seen inside LB3a with some slow bleeding. RDI™ technology confirmed no vessel encroachment at deeper level around the foreign body.
4. RDI™ vs. TXI™ technologies observation
Multiple attempts were tried before the foreign body was successfully removed. RDI™ technology mode confirm that the only source of (mild) bleeding is from where the foreign body had previously impacted.
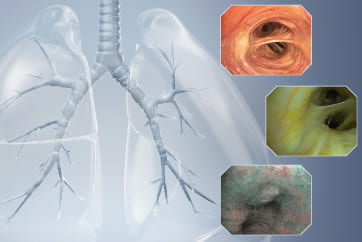
Case video
LB3c is shown at 1 o’clock position in the video clip. With BAI-MAC™ imaging on, the distal branching pattern within LB3c can be clearly seen from more than 2 bifurcations away (contrast this with the loss of detail when BAI-MAC™ technology was transiently turned off earlier in the clip). Pre-procedural planning had localized the pathology of interest with in LB3a & LB3c, but CT resolution was otherwise inadequate for more detailed planning; details picked up BAI-MAC™ technology imaging facilitating the decision to include LB3c pEBUS TBBX as part of the sampling procedure.
Overall Comment
BAI-MAC™ technology mode seems particularly suited to facilitate the observation of distant branching pattern in bronchoscopy, which is very useful in peripheral/navigational bronchoscopy procedure. Keeping the BAI-MAC™ technology mode turned on throughout the procedure does not otherwise seems to have an adverse effect on performance.
TXI™ technology mode gives a slightly better appreciation of subtle mucosal changes compared to white light, but bronchoscopist might need to acclimatize to the new ‘red hue’ that can dominate the palette when there is significant surrounding inflammation or after local bleeding.
NBI™ technology is not a new imaging modality and continues to be useful in identifying neovascularization pattern; the vessels pickup looks even more obvious than previous generation.
RDI™ technology mode is very useful in confirming the absence, or the position of, deeper mucosal vessels to guide the site for safer endobronchial biopsy.
* Specifications, design and accessories are subject to change without any notice or obligation on the part of the manufacturer
- Keyword
- Content Type