Colorectal ESD

Dr. Yutaka Saito, Endoscopy Division, National Cancer Center Hospital
Dr. Yutaka Saito took part in the development of ITknife nano in collaboration with Dr. Hiroyuki Ono. He believes that ITknife nano will contribute to faster and safer ESD in the colon.
Features and benefits of ITknife nano
Developing a suitable ITknife for the colon
Colorectal and esophageal ESD is considered technically difficult because of anatomical characteristics such as thin muscle layer. Because of this, the risk of perforation in these areas is higher than in gastric ESD. To minimize the risk of perforation during colorectal ESD, I greatly prefer to use ITknife as it is easy to manipulate. However, I found the size of the insulated tip would not allow smooth insertion of the knife into the submucosal layer of the colon since the mucosa and submucosa are thin. Therefore, further development was required to enable efficient use of the ITknife in the colon. Due to the minimized size of its insulated tip, ITknife nano is better suited for use in the colon and esophagus than conventional ITknives. With its smaller tip, ITknife nano can easily slip into the submucosal layer, resulting in faster dissection during colorectal ESD. Even though the needle-type knife has good cutting capability, it is necessary to cut difficult-to-see areas little by little since the tip of the knife may cauterize the tissue.On the other hand, the insulated tip of ITknife nano provides security, so more aggressive cutting becomes possible. In addition, the cutting range of a needle-type knife and ITknife nano differs. Since ITknife nano cuts with both the electrode and knife while the needle-type knife tends to cut only with the tip of the knife, more tissue can be cut at one time with ITknife nano. Another beneficial feature of ITknife nano is the sheath. The stiff sheath of ITknife nano helps to lift up the lesion. This is very useful when checking the cutting line during dissection.
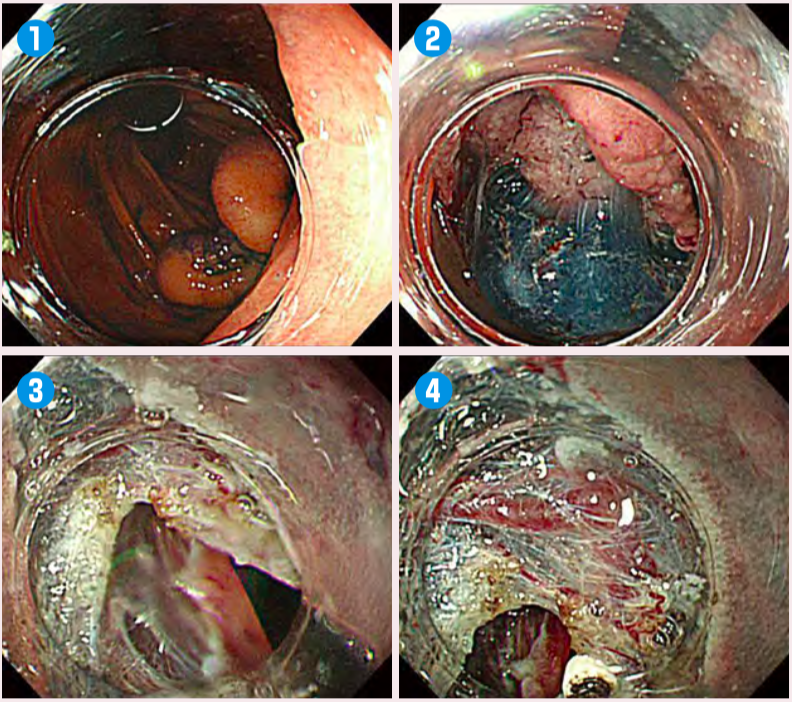
Fig.1:Easy to slip the knife under the submucosal layer
Use the retroflection of the endoscope and injection(1, 2)to make the submucosal layer visible. Use the attachment to slide the endoscope under the edge of the lesion(3)and then slide ITknife nano(4).Combine ITknife nano with a needle-type knife
Though ITknife nano was developed to be a suitable knife for the colon, it is still difficult to complete colorectal ESD with this knife alone. Because of the presence of peristalsis, folds and bends in the colon, some colorectal ESD cases may require more accurate control for cutting. Furthermore, for lesions with strong fibrosis, a needle-type knife is more suitable due to its little-by-little cutting style. For these cases, a combination of ITknife nano and a needle-type knife is the best way to perform efficient colorectal ESD.
Tips for colorectal ESD
Difference between colorectal and gastric ESD strategies
The strategy for colorectal ESD in our facility differs from the one used in gastric ESD. Instead of performing circumferential incision, we perform partial incision and dissection and repeat these steps. Also, we use the retroflexed position for the endoscope and start from the distal side. After we finish 50‒80% of the dissection, we change the endoscope to the straight position and continue incision and dissection from the proximal side. In most cases, we change again to the retroflexed position near the end to finish the procedure in a more stable position.
Visual confirmation of the submucosal layer
To dissect the submucosal layer safely, it is important to secure a safe margin by efficient submucosal injection. Obtaining countertraction by utilizing the force of gravity is also effective.
In addition, it is important to visually confirm the submucosal layer using a distal attachment.
With colorectal ESD, the dissection plane differs from gastric ESD. While the dissection plane for gastric ESD is right above the muscle layer, it is in the lower 1/3 of the submucosal layer for colorectal ESD. It is important to leave a small part of the submucosal layer during dissection in colorectal ESD to prevent perforation.
For large lesions, the key to safe resection is to repeat the following steps: 1) slide ITknife nano below the lesion, 2) lift it to confirm the cut surface and 3) cut. I believe that performing dissection cautiously in this manner will lead to a reduction of the risk of complications such as perforation to almost 0% even in difficult cases.
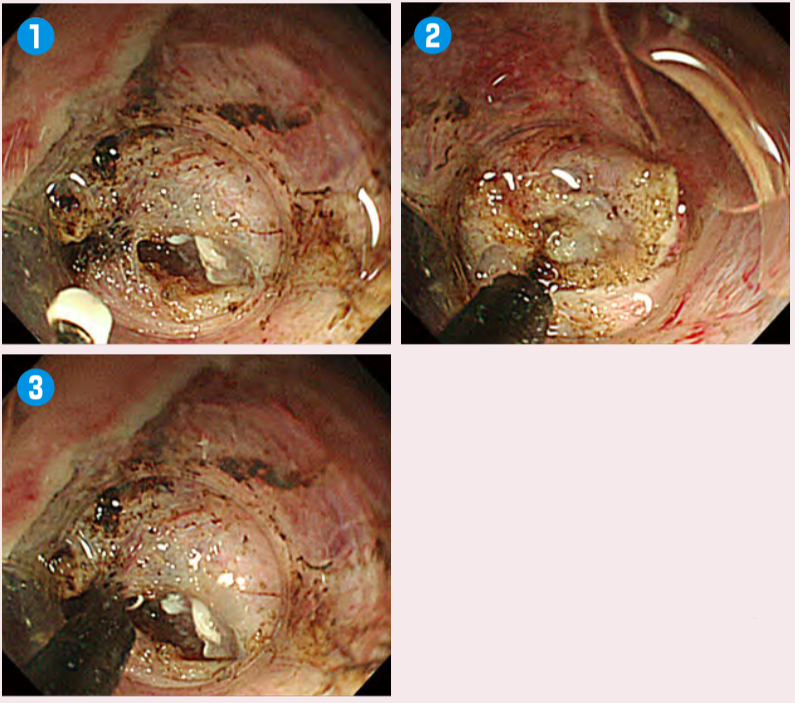
Fig.2:Visual confirmation of the submucosal layer
Push ITknife nano(1)into the area where the tunnel has been created(2). Before sliding the knife in parallel to the muscle layer, apply upward traction on the lesion to confirm the surface to be resected(3).Factors that make colorectal ESD difficult
One of the factors that makes colorectal ESD a difficult procedure is the existence of folds in the colon. When the lesion is located over a fold, it is necessary to check the contours of the fold carefully to avoid cutting the wrong area. Even with ITknife nano, perforation can easily occur if dissection is made in the wrong place.
For colorectal ESD using ITknife nano, we need to slide the knife smoothly over the fold by frequently using the endoscope in a retroflexed position. For that reason, ESD should be performed by imaging the dissection plane over the fold in 3 dimensions. The same technique is used when performing ESD on a lesion over the angular region of the stomach.
Another of the factors making colorectal ESD difficult is the paradoxical movement of the endoscope in the hepatic or splenic flexure. Where the endoscope cannot be properly controlled, the procedure in this position should be entrusted to a skillful endoscopist; even then, if the endoscope cannot be controlled in this instance, a contrivance such as the use of a sliding tube should be adopted, or ESD should not be performed if circumstances dictate. In the worst cases of perforation, where closure using clips is difficult, an emergency operation will be necessary.
On the other hand, ITknife nano is the knife to choose in cases where the endoscope is not stabilized. Compared to needle-type knives, you need not worry about cutting or damaging the lesion unintentionally using ITknife nano due to its insulated tip, which can also be used to hook and fix the lesion.
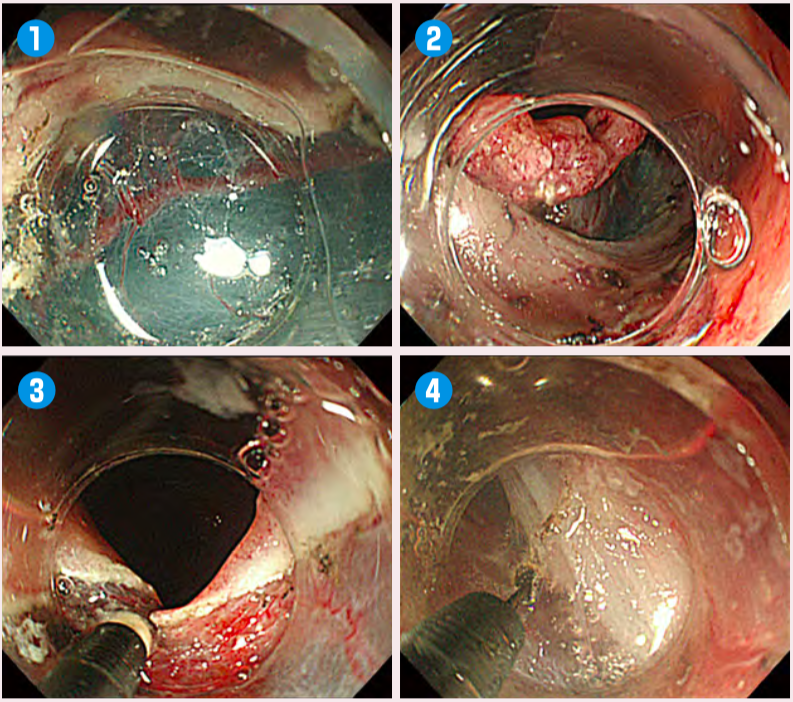
Fig.3:Submucosal dissection for lesion with folds
Use the attachment so that the submucosal layer can be seen directly(1). Pull the endoscope slightly to confirm the direction of the muscle layer from a short distance(2). Then, use the attachment to enter beneath the edge of the lesion(3)and slide ITknife nano into this area. The tip here is to slide the knife in parallel to the muscle layer(4)to prevent damage to the muscle layer. During dissection of the fold, imagining the contour of the muscle layer is essential.For safe colorectal ESD
2 cm can be a reference size for ESD
Although many colon tumours can be removed with piecemeal resection without any problem, LST non-granular type and 0-IIc LST-similar lesions, particularly those over 2cm, should be resected en bloc because they often have high degrees of malignancy and SM invasion rate.
In en bloc resection of a lesion larger than 2cm, the perforation risk is lower with ESD than with EMR, provided that the optimum device and procedure are used. If you attempt to remove a large tumour en bloc by force using a snare, unintentional perforation may occur. At our facility, we have 120–130 cases/year of flat lesions over 2cm and large Is villous lesions that require colorectal ESD. We have approximately 300 cases/year of early cancer and 1000 cases/year of whole colonoscopy treatment if we include polypectomy. As a result, colorectal ESD accounts for approximately 10% of whole colonoscopy treatments. Of course, this differs depending on the characteristics of each facility.
The biggest advantage of colorectal ESD is that it can remove early carcinoma by means of endoscopy, without going through surgery. Before the introduction of ESD, approximately 20% of intramucosal cancers had to be removed surgically due to technical difficulties, particularly if they were large lesions. However, the introduction of ESD reduced the percentage of intramucosal cancers treated surgically to just 1% in our facility. These lesions were indicated for surgery because they were circumferential lesions which lead to the problem of stricture. Today, almost any lesion diagnosed as intramucosal can be removed endoscopically, regardless of the tumour size. In theory, it should be possible to remove intramucosal lesions of 5-10 cm with an endoscope.
Safety is the first priority
Nevertheless, a large Is villous tumour still remains one of the most difficult cases for colorectal ESD.
Such lesions sometimes have fibrosis or disarrayed muscle plate. Moreover, there are some cases when the muscle layer is raised, making it impossible to anticipate the dissected plane. As these cases are accompanied with a high risk of perforation and because invasion depth is difficult to diagnose, they should be handled by a specialized facility or by switching to laparoscopy. Naturally, collaboration with the surgery department is indispensable.
To perform safe colorectal ESD, it is important to understand the risk, properly control the environment, and gain experience.
Setting
| Electrosurgical unit | Treatment | Setting |
|---|---|---|
| ESG-100 | Mucosal Incision | PulseCut 25W |
| Submucosal Dissection | ForcedCoag2 25W | |
| VIO 300D | Mucosal Incision | DryCut, Effect3, 100W |
| Submucosal Dissection | SwiftCoag, Effect2, 50W |
- Content Type