Colorectal Case 19

Disclaimer:
NBI™ and TXI™ technologies are not intended to replace histopathological sampling as a means of diagnosis
The positions and statements made herein by Dr. Ho Dang Quy Dung are based on Dr. Ho Dang Quy Dung’s experiences, thoughts and opinions. As with any product, results may vary, and the techniques, instruments, and settings can vary from facility to facility. The content hereof should not be considered as a substitute for carefully reading all applicable labeling, including the Instructions for Use. Please thoroughly review the relevant user manual(s) for instructions, risks, warnings, and cautions. Techniques, instruments, and setting can vary from facility to facility. It is the clinician’s decision and responsibility in each clinical situation to decide which products, modes, medications, applications, and settings to use.
*Information regarding competitor products is presented to the best of our knowledge as of the date of presentation. This material does not constitute medical or legal advice and should not be relied upon as such. It should not be considered as a substitute for carefully reading all applicable labeling, including the Instructions for Use. Please thoroughly review the relevant user manual(s) for instructions, warnings and cautions.
The EVIS X1™ endoscopy system is not designed for cardiac applications. Other combinations of equipment may cause ventricular fibrillation or seriously affect the cardiac function of the patient. Improper use of endoscopes may result in patient injury, infection, bleeding, and/or perforation. Complete indications, contraindications, warnings, and cautions are available in the Instructions for Use (IFU)
*Information regarding competitor products is presented to the best of our knowledge as of the date of presentation. This material does not constitute medical or legal advice and should not be relied upon as such. It should not be considered as a substitute for carefully reading all applicable labeling, including the Instructions for Use. Please thoroughly review the relevant user manual(s) for instructions, warnings and cautions. Techniques, instruments and setting can vary from facility to facility, and it is the clinician’s decision and responsibility in each clinical situation to decide which mode and settings to use.
1) Data on file with Olympus (DC00489968)
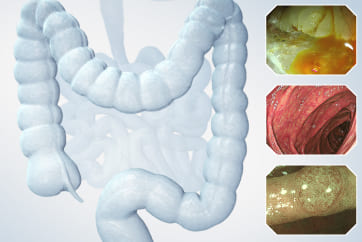
Scope: CF-EZ1500DL
Organ: Transverse colon
Patient information: 69 years old, Male
Medical history: No related diseases
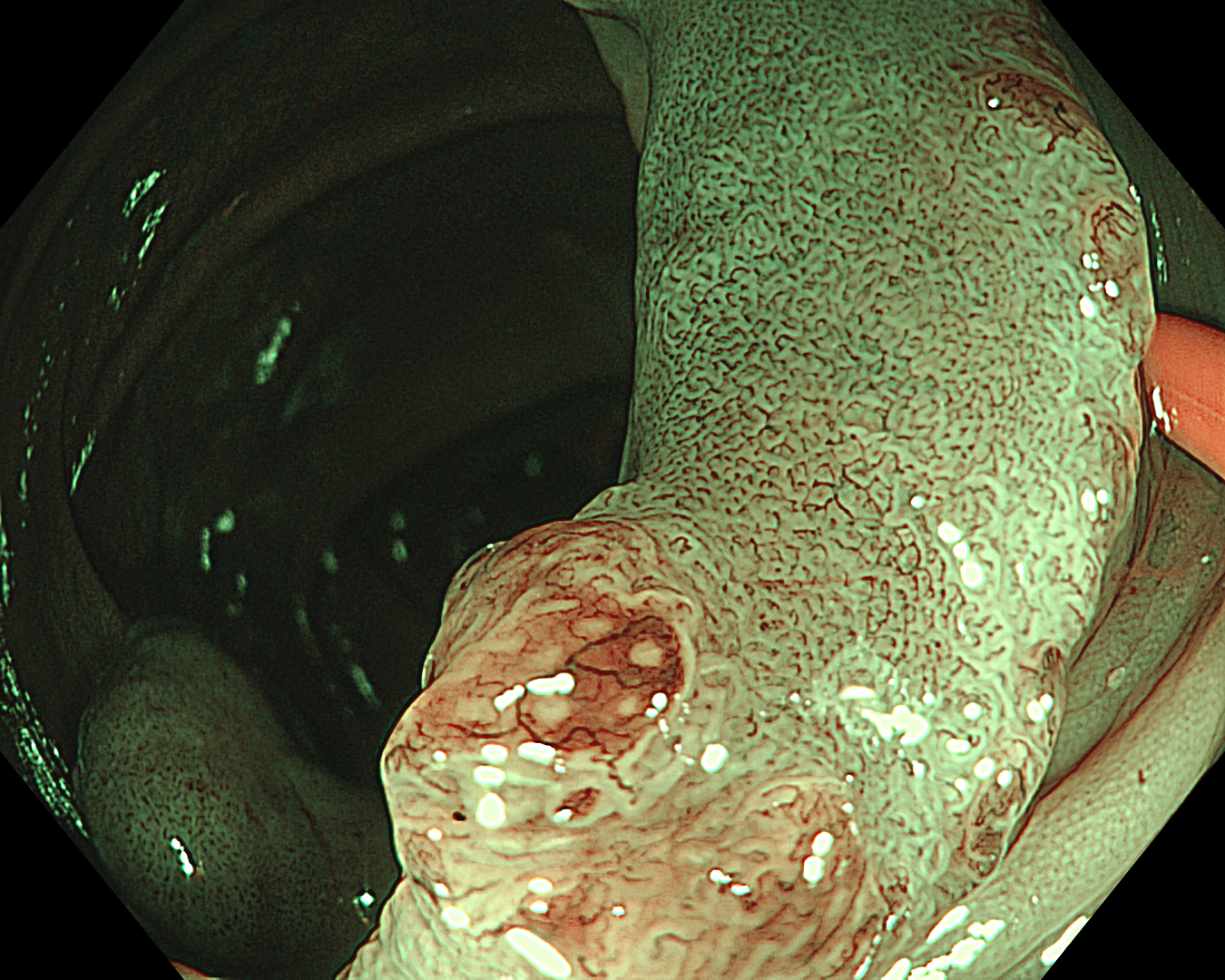
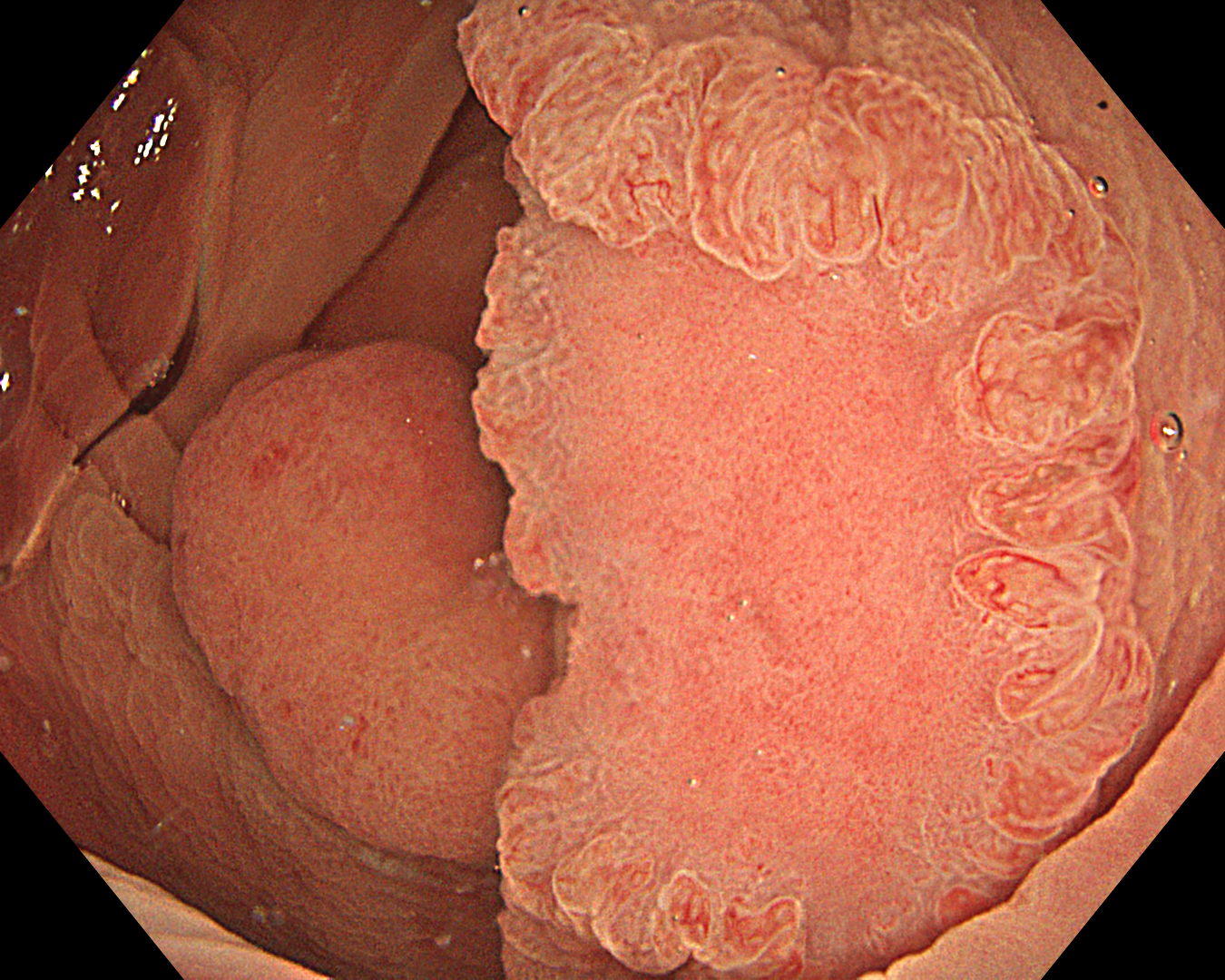
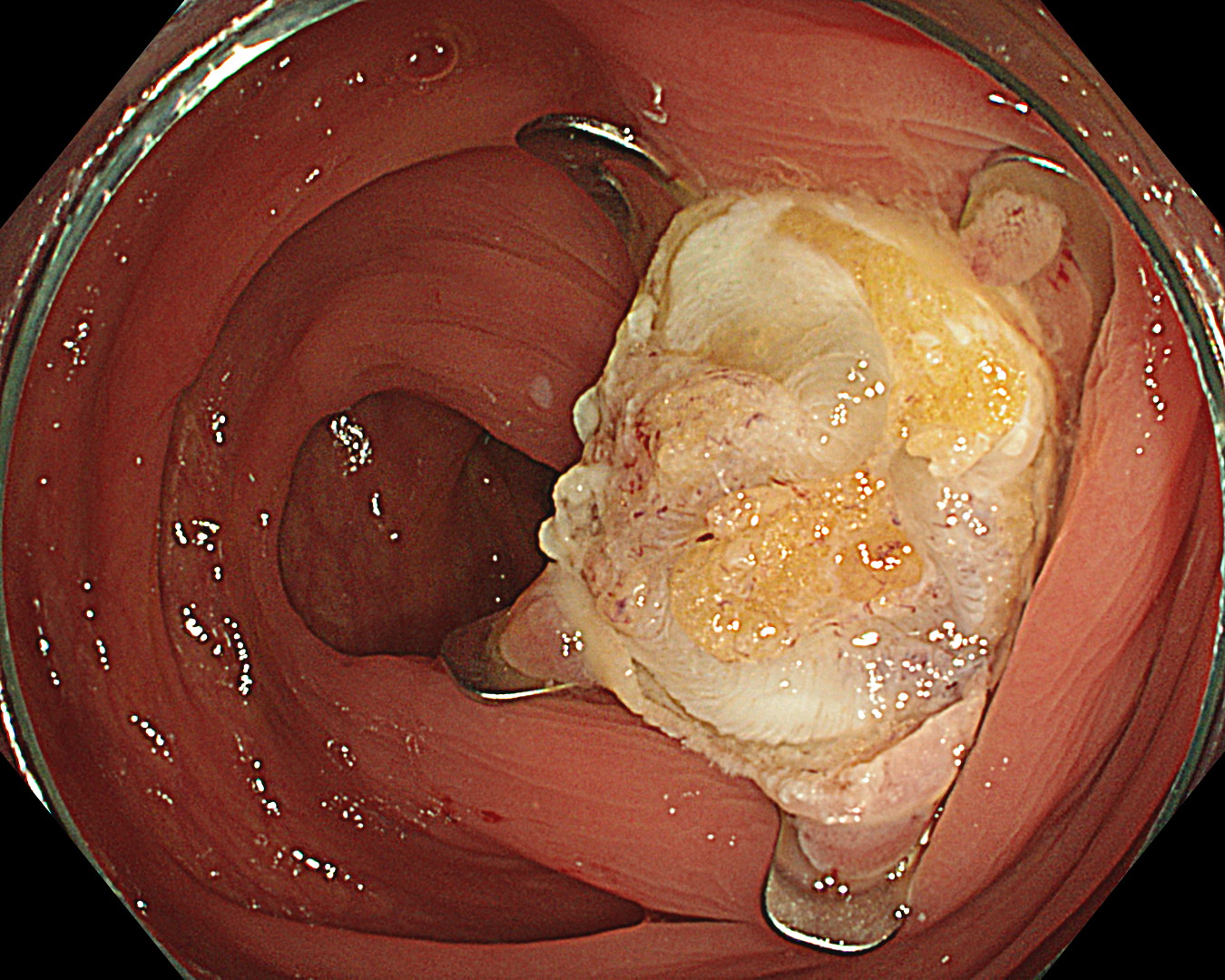
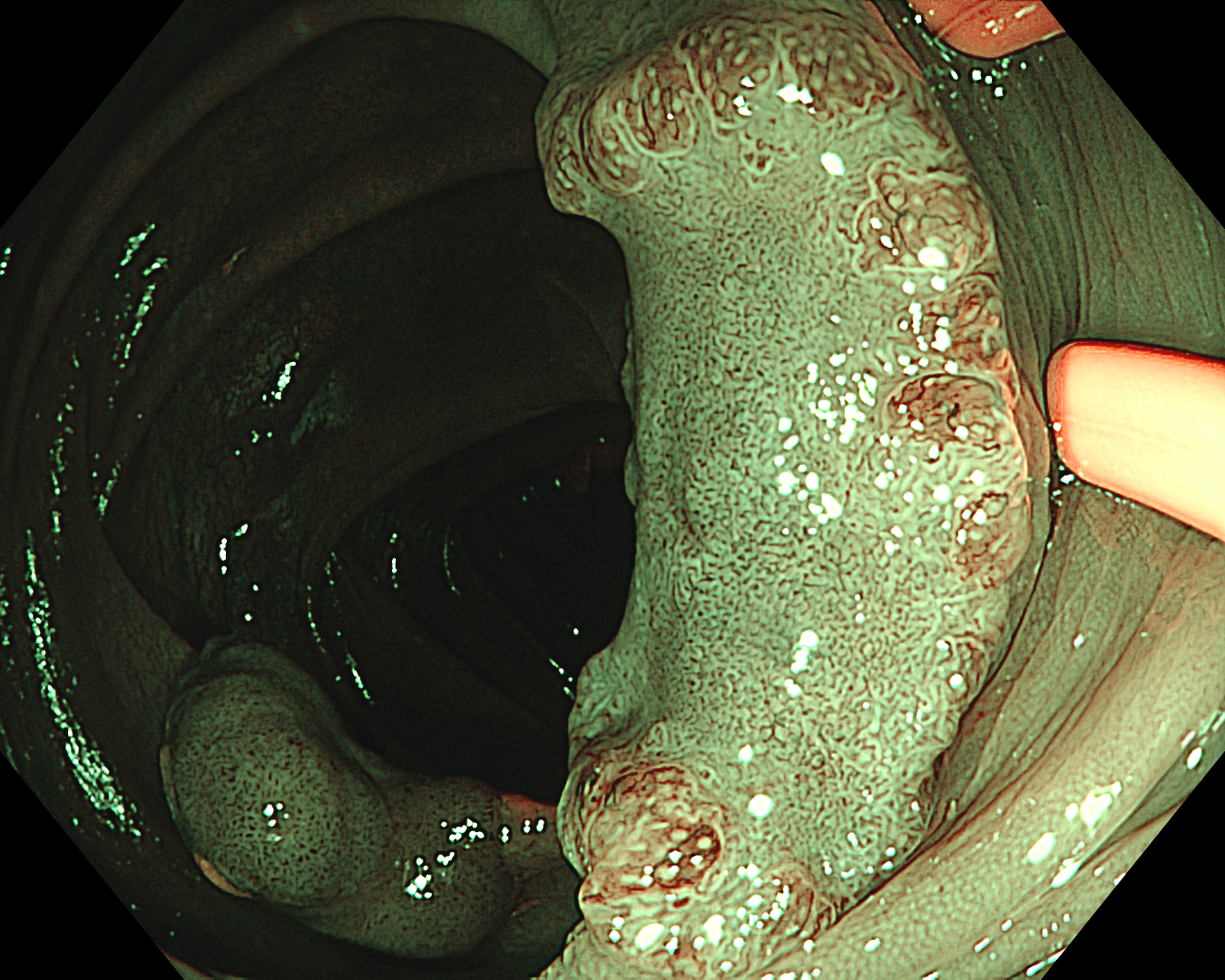
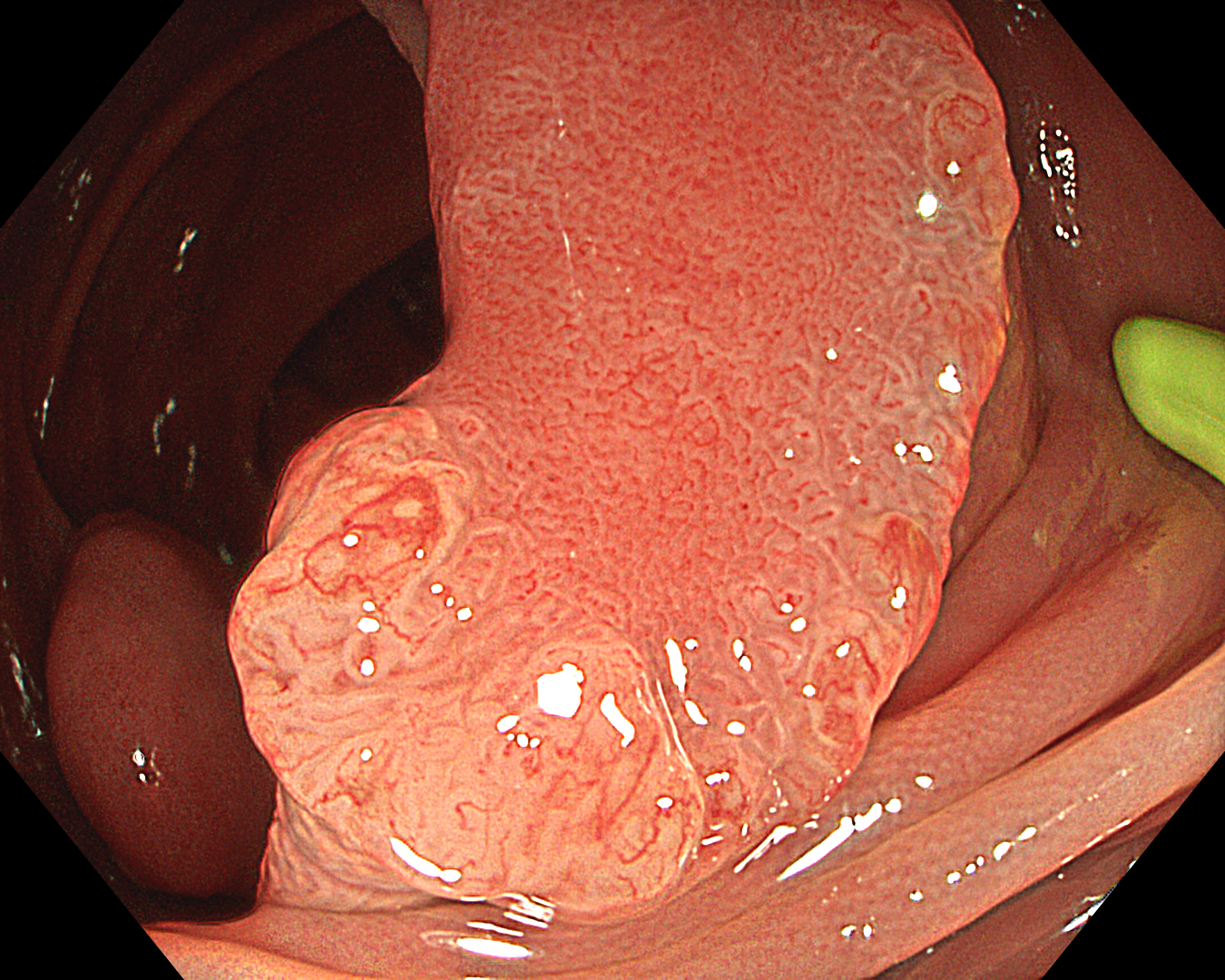
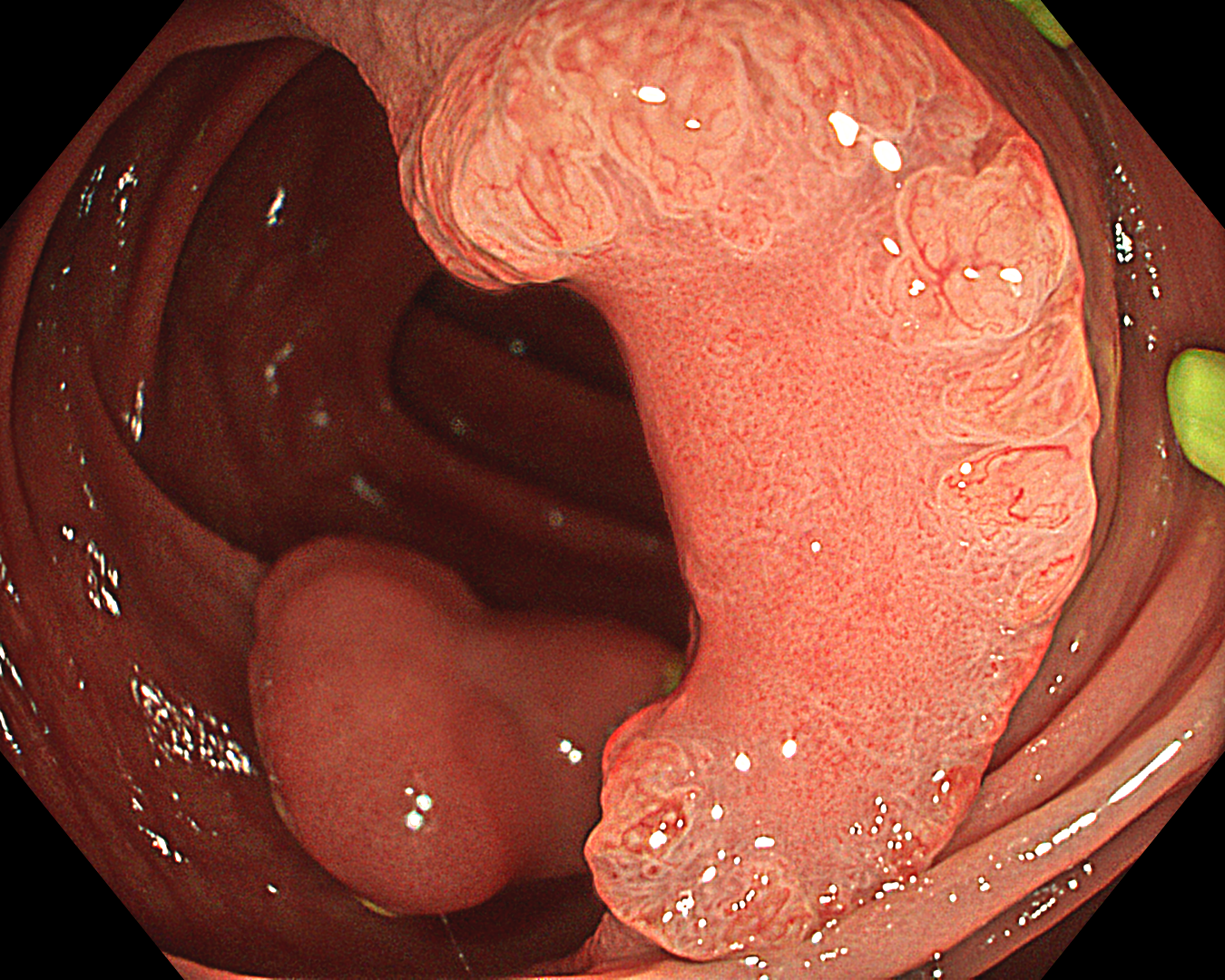
1. WLI Observation
Enhancement: A8
WLI mode
TXI Mode: None
RDI Mode: None
BAI-MAC: On
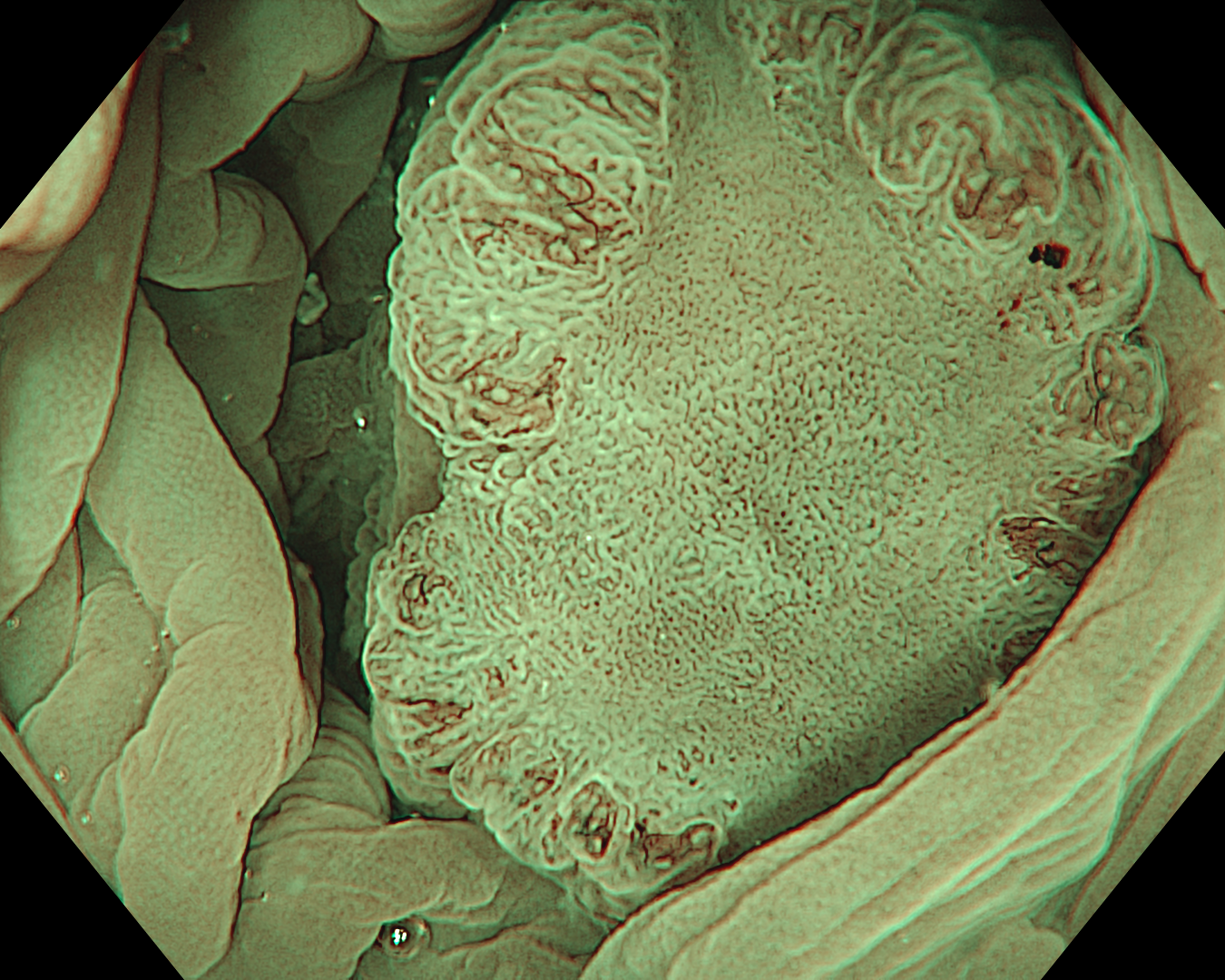
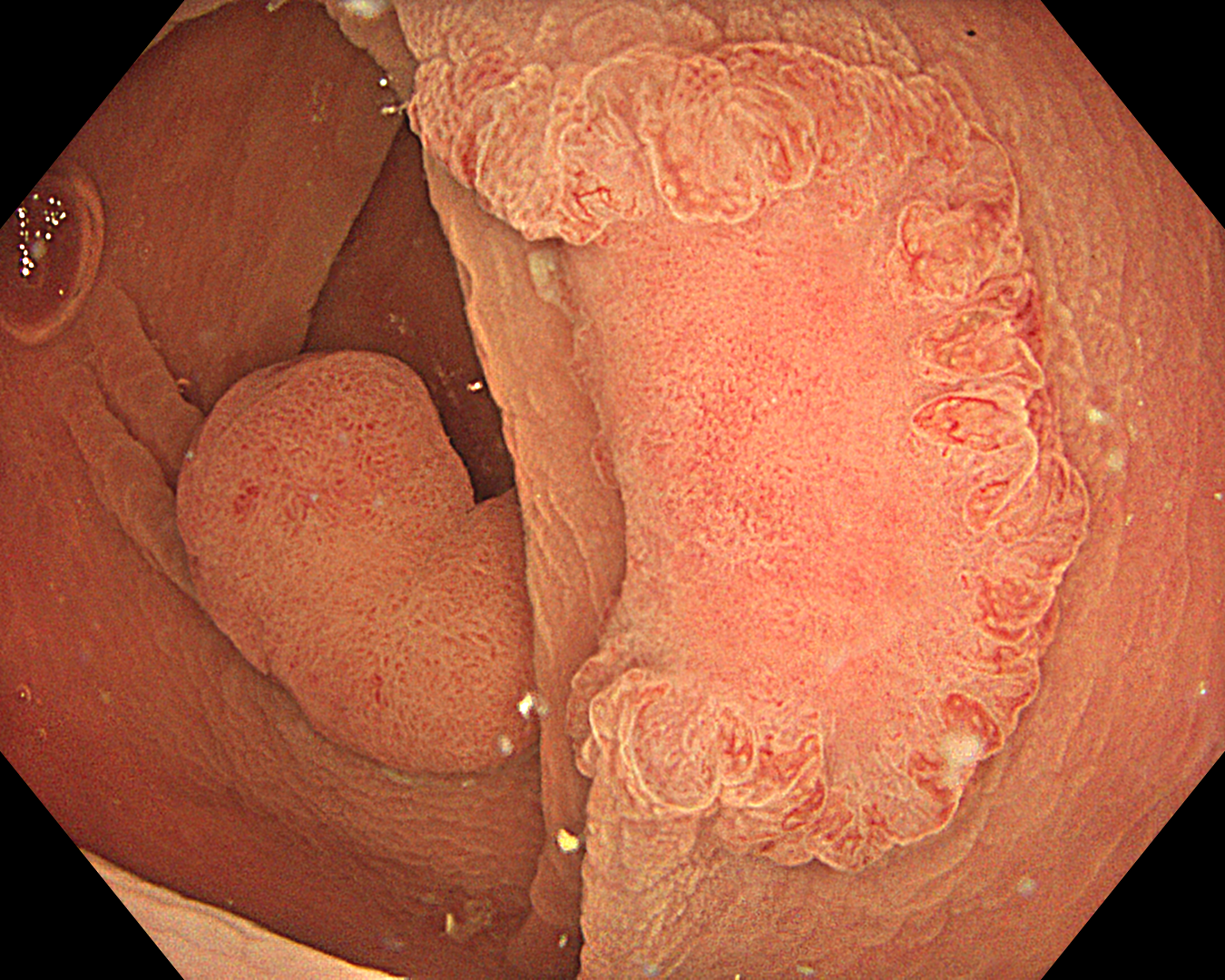
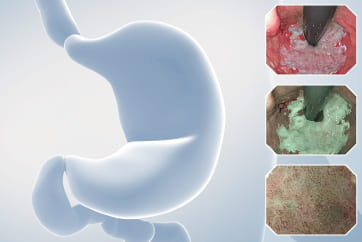
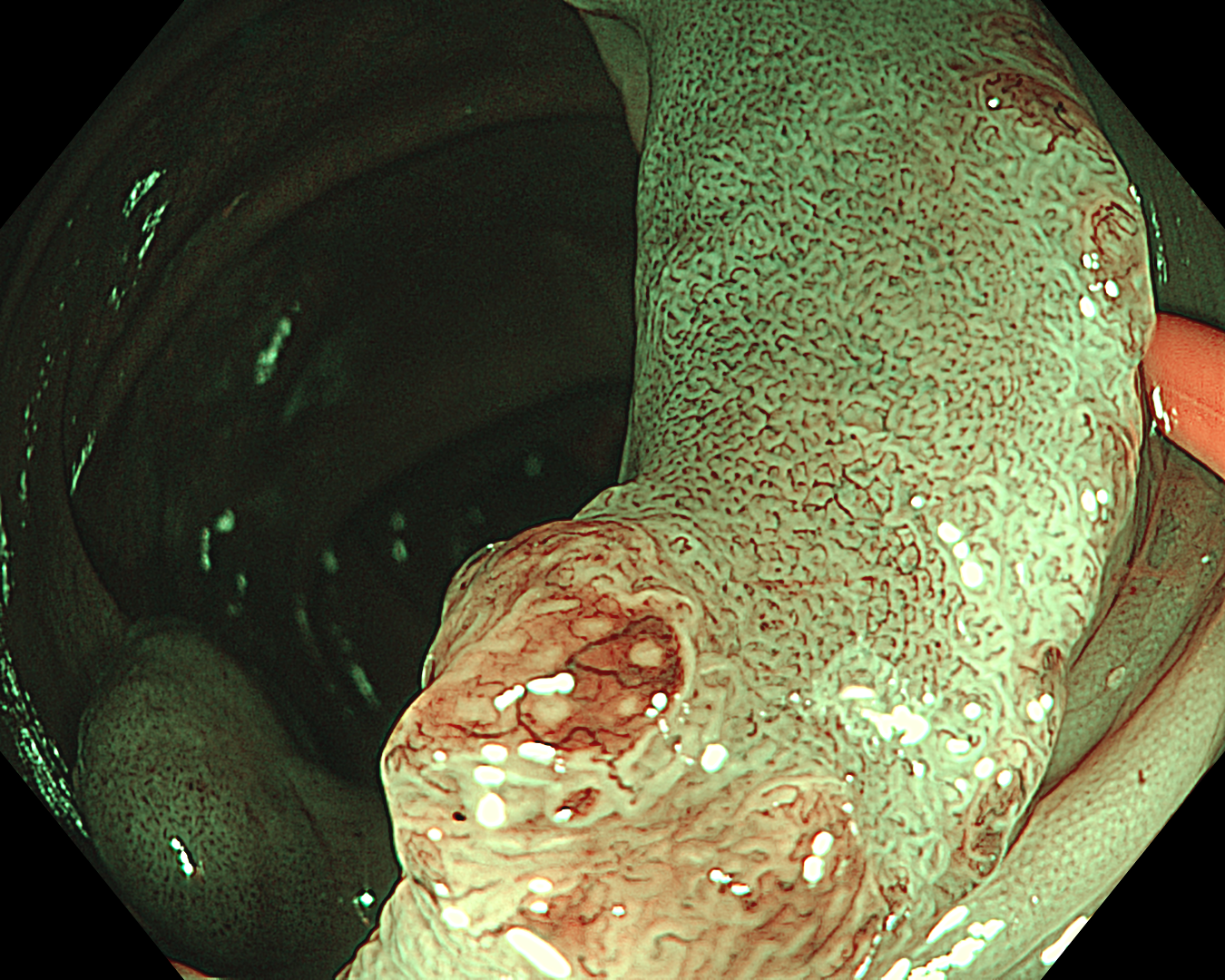
2. NBI™ technology Observation
Enhancement: B8
NBI mode
TXI Mode: None
RDI Mode: None
BAI-MAC: None
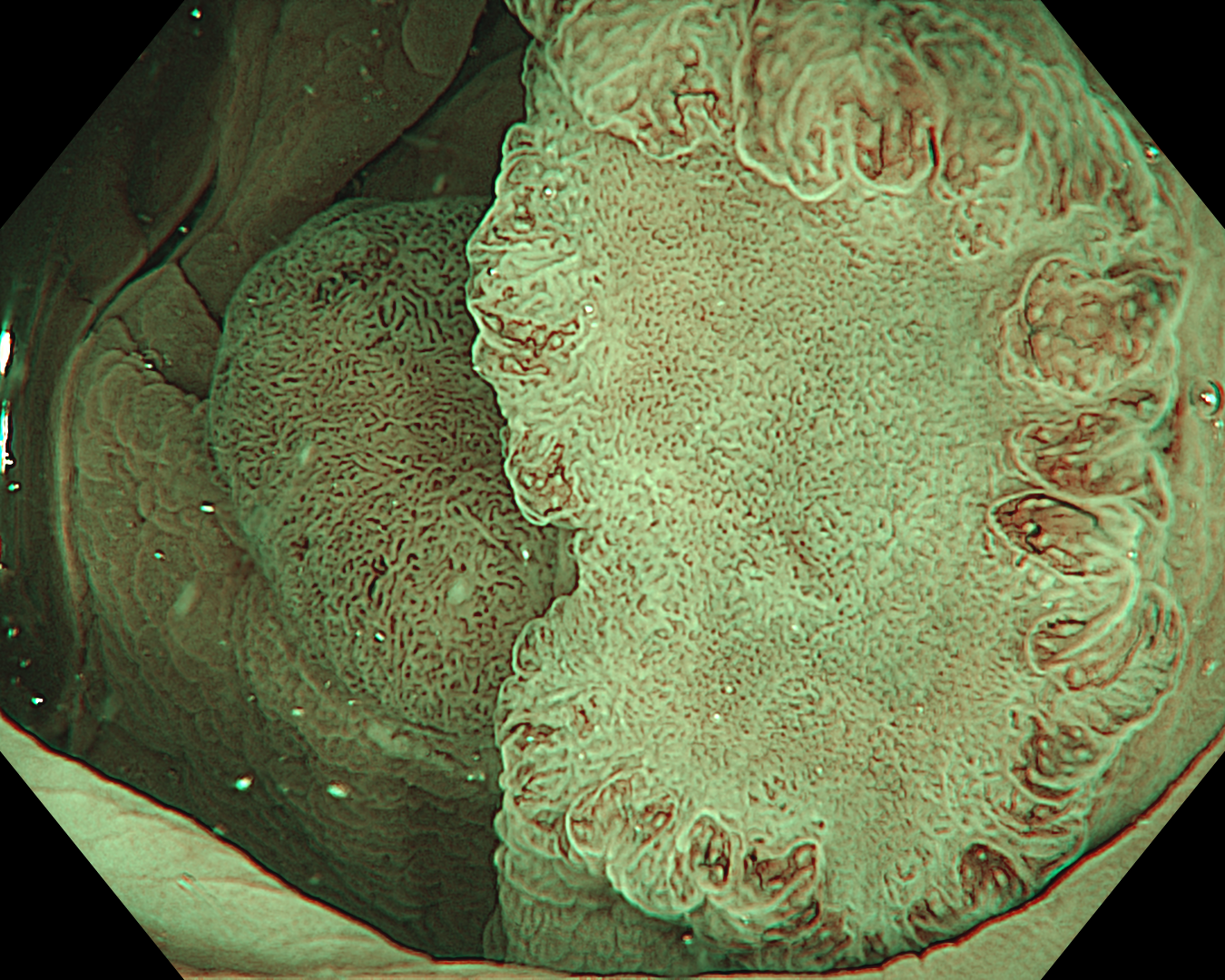
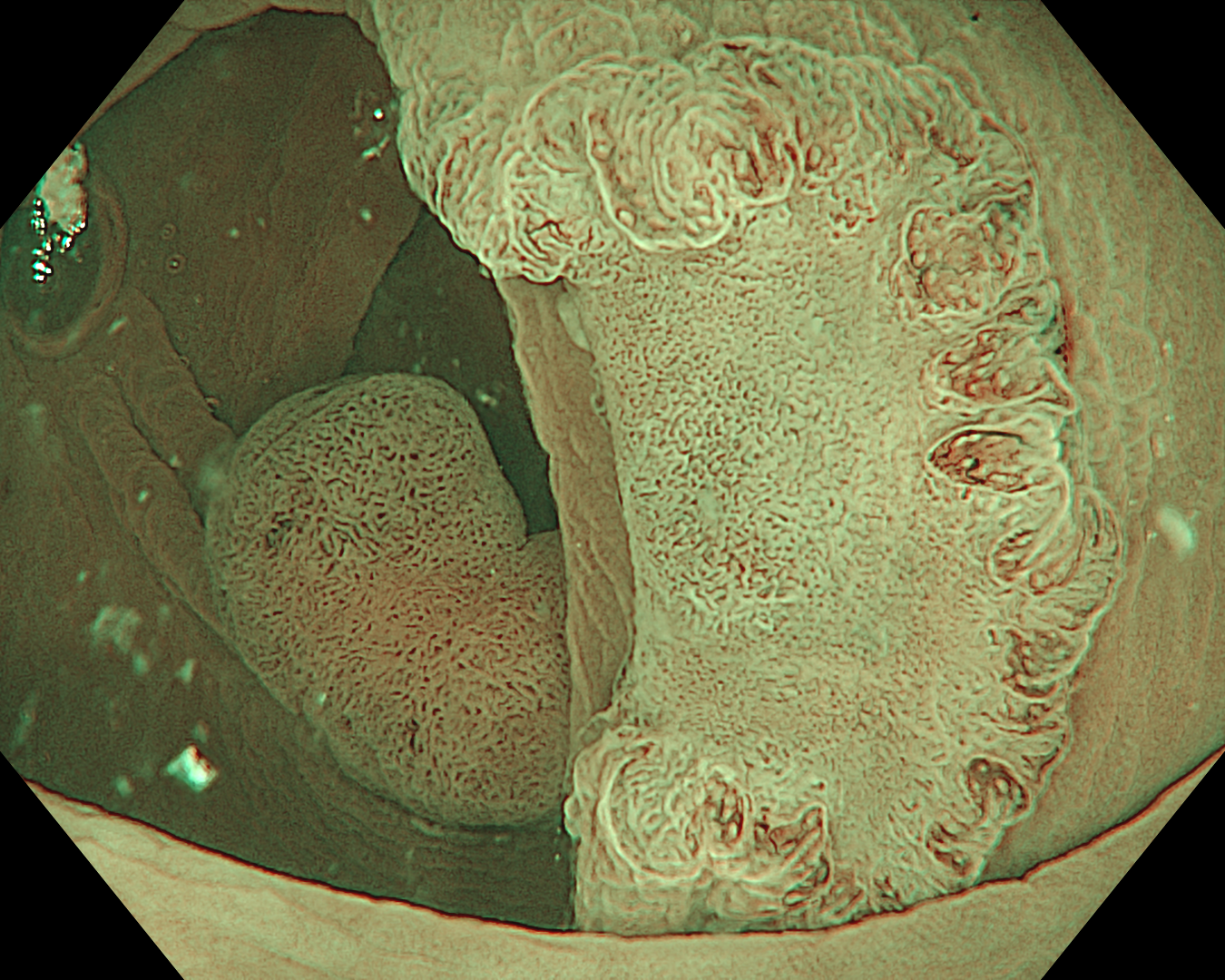
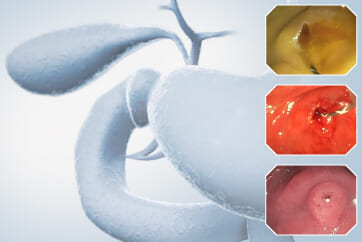
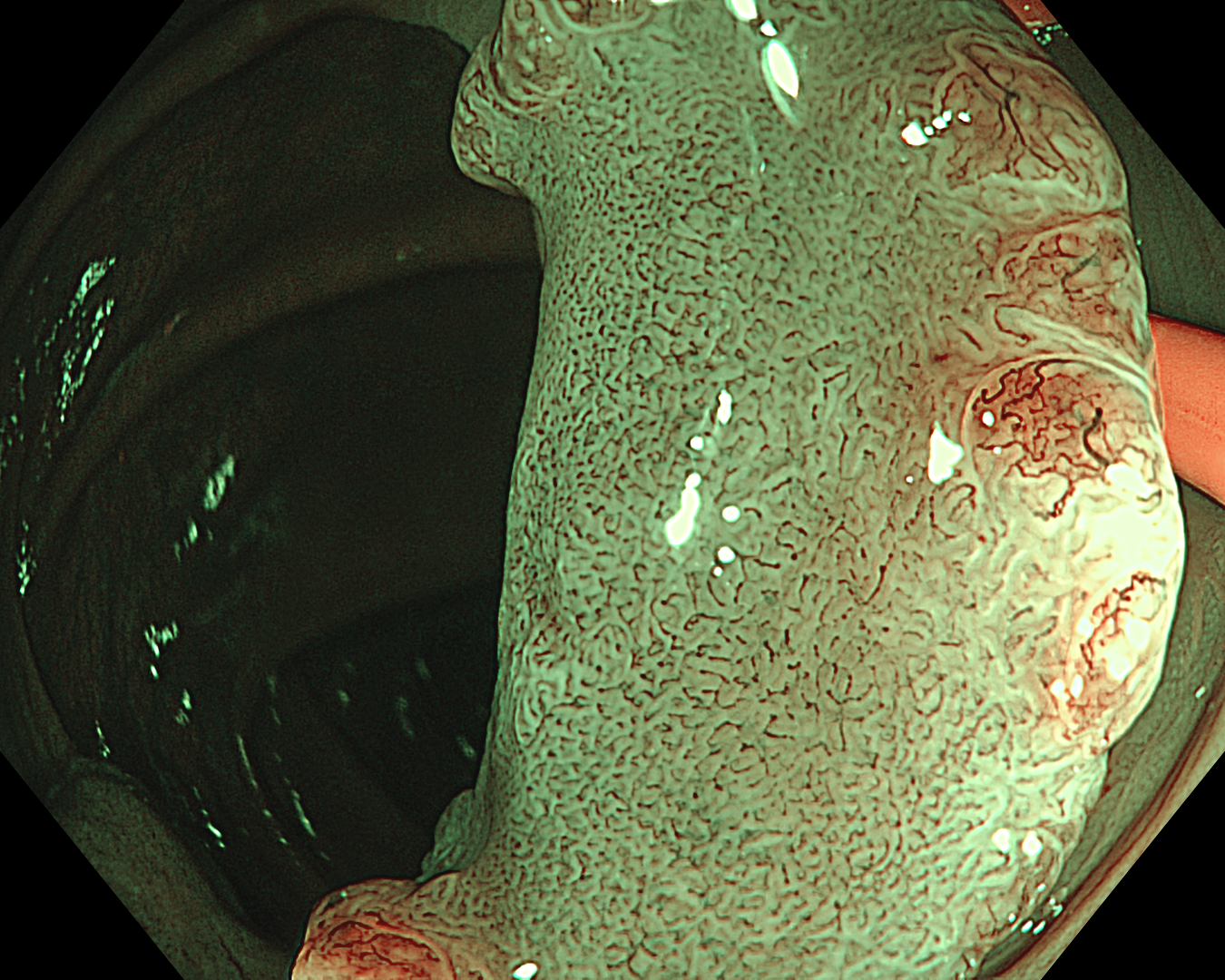
3. Near Focus mode with NBI™ technology
Enhancement: B8
NBI mode
TXI Mode: None
RDI Mode: None
BAI-MAC: None
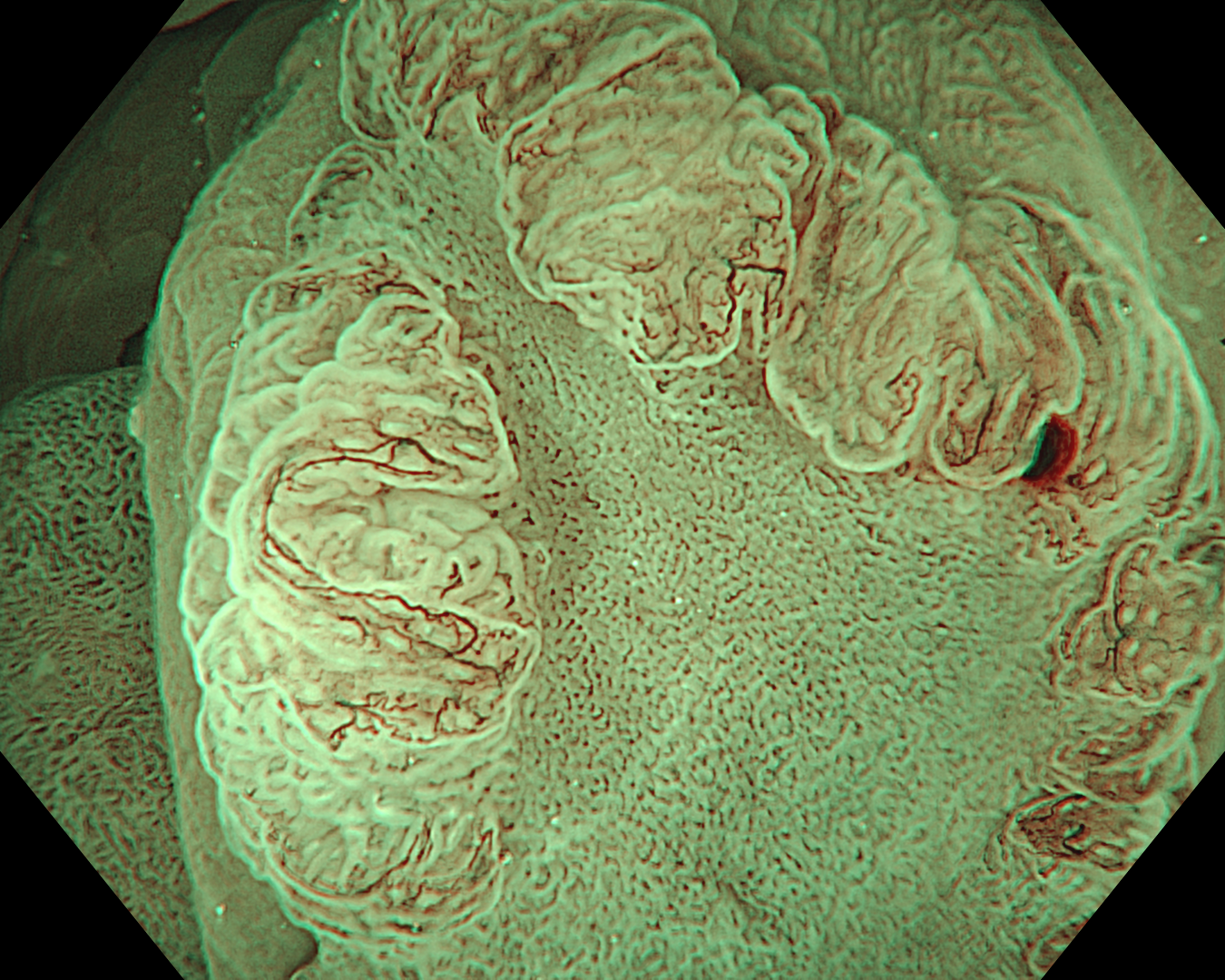
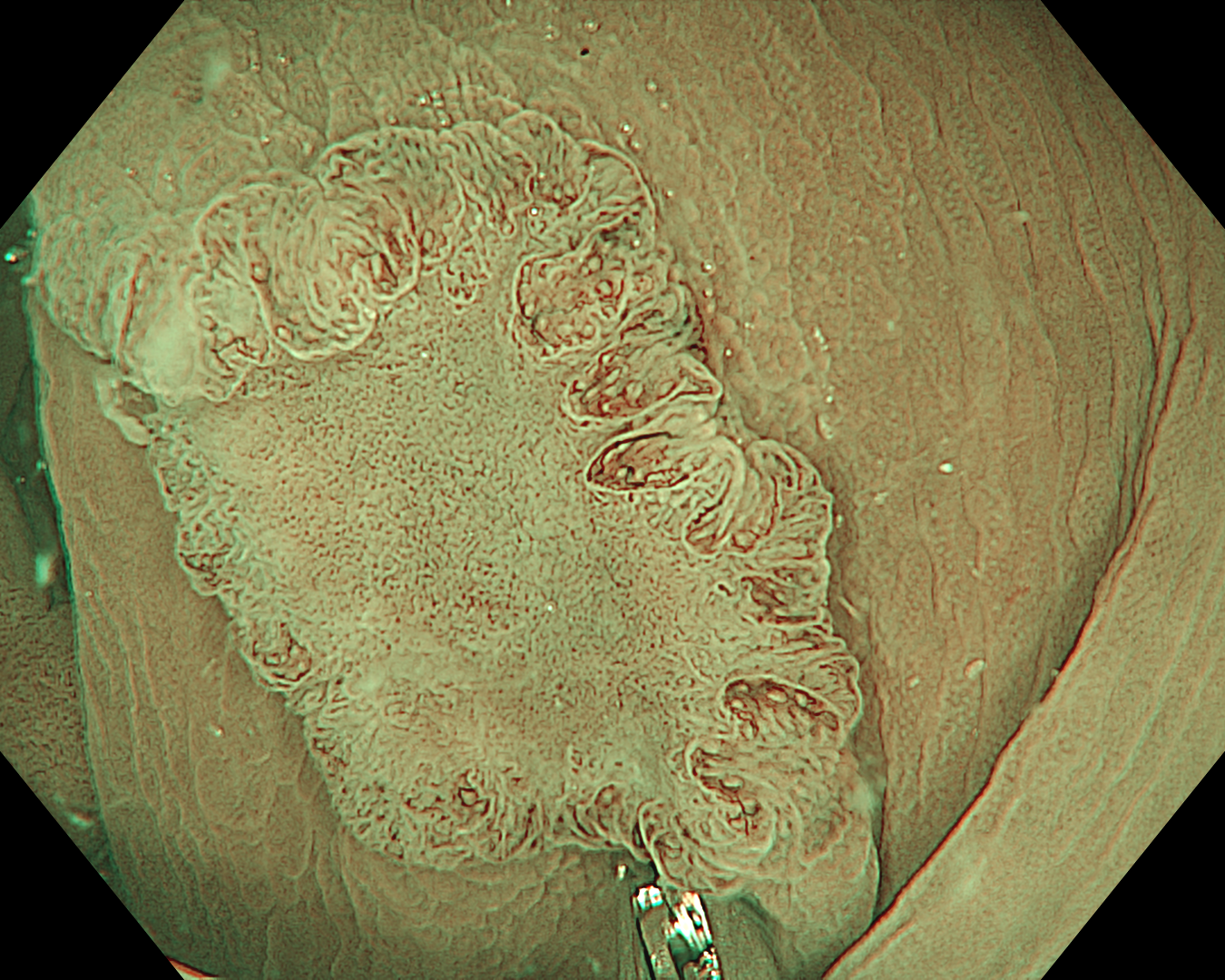
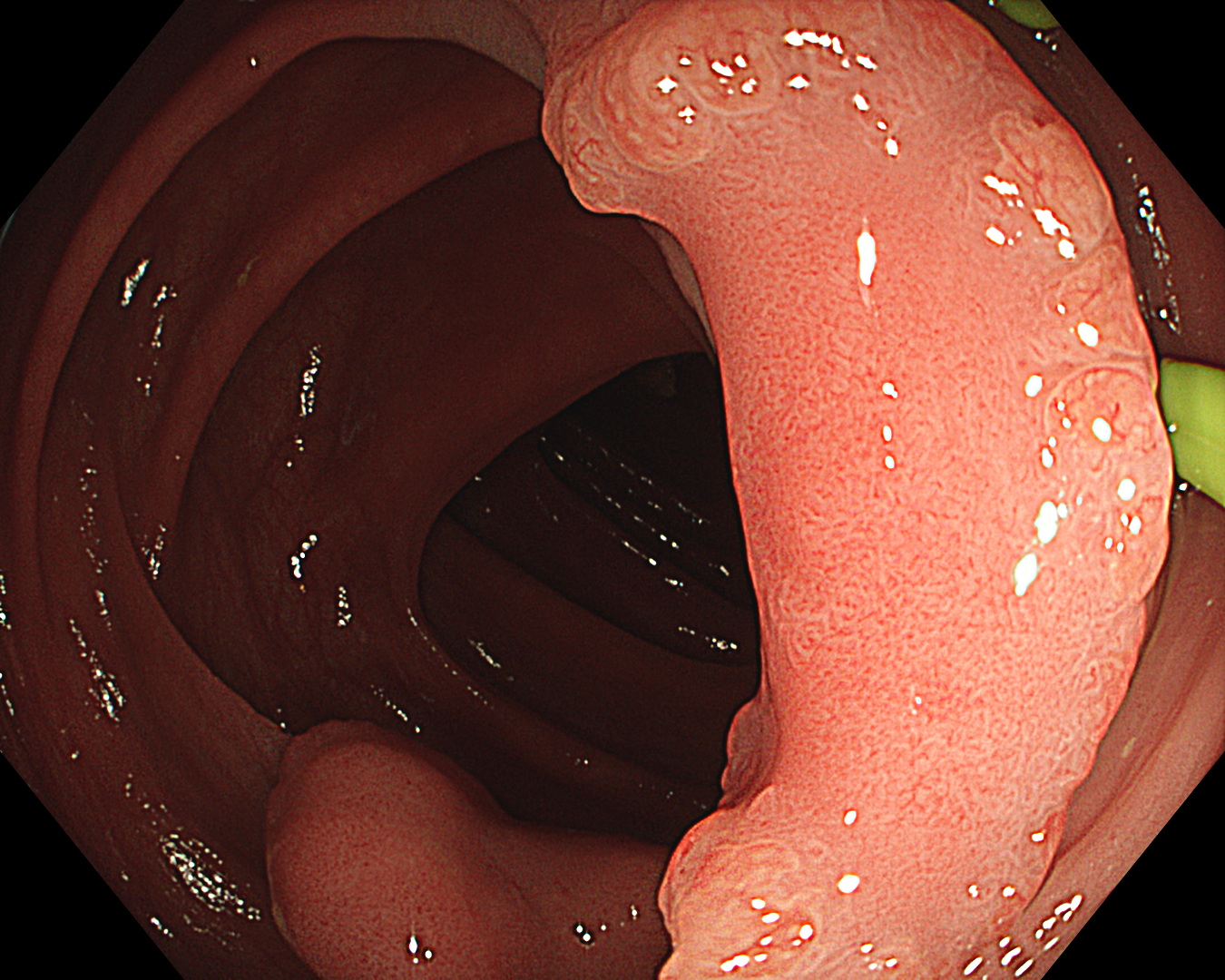
4. Near Focus mode with NBI™ technology
Enhancement: B8
NBI mode
TXI Mode: None
RDI Mode: None
BAI-MAC: None
6. TXI™ technology mode 2
TXI Mode: 2
7. TXI™ technology mode + Near Focus mode
TXI Mode: 2
8. TXI™ technology mode + Near Focus mode
TXI Mode: 2
Case Video
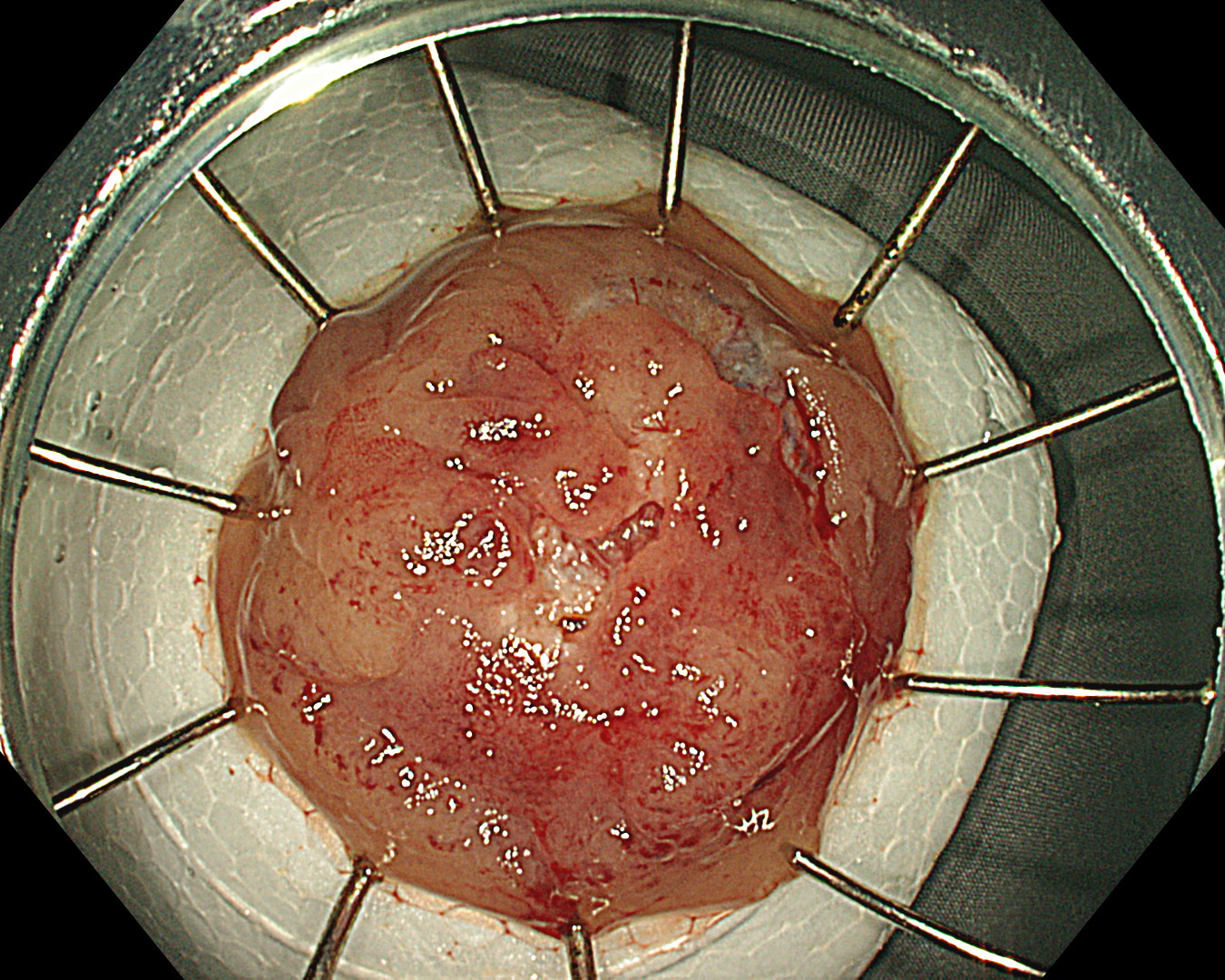
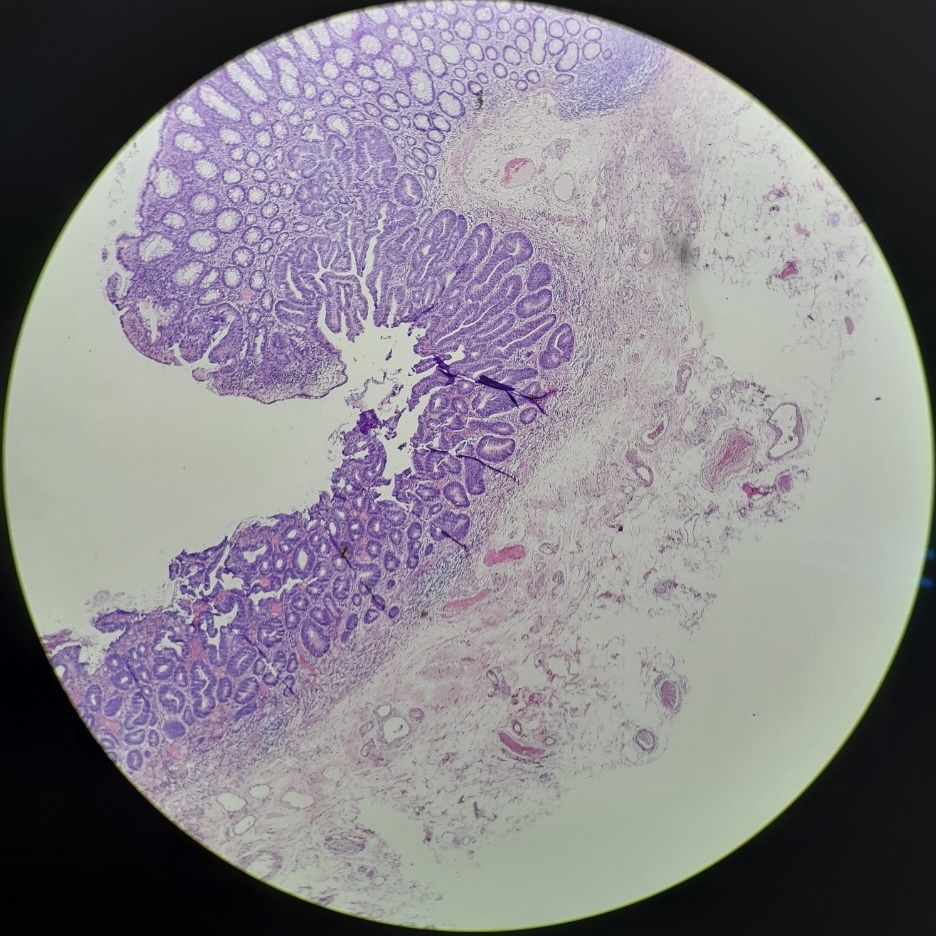
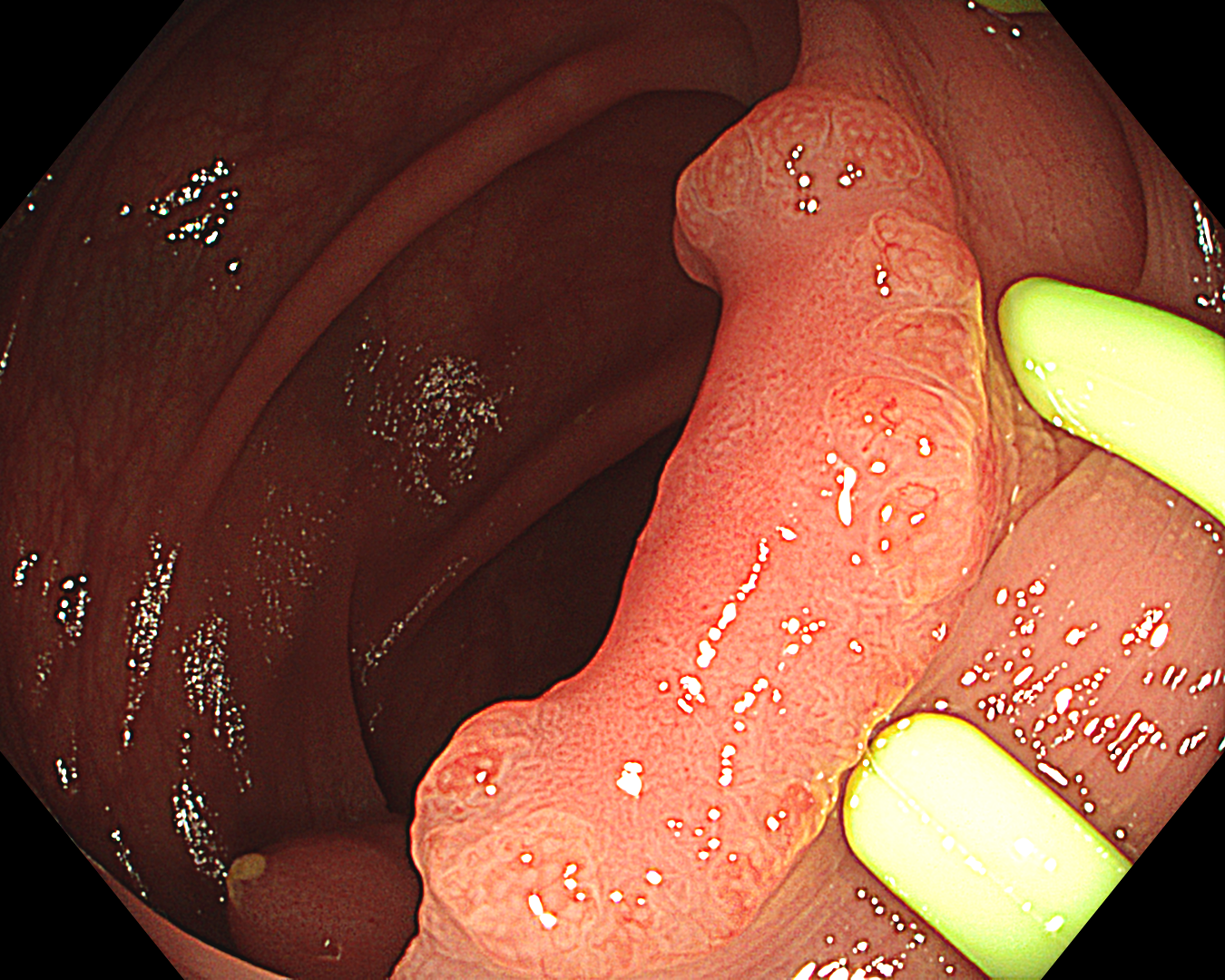
LST PD
This was an LST-NG-PD-type mucosal cancer in the transverse colon. By using image enhancement modes (WLI, TXI™, and NBI™ technologies) with or without near mode), surface and vessel abnormalities of the lesion are clearly observed, making an important contribution to the assessment and classification of the lesion. Underwater observation, visualization of the entire lesion is easy, while assessment of surface pattern and vessel pattern of the lesion is still very clear.
Overall Comment
Laterally spreading tumors (LSTs) were originally classified into four subtypes by Shin-ei Kudo et al., including LST-G (granular type) and LST-NG (non-granular type). LST-G is subclassified into homogeneous (LST-G-H) and nodular mixed types (LST-G-M), and LST-NG is divided into flat elevated (LST-NG-F) and pseudo-depressed types (LST-NG-PD).
LST-G types tend to have less submucosal carcinoma, irrespective of the size of the lesion. However, the LST-NG types tend to be more aggressive, with a higher incidence of advanced carcinoma, especially the pseudo-depressed type.
Different classifications help predict the risk of submucosal invasion, such as the NICE classification and the JNET classification. Its subclass JNET2a is mostly comprised of intraepithelial lesions; JNET3 is composed mainly of deep submucosal invasive lesions; and JNET2b can be found in both intramucosal and submucosal invasive lesions.
When a part of the polyp is hidden behind a fold or clamshell wrapped around a fold, endoscopists encounter challenges in visualizing the entire surface area of the polyp. Underwater observation could help solve this issue.
This is a LST-NG-PD with a 16-mm diameter. The lesion has a red O-ring with a depressed area about 14mm in diameter. In “air” endoscopy and underwater endoscopy, the lesion has a “non-extension” or “sclerosis of the wall” sign. Observing in the “near focus”, some areas had JNET type 2b, suggesting that this is either an intramucosal cancer lesion or a cancer lesion with submucosal invasion.
We resected the lesion by FTRD (Full-Thickness Resection Device) due to failure to resect the lesion by ESD.
* Specifications, design and accessories are subject to change without any notice or obligation on the part of the manufacturer
Dr. Serhii Polishchuk Case 20: 0-Is (LST-mixed type), 22mm, JNET 2A with fern-like pits
Prof. Yasushi Sano
- Content Type