Pancreatobiliary case 4

Dr. Masafumi Mizuide
Department of Gastroenterology, Saitama Medical University International Medical Center, Japan
Introduction
The new Olympus endoscopy system EVIS X1™ includes features such as TXI (Texture and Color Enhancement Imaging) and RDI (Red Dichromatic Imaging), which are expected to improve endoscopic images. RDI is a unique image enhancement technology using narrow-band light of red, amber, and green, and its usefulness during ESD procedures has already been reported.
However, the evaluation of EVIS X1 in the field of pancreatobiliary endoscopy is currently insufficient. Therefore, we examined the potential of EVIS X1 in the field of pancreatobiliary endoscopy at our hospital. This report focuses on the usefulness of TXI in improving the visibility for the orifice of major duodenal papilla.
EVIS X1/ TXI
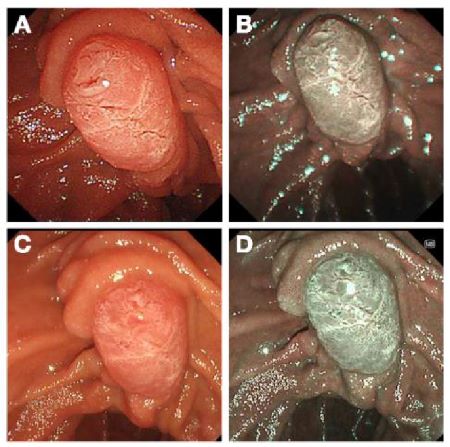
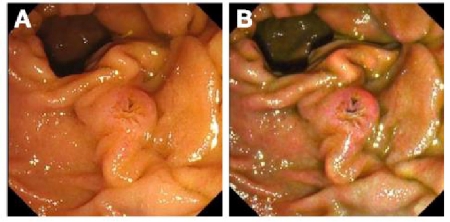
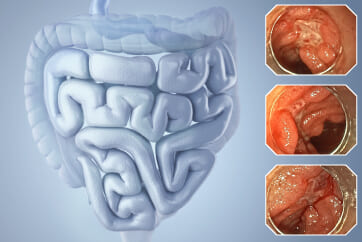
First, we present images of the same case with adenoma of major duodenal papilla observed using the light source devices EVIS LUCERA ELITE™ and EVIS X1™ (Figure 1).
The EVIS X1 is equipped with five LEDs, covering the wavelength range of light provided by the xenon light source EVIS LUCERA ELITE, resulting in enhanced white light contrast and excellent color reproduction. With the new Pre-freeze function, the halation is reduced and clear images can be selected. With the new noise reduction function, the noise is reduced (especially in dark areas), as a result, the images are clearer than those from the EVIS LUCERA ELITE (Figure 1 A/B) as shown in (Figure 1 C/D).
The TXI feature of EVIS X1 is an image processing function focusing on three elements that impact screening: 1) structure, 2) brightness, and 3) color tone. It decomposes the input information from white light into “texture images” and “brightness components,” optimizes each through image processing technology, and then integrates them (TXI Mode 2). Furthermore, by adding color enhancement (TXI Mode 1), images are brightened without halation, structural changes in mucosal morphology and subtle color changes become easier to recognize. As a result, TXI can support the early detection of lesions.
There are two modes of TXI: Mode 2, which provides a color close to white light without emphasizing “color tone” (Figure 1 E), and Mode 1, which emphasizes “color tone,” making bright reds, blues, and yellows stand out (Figure 1 F). In Mode 1, the gastrointestinal mucosa appears bluish-white. Initially, some users may experience eye strain with Mode 1, so switching to Mode 2, which is closer to white light, can also be an option.
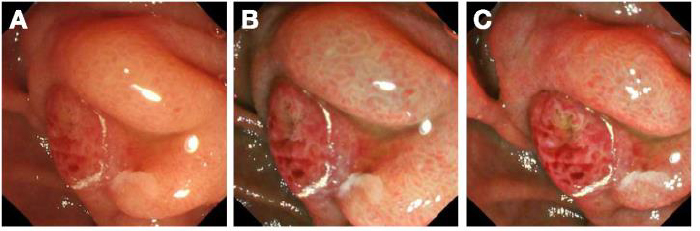
[Fig. 1] "Same Case with Adenoma of Major Duodenal Papilla: Image with two Light Sources"
A/B. Image with white light/NBI using EVIS LUCERA ELITE
C/D. Image with white light/NBI using EVIS X1: Compared to A/B, the images are clearer, and overall brightness in the field of view is improved
E. TXI Mode 2 Image: Colors close to white light, and the irregular structure of the mucosal surface is clarified
F. TXI Mode 1 Image: In addition to clarification of mucosa surface irregularities, reddish and white areas are clarified
Improving visibility for the orifice of major duodenal papilla using TXI
In our facility, we focused on the characteristics of TXI, specifically “structure enhancement” and “color enhancement.” We anticipated that “structure enhancement” would clarify the mucosal structure of the major duodenal papilla, (hereafter referred to as “major papilla”) especially its surface irregularities, and that “color enhancement” would improve recognition of bile flow from the orifice of major papilla. Based on these expectations, we considered that TXI could be beneficial for improving the visibility for the orifice of major papilla.
To evaluate the effectiveness of TXI in improving visibility for the orifice of major papilla, we observed the major papilla in untreated cases using two methods: 1) Image using white light with TJF-Q290V. 2) Image using TXI (Mode 1), comparing visibility for the orifice of major papilla between TXI and white light.
Regarding visibility for the orifice of major papilla, we conducted a survey for the orifice of major papilla in twenty untreated cases, involving four resident trainees (hereinafter referred to as “trainees”) and four expert endoscopists at our institution. They were asked to choose from “decreased,” “equivalent,” or “improved” visibility for the orifice of major papilla compared to white light. Furthermore, they were asked to assess the morphology of the major papilla using the Inomata classification under both white light and TXI.
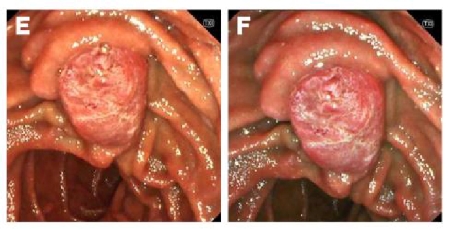
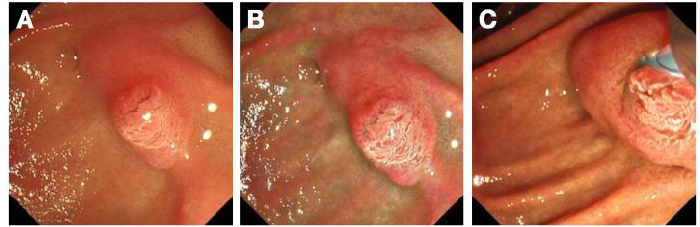
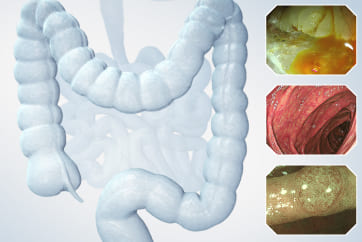
The survey results regarding TXI visibility were as follows: Trainees: “Decreased: 0%,” “Equal: 41.2%,” “Improved: 58.8%”, and expert endoscopists: “Decreased: 0%,” “Equal: 36.2%,” “Improved: 63.8%” As anticipated, in many cases, the mucosal structure of the major papilla, particularly the surface irregularities, appeared more clearer, leading to improved visibility for the orifice of major papilla (Figure 2). In TXI Mode 1, the orifice of major papilla is observed as a “hole-like” structure, making it easier to recognize (Figure 2B). In TXI Mode 1 with added “color enhancement,” the capability for recognition of bile flow also increases (Figure 3B/D), leading to further improvement in the visibility for the orifice of major papilla.
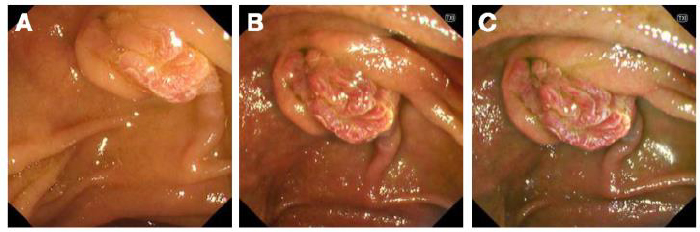
[Fig. 2] "Improved Visibility for the Orifice of Major Papilla with TXI: Septal Type (Tatenaga Type)"
A. Image with white light of a septal type (Tatenaga type): A slight depression that appears to be the orifice is visible on the oral side
B. Image with TXI Mode 1 of the same case: Irregularities in the structure are clarified, and the orifice is distinctly recognized as a black "hole-like" structure
[Fig. 3] "Improved Recognition of Bile Flow with TXI Mode 1"
A. Image with white light: The overall brightness in the distant view is reduced, making it difficult to recognize bile flow
B. Image with TXI Mode 1 of the same case: Bile flow becomes clear due to color enhancement and brightness adjustment
C. Image with white light in case of biliary sludge: the recognition of biliary sludge is possible even with white light
D. Image with TXI Mode 1 in the same case: Yellow enhancement and suppression of mucosal color tones result in clearer visibility for biliary sludge
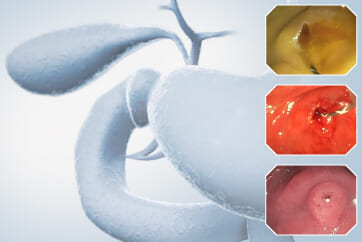
The contribution of TXI in ERCP cannulation
We investigated the visibility for the orifice of major papilla with TXI, using category by the Inomata classification.
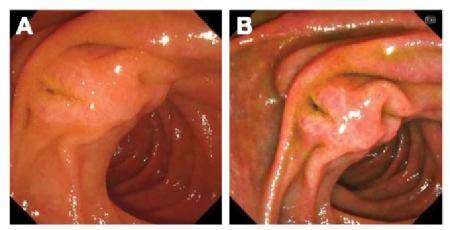
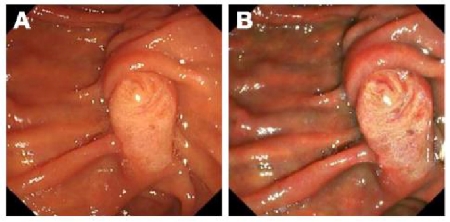
In separate type (including Betsukaiko type; comprising two separate, isolated orifices. Tamanegi type; comprising gyrate, separate onion ducts.), both trainees and expert endoscopists noted improved visibility with TXI in nearly all cases. In the survey of 20 cases, there were 3 cases of Betsukaiko type (Figure 4/5) and 1 case of Tamanegi type (Figure 6). Among trainees, the recognition rate of the major papilla morphology with white light was 37.5%, which improved to 87.5% with TXI. Similarly, among expert endoscopists, the recognition rate with white light was 68.8%, which improved to 100% with TXI (Figure 4 B, Figure 5 B/C, Figure 6 B). In cases with separate types, the recognition of the orifice directly impacts the success of cannulation. Therefore, improving the visibility for the orifice with TXI can enhance the success rate of cannulation. Especially among less experienced beginners, TXI may contribute to an increased success rate in cannulation.
Even in Septal type (including Kesetsu type; comprising nodular changes on the oral side of center. Tatenaga type; comprising longitudinal grooves continuous with the orifice. Jyumo Type; comprising villous papilla. Heitan Type; comprising unstructured without a clear orifice.), Visibility with TXI is improved in many cases. In Kesetsu type, the nodular areas become clearer with TXI. Recognizing nodular areas with TXI enables to perform cannulation conceiving techniques such as pushing nodule into bile duct. In Tatenaga type, the slit becomes more clearer, and the orifice of major papilla is emphasized as a black “hole-like” structure with TXI, making it easier to identify the point for addressing the contrast catheter (Figure 2B).
On the other hand, in Jyumo type or Heitan type, there were often “equivalent” in TXI visibility among both trainees and expert endoscopists. This suggests that the contribution of TXI in ERCP cannulation may vary depending on the morphology of the major papilla.
[Fig. 4] "Improved Visibility of the Pancreatic Duct orifice with TXI Mode 1: Separate Type (Betsukaiko Type)"
A. Image with white light of a separate type (Betsukaiko type): The pancreatic duct orifice is not clearly discernible, making it difficult to understand it as a separate type
B. Image with TXI Mode 1 of the same case: The visibility of the pancreatic duct orifice improves, making it clear that it is a separate type
[Fig. 5] "Improved Visibility for the Bile Duct orifice with TXI Mode 1: Separate Type (Betsukaiko Type)"
A. Image with white light of a separate type (Betsukaiko type): The bile duct orifice cannot be recognized
B. Image with TXI Mode 1 of the same case: Thebile duct orifice is visible
C. Image with TXI Mode 2 of the same case: Cannulation for the bile duct orifice
[Fig. 6] "Improved Visibility of the Bile Duct orifice with TXI Mode 1: Separate Type (Tamanegi Type) (Video)"
A. Image with white light of a separate type (Tamanagi type): It can be identified as onion-shaped, but recognizing the central part of the onion shape is difficult
B. Image with TXI Mode 1 of the same case: The structure becomes clearer, allowing recognition of the central part of the onion shape. Using TXI can perform that the tip of contrast catheter is addressed on bile duct orifice surely.
Other contributions from TXI
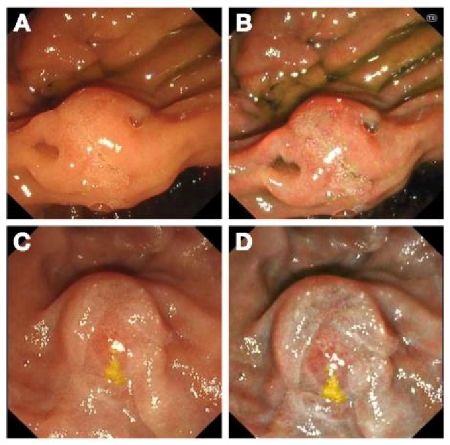
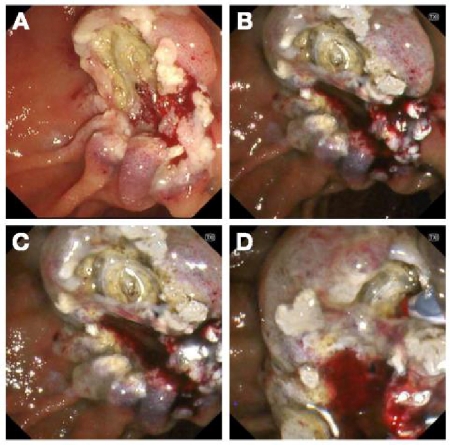
There are other situations where TXI is considered beneficial. In endoscopic papillectomy (EP), pancreatic duct stenting is required for prevention of pancreatitis. Cannulation of the pancreatic duct is essential, but TXI remains useful even after EP (Figure 7). Immediately after resection, under white light image, the resected area appears flat, making it difficult to easily identify the pancreatic duct orifice (Figure 7A). With TXI, the concave pancreatic duct orifice becomes clear, enabling rapid cannulation for the pancreatic duct (Figure 7 B/C/D). If the view of the major papilla is difficult due to malignant tumors (Figure 8), using TXI Mode 1 makes it easier to recognize the concave orifice of the major papilla, which involves bile flow, and proves useful for cannulation (Figures 8 B/C). For beginners, even after EST, Image of the major papilla becomes easier for determining the bile duct orifice (Figure 9). Even in situations requiring treatment of the minor papilla, TXI can be expected to assist in identifying the orifice of the minor papilla.
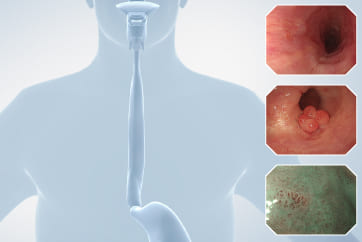
[Fig. 7] "Improved visibility of the pancreatic duct orifice with TXI Mode 1: Immediately after endoscopic papillectomy"
A. White light Image immediately after papillectomy: It is difficult to identify the pancreatic duct orifice
B. TXI Mode 1 Image immediately after papillectomy: Structural enhancement makes the concave pancreatic duct orifice clear
C. TXI Mode 1 Image immediately after papillectomy: Close-up view
D. TXI Mode 1 Image immediately after papillectomy: Cannulation while confirming the pancreatic duct orifice
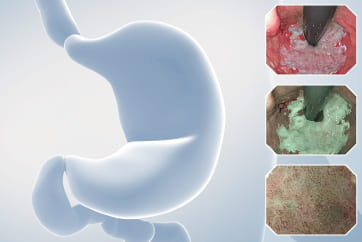
[Fig. 8] "Improved visibility for the orifice of major papilla with TXI: Cases with difficult view"
A. White light Image in case with difficult view: Major papilla is observed tangentially, making it difficult to easily identify the orifice
B. TXI Mode 1 Image in the same case: The concave area becomes clear, allowing recognition of the orifice
C. TXI Mode 1 Image in the same case: With added recognition of bile, the orifice becomes clearly visible
[Fig. 9] "Improved visibility of the bile duct orifice with TXI Mode 1: Post-EST papilla"
A. White light Image of the post-EST papilla: The bile duct orifice is located on the oral side
B. TXI Mode 2 Image in the same case: Although similar in color to white light, surface irregularities become clear, improving visibility of the bile duct orifice
C. TXI Mode 1 Image in the same case: Clarity of surface irregularities, coupled with recognition of bile flow, enhances visibility of the bile duct orifice
Conclusion
In this report, we focused on the utility of TXI in the field of pancreatobiliary endoscopy, particularly discussing the potential of EVIS X1. Cannulation of the bile duct and pancreatic duct during ERCP requires careful consideration of the morphology of the major papilla and the confluence pattern of the pancreaticobiliary ducts. Image of the major papilla with TXI can improve visibility of the orifice and aid in understanding the morphology of the major papilla, potentially contributing to increased success rates of cannulation in the target area. In the future, we hope that with accumulated cases, the effectiveness of TXI will become more evident .
* Specifications, design and accessories are subject to change without any notice or obligation on the part of the manufacturer
Jong Ho Moon, MD, PhD, FASGE, FACG, FJGES
Il Sang Shin, MD, PhD Cases 5: Bile Duct Orifice observation and Duodenal Papilla Tumors treatment
Dr. Haruka Toyonaga
- Keyword
- Content Type