Author

Dr. Yuko Kitagawa, Professor, Department of Surgery, School of Medicine, Keio University
Biography
Graduated from Department of Surgery, School of Medicine, Keio University in 1986. Studied at the University of British Columbia in Canada for about three years from August 1993. Upon returning to Japan, worked at Keio University and became a professor at the Department of Surgery, School of Medicine, Keio University in April 2007. Became Director of Keio University Hospital and a board member of Keio University in August 2017. The specialization is the minimally invasive surgical treatment and multidisciplinary treatment of esophageal carcinoma and gastric cancer.
Introduction
Sentinel node (SN) theory is the concept that the first lymph node metastasis occurs in the SN, which is defined as the lymph node that receives lymph flow directly from a tumor. For breast cancer and malignant melanomas, personalized surgery according to each patient is conducted as the standard treatment. To examine possible clinical applications of SN theory in gastric cancer, a multicenter study was conducted by an sentinel node navigation surgery (SNNS) study group of patients with cT1N0-cT2N0 gastric cancer1). The number of SNs detected was 5.4 on average and the identification rate was 97.8% (456/466). Metastasis detection sensitivity in SN was 94.0% (63/67); negative predictive value, 98.9% (389/393); and diagnostic accuracy, 99.1% (452/456). The results of this clinical study showed that safer selective sentinel lymphadenectomy was possible also in SN metastasis-negative patients by resecting not only the SN, but also the lymphatic basin.
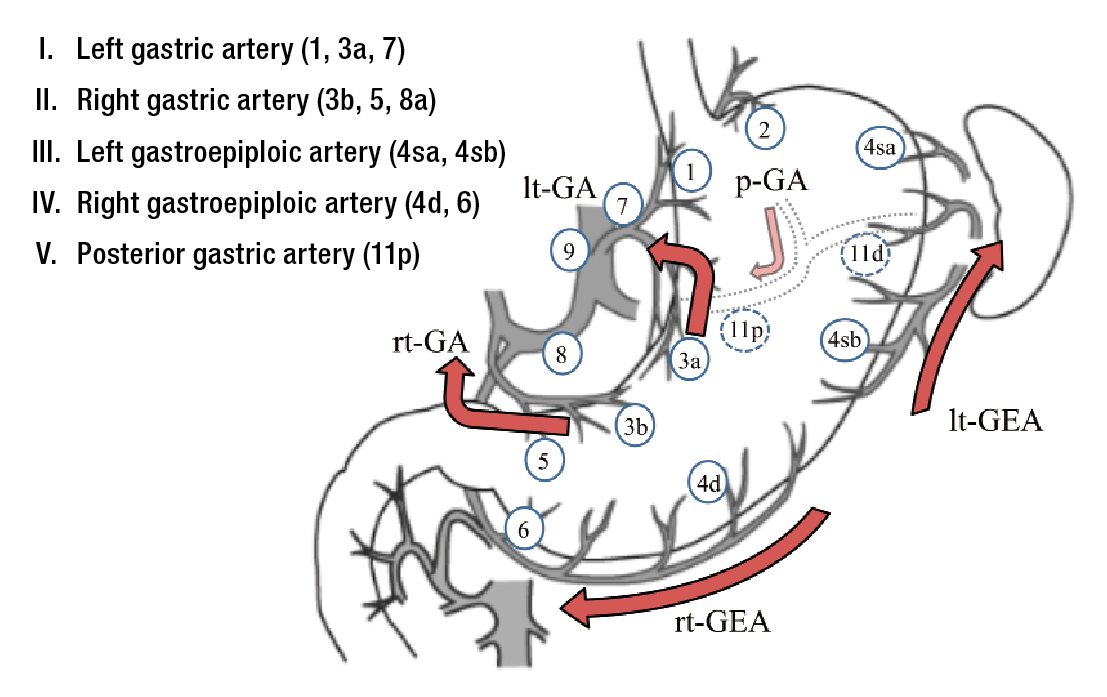
*: Gastric lymphatic basins are classified into five directions shown on the right(Figure 1) 2).
Method of identifying SNs in gastric cancer
Methods of identifying SNs in gastric cancer include the use of a radioisotope (RI) as a tracer, and the use of dye. The RI method is known for a high identification rate, but it poses problems including limited control area and shine through (a phenomenon where the high accumulation of radiation around the RI injection site masks the accumulation of radiation in the proximal SN). Meanwhile, the dye method can be implemented by any facility, and is superior in terms of convenience and cost. Intraoperative administration of dye allows real-time observation of lymph flow.
Cases indicated for SNNS in gastric cancer
- cT1N0M0
- No previous treatment
- Major axis of tumor is 4 cm or less
- Solitary lesion
Those patients exceeding these criteria, turned out to be 1% (4/466 cases) false-negatives (i.e., despite being SN-negative, lymph node metastasis is noted outside the lymphatic basin that includes the SN)1).
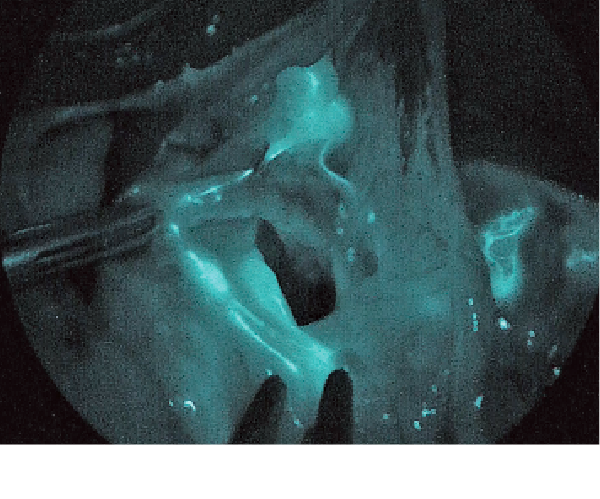
Method of identifying SN using indocyanine green (ICG)
This method entails injecting 0.5 mL each of 0.5% ICG (one ampule of 25 mg is dissolved in 5 mL) on four spots of submucosa around a tumor during a procedure using a gastrointestinal endoscope. Immediately after injection, the lymphatic vessels and lymph nodes that fluoresce under infrared (IR) observation are identified, and the lymph nodes that continue to fluoresce up to 15 minutes after injection are regarded as SNs.
Following the dissection of basins that include SNs, the stained/fluorescing lymph nodes are examined and the SNs are search/ dissect by using the RI count at the back table. The results are submitted to rapid pathological testing.
To those cases diagnosed as SN metastasis negative, SN basin dissection and limited gastrectomy (local resection, segment resection, etc.) is performed. If SN metastasis is positive, D2 lymph node dissection and regular gastrectomy are performed in accordance with gastric cancer treatment guidelines.
SNNS in gastric cancer using IR observation
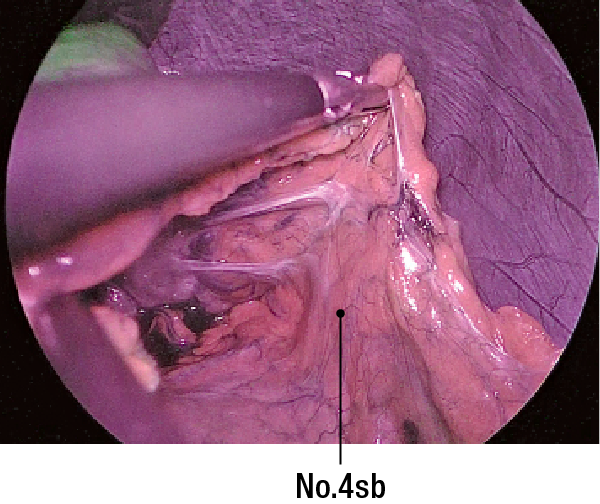
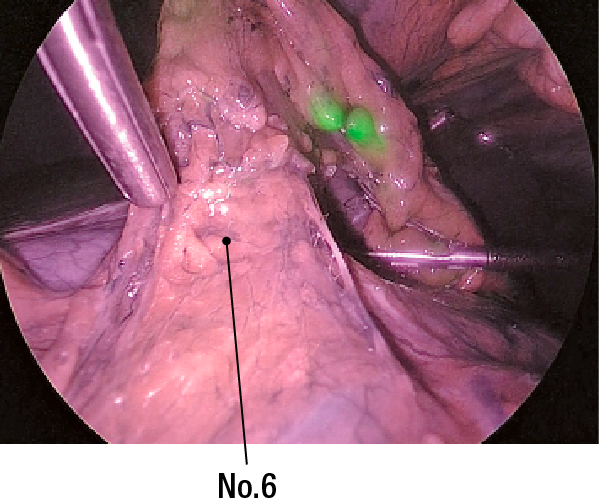
*: Prior to ICG injection, the omental bursa is opened, and adhesions are peeled off so that No.4sb, 6, 7, 8a, and 11p can be observed.
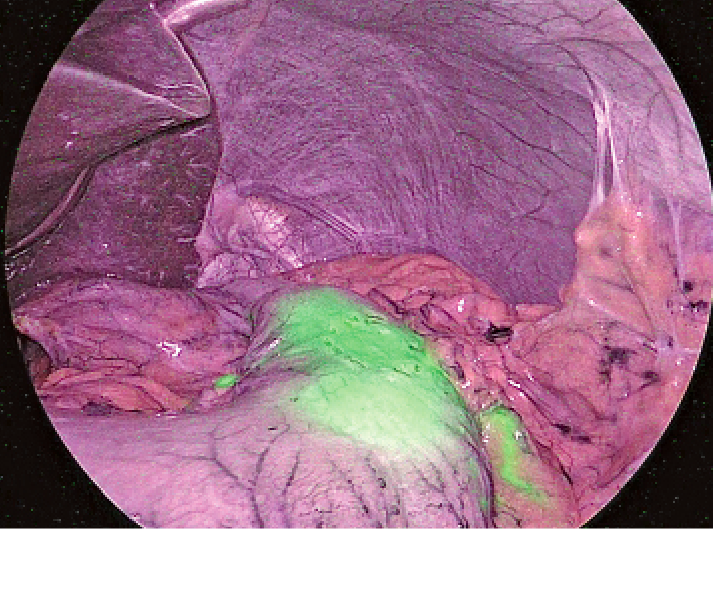
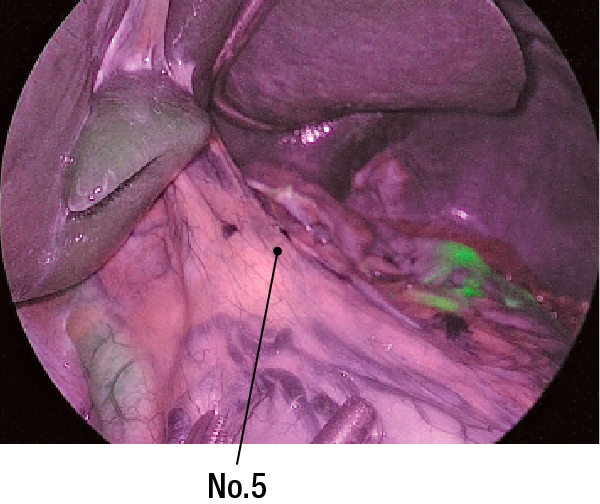
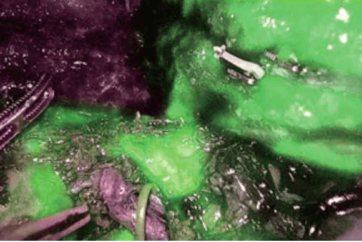
15 minutes after injecting ICG into a lesion on the anterior wall of the upper gastric body
(1) Lymph flow is noted in two directions of the greater curvature side and the lesser curvature sideFigure2Lesser omentum.
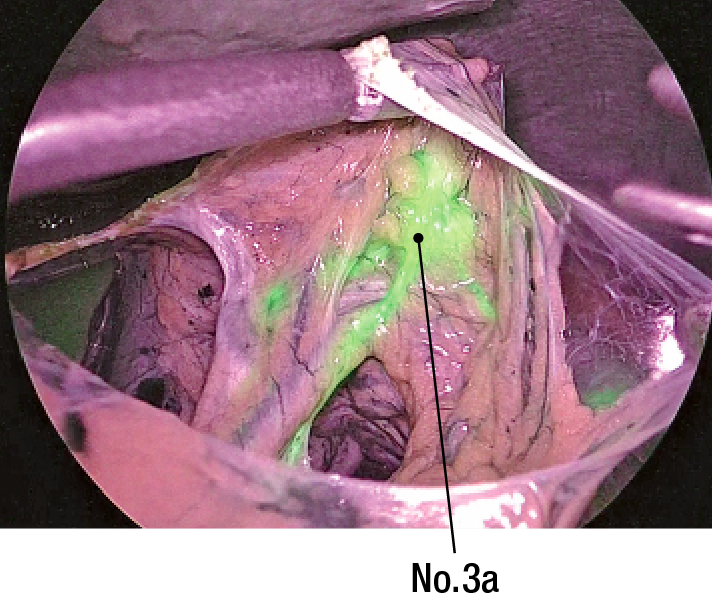
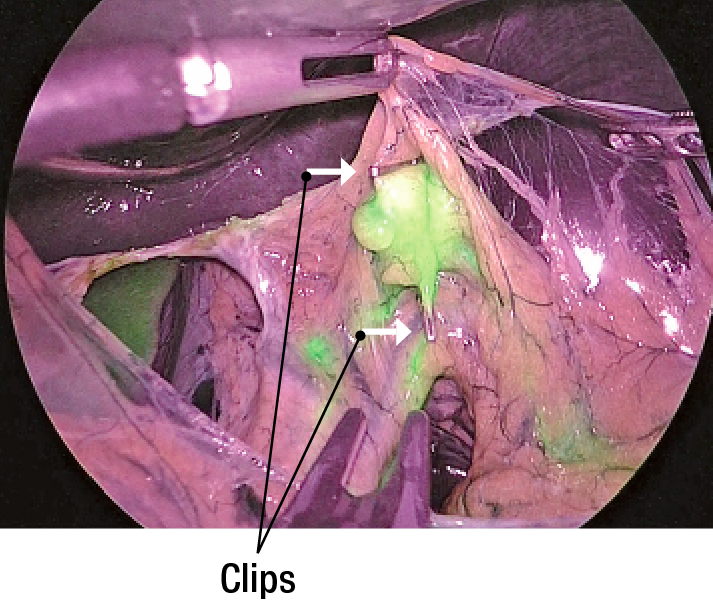
(2) Lesser omentum is incised and observed. No.3a is shown as SN(Figure3). SN is marked by clips(Figure 4).
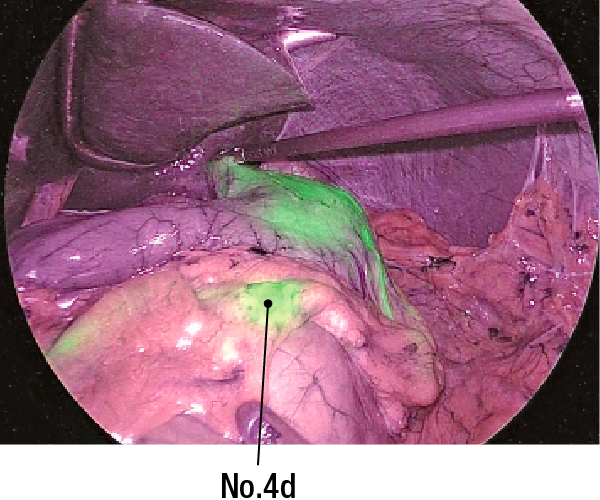
(5) No SNs are noted on No.4sb(Figure 7), No.6 (Figure 8), or No.5 (Figure 9)
*: In this case, the left gastric artery basin (1, 3a, 7) and the right gastroepiploic artery basin (4d, 6) are dissected. Limited surgery was performed with the primary focus on segmental gastrectomy.
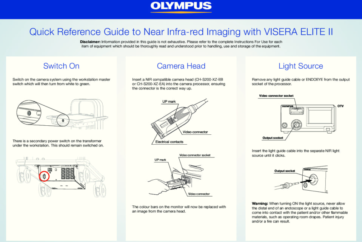
With VISERA ELITE II, a scopist can manually switch from the white light to IR observation light. Conventional IR observation systems do not allow surgical operation concurrently with IR observation. However, IR MODE 1 in this system allows superimposed observation. Surgeons can identify SNs and the pathway of lymphatic vessels while clipping to make markers; enabling smooth operation.
The use of ICG in identifying SNs is off-label. Thus, care should be taken during such use; the approval of the ethical committee of each medical institution may be required.
Currently, “A phase III study of Sentinel Node Navigation Surgery for Early Gastric Cancer” (UMIN00014401) is being conducted as Advanced Therapy of Type B.
2. Kinami S, Fujimura T, Ojima E et al. PTD classification: proposal for a new classification of gastric cancer location based on physiological lymphatic flow. Int J Clin Oncol 2008; 13: 320-329.
- Content Type