Author

Ki-Hun Kim, MD, PhD.
Professor and Chief, Division of Hepatobiliary Surgery and Liver Tr ansplantation, Depar tment of Surgery, Asan Medical Center, Ulsan Univer sity, Seoul, Korea.
Biography
Dr. Ki-Hun Kim graduated from Korea University College of Medicine in 1992 where he earned PhD degree in 2003, and completed a surgical resident training in Korea University hospital in 1998. He was a visiting professor of Surgery at Kobe University Hospital, Kobe, Japan in 2006, and participated in the Multivisceral Transplantation Program as a visiting professor at Miami Transplant Institute, University of Miami, USA in 2007. He was a secretary general in the international meeting for HCC 2008, IHPBA 2014, ELSA 2015, ELSA visionary summit 2017, and ISLS 2018. He is currently a chair, scientific committee of KAHBPS, secretary general of ISLS, council member of APHPBA, and an advisory board of ILLS. He performed the first successful pure laparoscopic living donor hepatectomy in 2008, Asia-Pacific region and multivisceral transplantation with a pediatric surgeon in 2011, Korea
IR observation in laparoscopic living donor hepatectomy
Liver transplantation is the most effective treatment for end-stage liver disease. The growing disparity between the number of liver transplant candidates and the supply of deceased donor organs has motivated the development of living donor liver transplantation (LDLT). Since living donors are not being operated on in a pathological condition, it is useful to operate with a laparoscopic procedure with less scarring. However, laparoscopic anatomical liver resection (LALR) procedures are very difficult to reproduce, and the confirmation of demarcation of the hepatic segment on a monitor is also challenging. Recently, indocyanine green (ICG) fluorescence imaging has been used to identify hepatic tumors and segmental boundaries during hepatectomy. When the VISERA ELITE II (Olympus) was used as the near-infrared (IR) imaging system for ICG fluorescence imaging, LALR using ICG fluorescence imaging is a feasible procedure as a tool for intraoperative real-time navigation, because ICG fluorescence provides excellent visualization of demarcation lines and identification of the boundaries of cone units, hepatic segments, and sections.
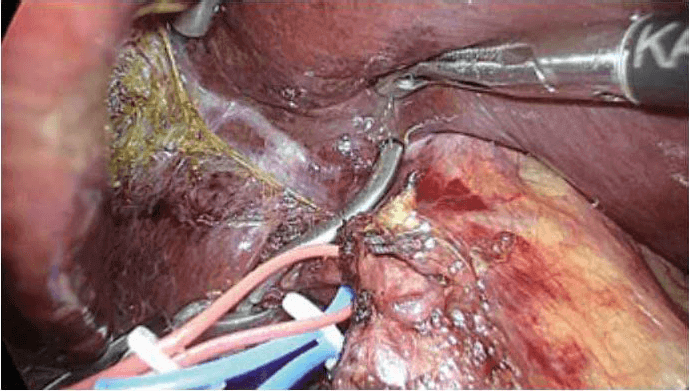
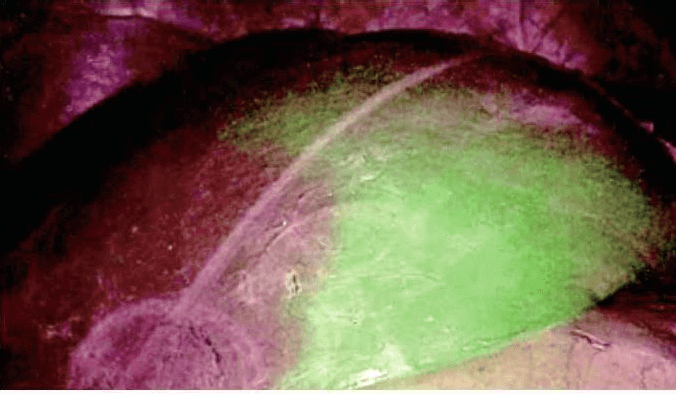
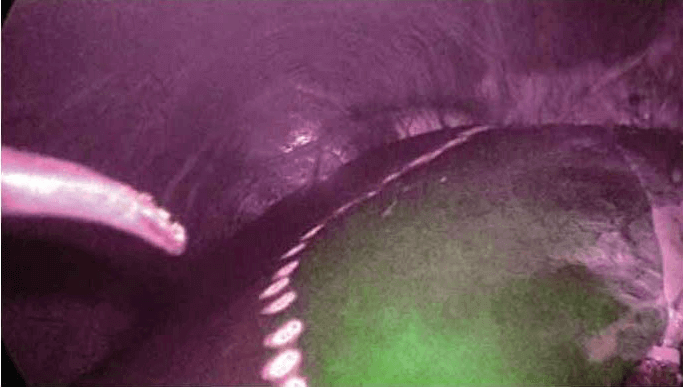
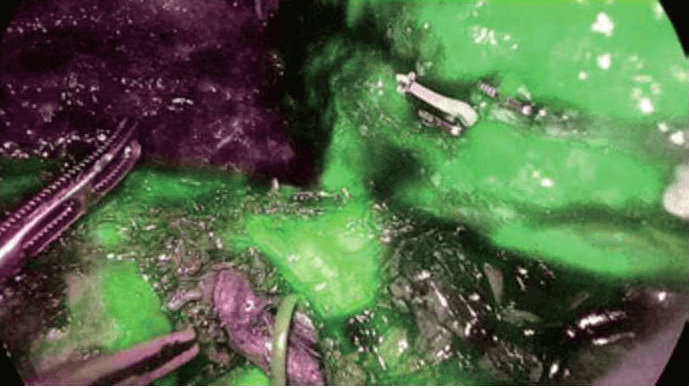
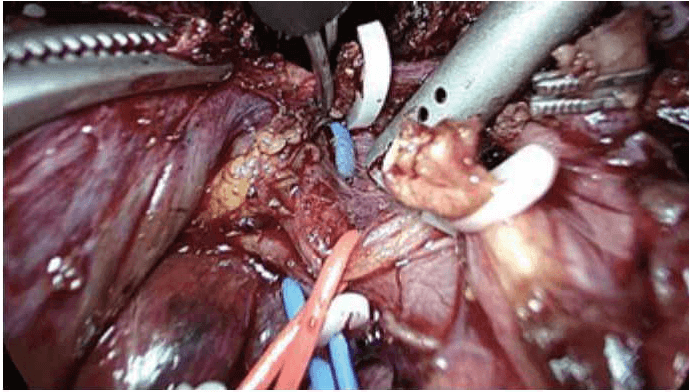
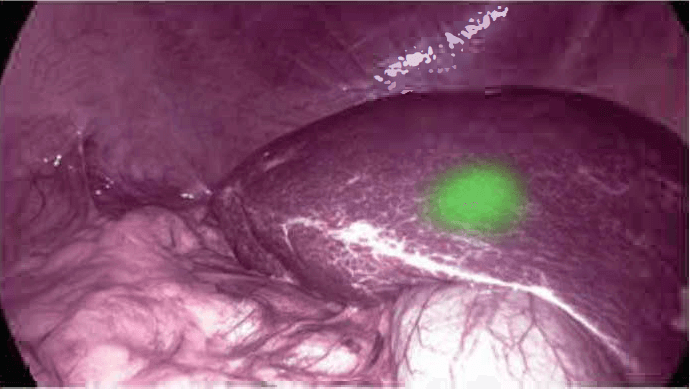
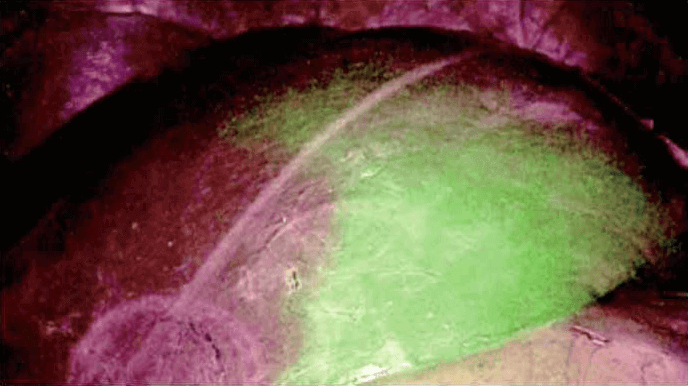
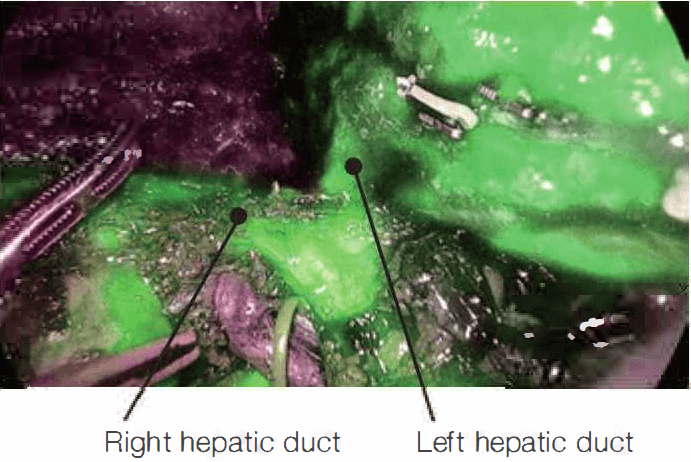
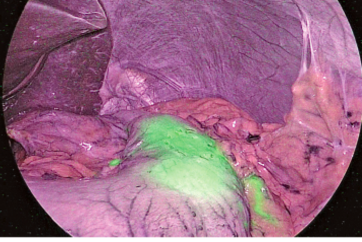
Laparoscopy is currently utilized in liver resections with minimally invasive surgical techniques. Recently, more difficult surgeries such as living donor hepatectomy have been performed with laparoscopy. Figure 1 to figure 6 show the case of a patient who experienced right hepatectomy as a living donor in a liver transplantation.
Role of IR observation in HBP surgery using ICG
IR observation using ICG in liver laparoscopic procedures is used to identify hepatic tumors, hepatic segments, and bile ducts or bile leakage in donor surgery. Among these uses, the most common one is to view hepatic segments. The second most useful application is for the safe resection of the bile ducts in case of or if there is the anatomical variation of bile duct during donor surgery by viewing the precise shape of bile ducts. In addition, for hepatic tumors, if the margin of the tumor is unclear, it can be useful to determine the resection margin.
1. Hepatic tumors
To identify hepatic tumors, ICG is administered at a dosage of 0.25 mg/kg 24 to 48 hours prior to the surgery. One vial of ICG contains 25 mg of ICG powder, which when mixed with 10 cc of sterile water yields a 2.5 mg/ml solution of ICG. However, the optimal ICG dosage is not well established and differs between IR systemic devices from different manufacturers. When the lesion of the tumor is unclear, a few days before surgery, ICG is just injected intravenously, and the tumor area is shown as green color due to the inability of the hepatic tumor to detoxify. ICG is completely deposited on the surface of the liver and is gradually left just in the tumor as it is washed out.
2. Hepatic segments
ICG dose for tumors, hepatic segments, and bile ducts does not differ, but the period of injection is slightly different. For liver resection, it is important to determine the resection margin of the segment to be removed in anatomical liver resection. If on the preoperative examination such as CT or MRI, the segment or section to be removed includes tumor
with sufficient resection margin, 2.5 mg of ICG is injected intravenously after isolation and clamping of the Glisson of the liver to be excised. Then, ICG is administrated into the entire remnant liver segments, excluding the clamped side. Finally, mark it on the liver surface and change IR mode into white light imaging (WLI) mode.
3. Bile ducts in donor surgery
It is very important to determine the division site of the bile duct in donor hepatectomy. This is because wrong division of bile duct can cause severe complications to the donor. Donor surgery requires more careful attention because it is not the operation in pathological status. After the ICG is administered intravenously, it is initially deposited on the liver parenchyme, and later remained only in the bile duct as time passes through the wash out process. About 2-3 hours after the administration of ICG, the biliary tract becomes green and shows precise division point. IR observation could make difficult donor surgery more safety.
Tips and cautions in the application of IR observation for liver resection
The usage of ICG (Table 1) in laparoscopic hepatectomy is very important. Anatomical liver resection in hepatocellular carcinoma (HCC) is better than non-anatomical liver resection in terms of oncological outcomes. Therefore, it is very important to make sure that the territory for the resection by ICG is defined. In addition, it is important in donor surgeries that the resection of the liver occurs according to the original anatomic plan to ensure the remaining liver volume in the donor is sufficient. For this, the usage of ICG is very important.
| Application | ICG dosage | Timing of injection |
| Hepatic tumors | 0.25 mg/kg | 24 to 48 hours prior to the surgery |
| Hepatic segments | 2.5 mg | after the time of clamping |
| Bile ducts | 2.5 mg | 2-3 hours prior to the detection |
· To identify hepatic tumors, ICG is administered at a dosage of 0.25 mg/kg 24 to 48 hours prior to the surgery.
· For hepatic segmentation, it is important to see where the margin of the particular segment is and not the tumor itself and 2.5 mg of ICG is injected intravenously on the day of surgery after hepatic artery and portal vein isolation and clamping
· In donor surgery, when the bile duct, hepatic artery, and portal vein are separated from each other and clamped, ICG is administrated. About 2-3 hours after the administration of ICG, the biliary tract becomes green and shows the part that is divided from common bile duct
References
1. Lee SG. A complete treatment of adult living donor liver transplantation: a review of surgical technique and current challenges to expand indication of patients. Am J Transplant. 2015 Jan; 15(1): 17-38
2. Urade T, Sawa H, lwatani et al. Laparoscopic anatomical liver resection using indocyanine green fluorescence imaging. Asian J Surg. 2019 Apr 28
pii: S1015-9584(19)30220-9. doi: 10.1016/j.asjsur.2019.04.008. [Epub ahead of print]
3. Kim KH, Kang SH, Jung DH et al. Initial outcomes of pure laparoscopic living donor right hepatectomy in an experienced adult LDLT center. Transplantation 2017 May; 101(5): 1106-10
- Content Type