Author

Takeaki lshizawa, M.D., Ph.D., F.A.C.S., Hepato-Biliary-Pancreatic Surgery,
Cancer Institute Hospital of Japanese Foundation for Cancer Research
Biography
Graduated from Chiba University in 2000. While working as a clinician at the Hepatobiliary and Pancreatic Surgery Division, Department of Surgery, Graduate School of Medicine, The University of Tokyo, started to develop intraoperative fluorescent imaging in 2007. Made a profound study of laparoscopic surgical procedures at the Institut Mutualiste Montsouris (Paris) in 2011. Occupied with the present post since 2014 and performs a wide range of both laparotomic and laparoscopic hepato-biliarypancreatic procedures aided by the active use of fluorescent imaging.
Usability of IR Observation in Laparoscopic Liver Resection
The role of IR observation using ICG in liver resection is to identify ① liver tumors, ② hepatic segments, and ③ bile ducts / bile leakage. For laparoscopic surgeries in particular, IR observation is a technique that is advantageous in terms of compensating for the limitations of manual palpation and facilitating image modification.
①Liver tumors can be identified by utilizing the phenomenon where ICG (0.5 mg/kg) intravenously injected for a liver function test before surgery is retained in the cancerous tissues of hepatocellular carcinoma (HCC) and noncancerous liver parenchyma surrounding metastatic liver cancers, which is consistent with local biliary excretion disorders [1, 2]. If ICG examination is performed within two weeks before surgery, hepatic subcapsular tumors can often be identified by IR observation.
② In order to visualize the hepatic segmental border, the portal branches are punctured under the guidance of ultrasonography and ICG diluted to about 0.1 mg/mL is injected [3, 4]. Because puncture of the portal branches is difficult in laparoscopic procedures, a negative-staining technique is often utilized. This involves temporarily clamping the root of the Glisson’s pedicle for the cancer-bearing hepatic segment and then intravenously injecting 1.25 mg of ICG [5].
③ By cholangiography, while biliary excretion of preoperatively injected ICG continues, fluorescence images of extrahepatic bile ducts can be obtained without intraoperative additional administration of ICG. When the intraoperative administration is needed, 1.25 to 2.5 mg of ICG is injected intravenously. Bile ducts can be visualized from about 15 minutes until 6 hours after intravenous injection [6]. Direct injection of diluted ICG into bile ducts may also be used [7].
Laparoscopic Resection of S6 of Liver (HCC) Using IR Observation
1 Injection of ICG
In principle, the ICG retention rate at 15 minutes is measured in all cases as a liver function test before hepatectomy. In the present case, ICG (0.5 mg/kg) was injected intravenously two days before surgery (measured value: 12%).
2 Placement of Trocars and Mobilization of Liver
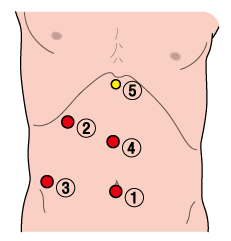
Surgery was initiated by positioning the patient with the legs open, the right hand raised, and only the upper body placed in the left lateral decubitus position. Trocars were placed at 5 locations (Figure 1), and the right liver was mobilized to the front of the adrenal gland.
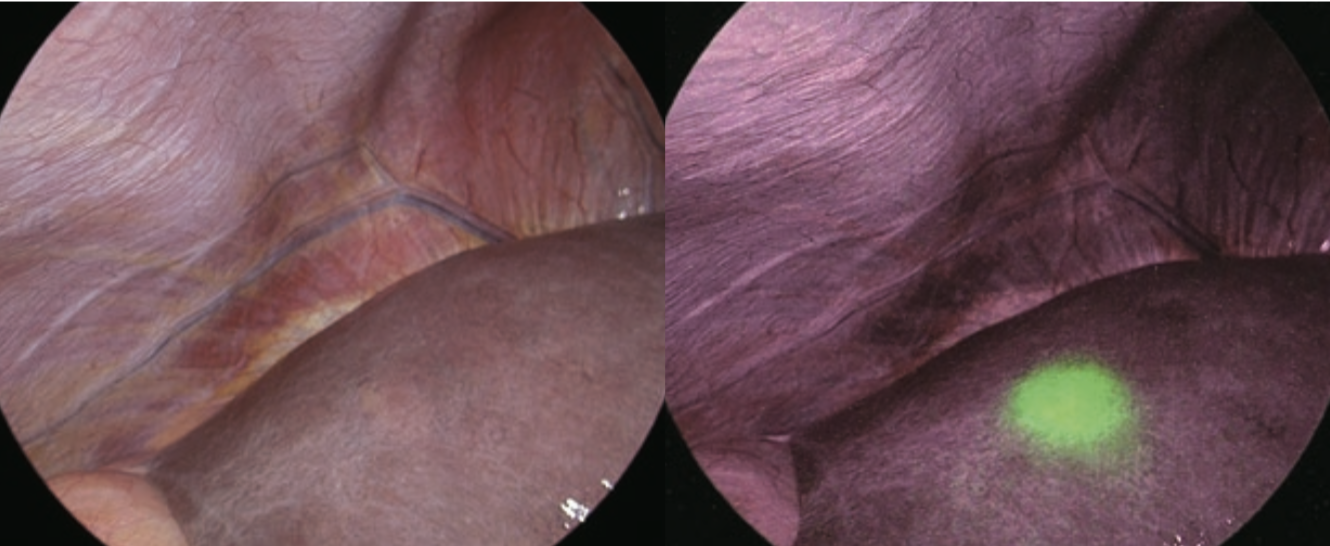
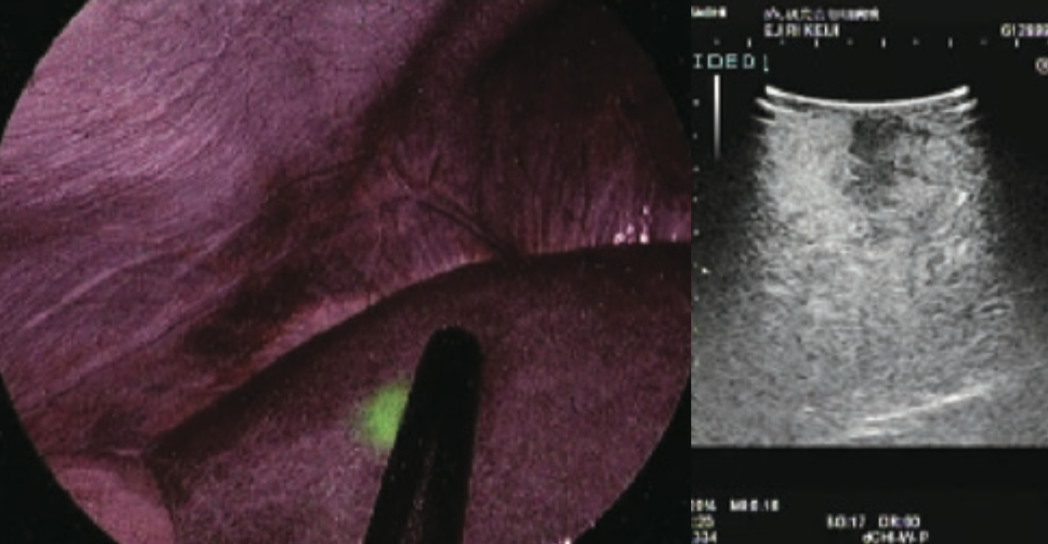
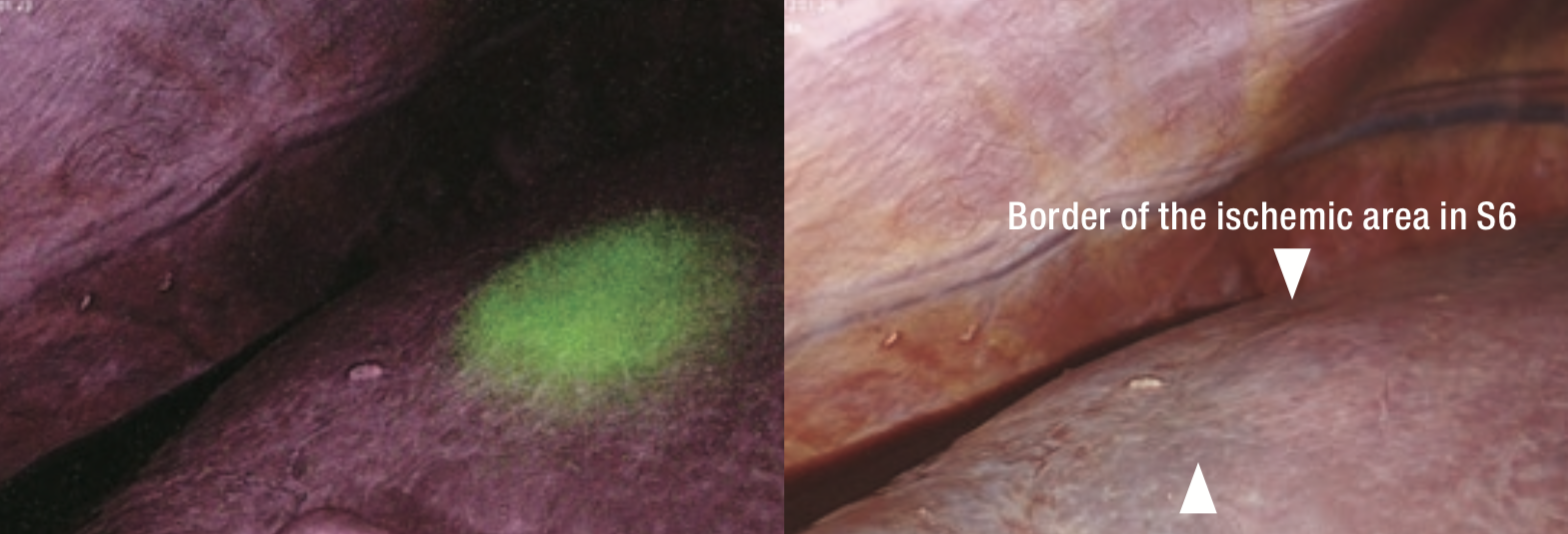
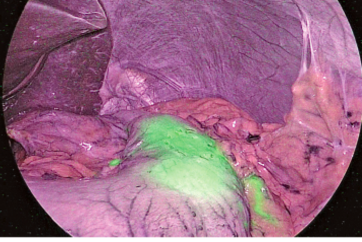
3 Identification of Tumor by IR Observation and Intraoperative Ultrasonography
Switching to observation of liver surfaces in IR MODE, a clear fluorescent area was found in the cranial portion of S6 of the liver, which corresponded with the ultrasound findings of HCC (Figures 2 and 3). No fluorescent area suggesting a tumor was detected at other locations.
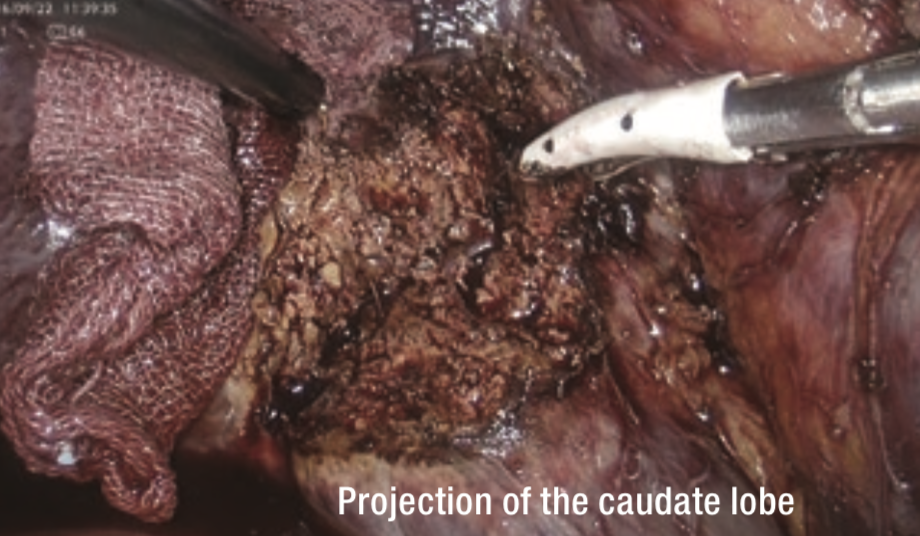
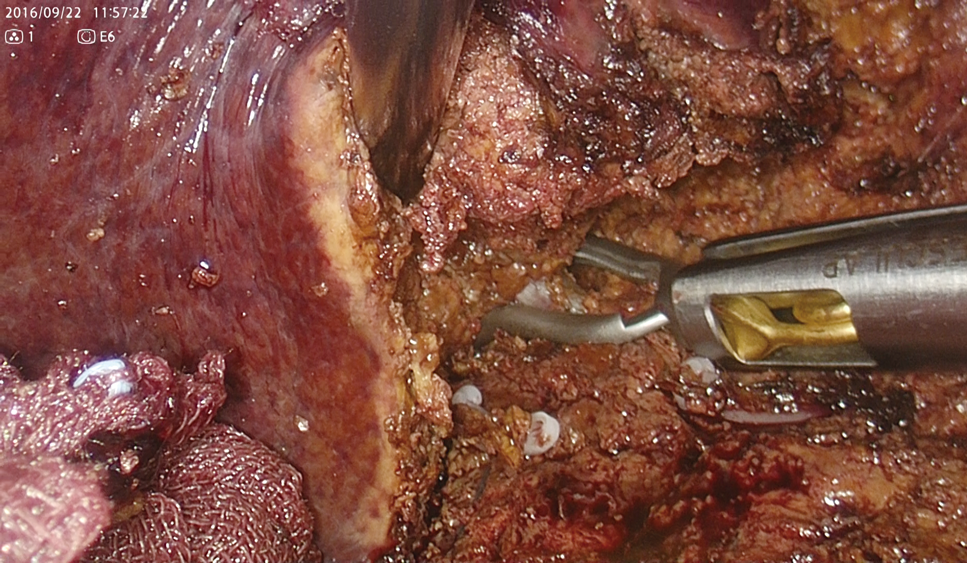
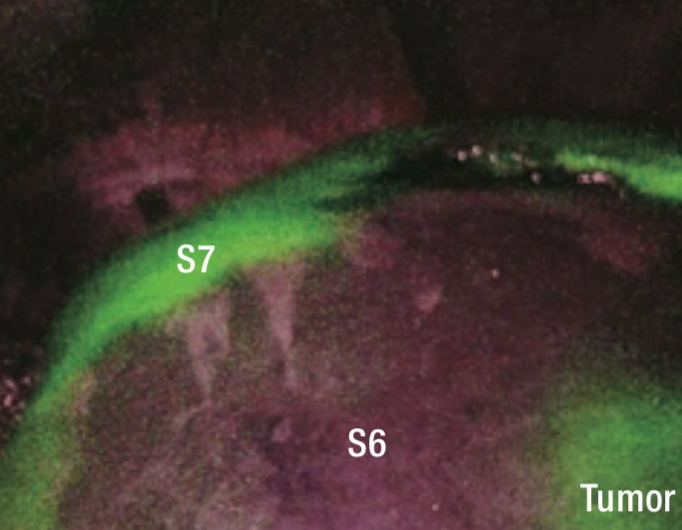
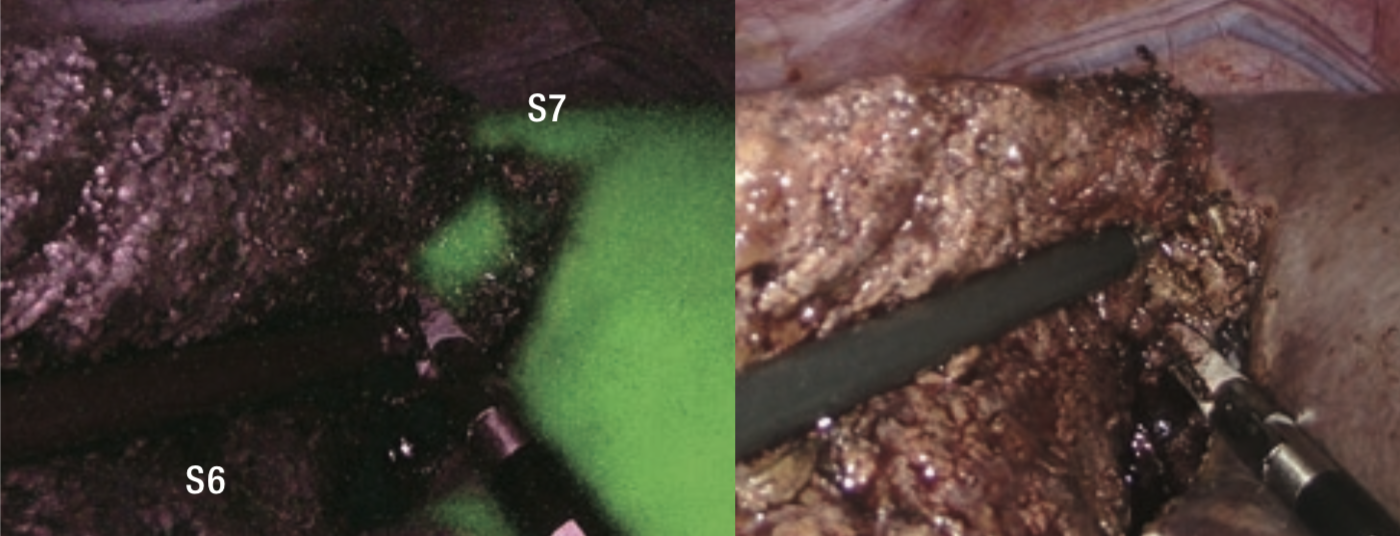
4 Liver Transection and Identification of Glisson’s Sheath in S6
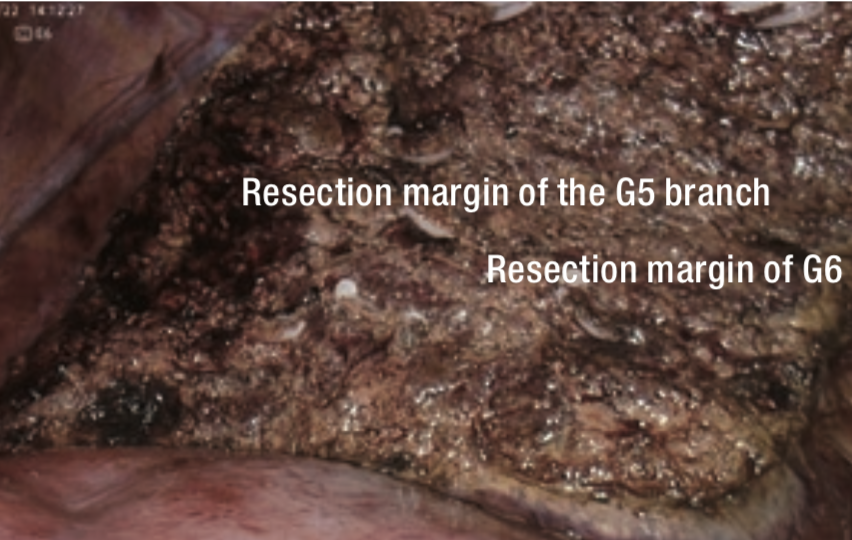
Because Rouviere’s sulcus was unclear, the junction of the gallbladder was dissected and the excavation between the projection of the caudate lobe and the posterior segment was transected in a direction perpendicular to the axis of Glisson’s sheath in the posterior segment (Figure 4). Then, a fine Glisson’s sheath running toward the ventral side of S6 was dissected. Behind it, the vessel that appeared to be the main trunk of Glisson’s sheath in S6 (G6) was identified and the vessel was clamped using bulldog forceps (Figure 5). When observing the ischemic area that appeared on the liver surface, the tumor appeared to deviate toward the inside of the ischemic area in S6 (Figure 6). On repeat ultrasonography, the branch of Glisson’s sheath in S5 (G5) originating from the dorsal branch of S8 extended to the inside of the tumor. The liver parenchyma was transected from the caudal to cranial side along the ischemic area at S5/6 border to reach the G5 branch, and it was dissected (Figure 7).
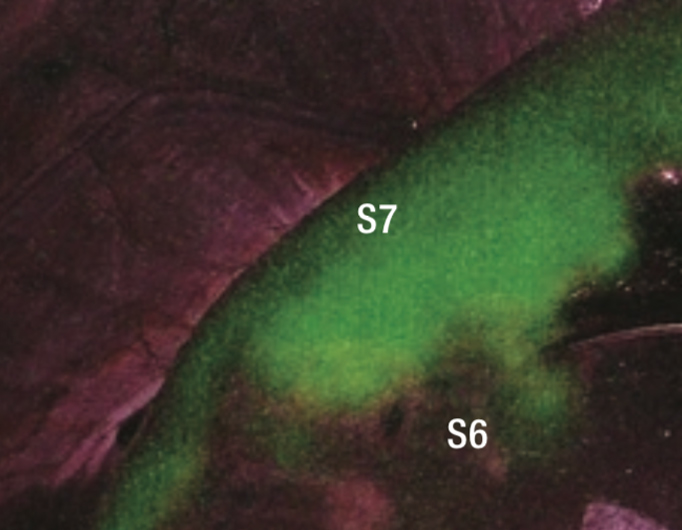
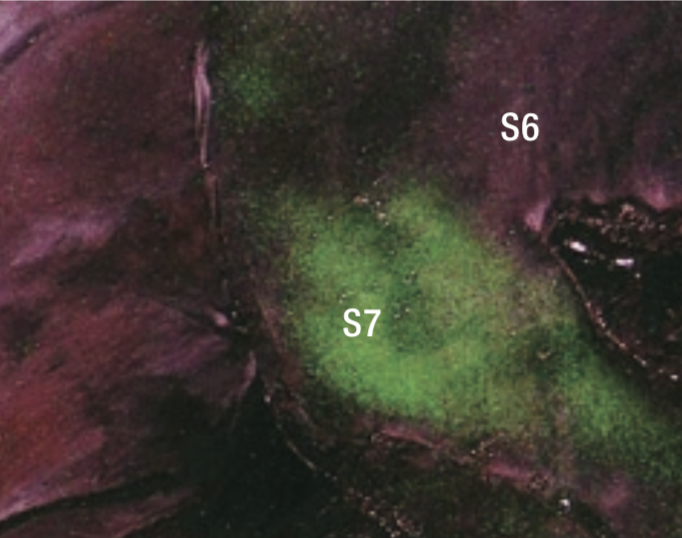
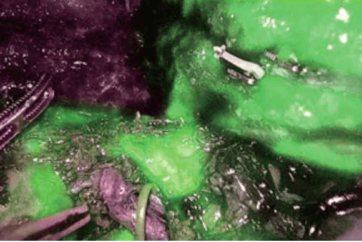
5 Identification of Hepatic Segments Using IR Observation
When observing liver surfaces in IR MODE after intravenous injection of ICG at 0.5 mL (1.25 mg), the entire S6 segment excluding tumorous fluorescence and part of S5 were clearly visualized as nonfluorescent areas (Figures 8 to 10). Having confirmed blood flow to S7 by this method, the bulldog forceps were removed and G6 was dissected.
6 Liver Transection along the Hepatic Segmental Border and Resection of a Specimen
The border of the nonfluorescent area on the liver surface was marked using electrocautery. Liver transection was performed while checking the hepatic segmental border using IR MODE as appropriate (Figure 11), and S6 resection extended to S5 was completed (Figure 12).
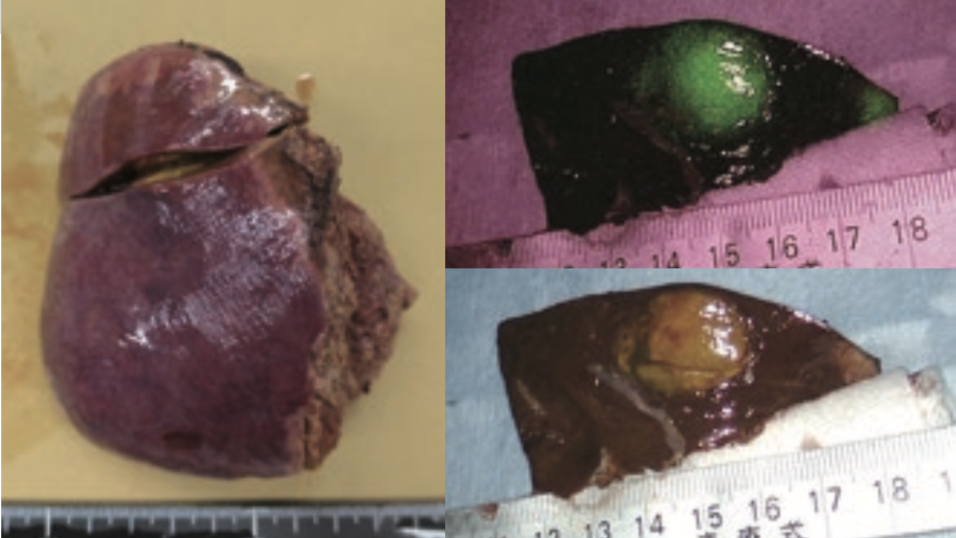
7 Bile Leakage Test by IR Observation
After wiping the liver transection plane with gauze, the absence of fluorescence signals suggesting bile leakage was confirmed in IR MODE observation (Figure 13). Fluorescence observation of cross-sections of the resected specimen showed ICG fluorescence throughout the tumor tissue, which was consistent with the findings of HCC with preserved bile productivity (Figure 14). According to histopathological diagnosis, it was moderately differentiated HCC.
Tips and Cautions in Application of IR Observation to Liver Resection
- The diagnosis of liver cancer is associated with high false-positive rates (20% to 40%). When a fluorescent area is observed at a location other than that where a tumor was detected by preoperative diagnosis, additional resection should be performed if the diagnosis as malignant tumor is supported also by other intraoperative diagnostic modalities such as ultrasonography. To reduce the false-positive rate, ICG examination on the day before surgery should be avoided especially in patients with decreased liver function due to chemotherapy and/or hepatitis/cirrhosis.
- For identification of hepatic segments, an increase in fluorescence signals in an ischemic area can be prevented by administering only a small amount of ICG (intravenous ICG administration at 1.25 mg for negative staining of the ischemic area) and clamping the relevant Glisson’s sheath for at least 10 minutes.
- It should be noted that the use of ICG for fluorescent imaging during abdominal surgery is currently off-label use in some countries including Japan.
References
1.Cancer 2009;115:2491-504.
2.Ann Surg Oncol 2014;21:440-8.
3.J Am Coll Surg 2015;221:e27-36.
4.Ann Surg 2015;262:1092-101.
5.Arch Surg 2012;147:393-4.
6.Br J Surg 2010;97:1369-77.
7.Arch Surg 2009;208:e1-4.
- Content Type