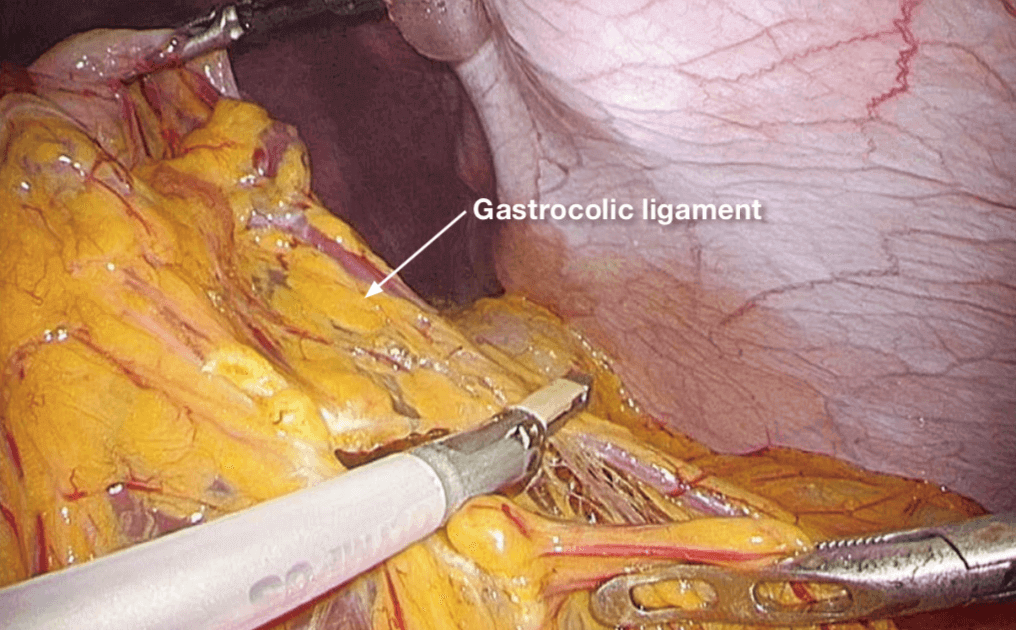
1.Transection of the gastrocolic ligament
The surgeon (left hand) and assistant (right hand) grasp the greater curvature at two rostral points opposite the angular incisure, and between those two points, a triangle is created, with the existing space being used as the base. To do this, the assistant grasps (left hand) the gastrocolic ligament. The gastrocolic ligament is then cut in the direction of the inferior splenic pole ≥3 cm from the gastroepiploic arcade.
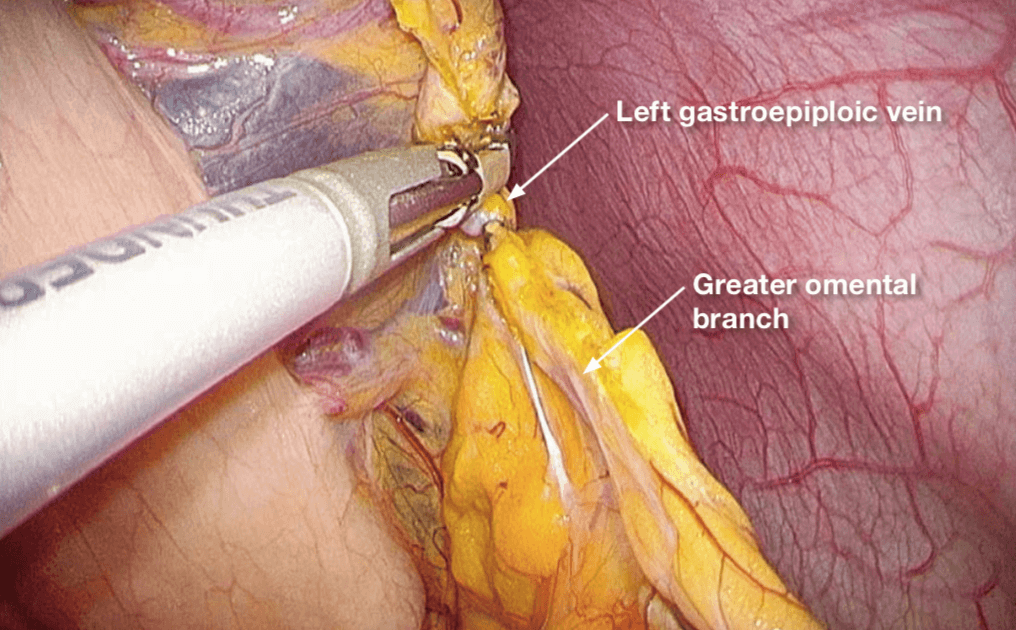
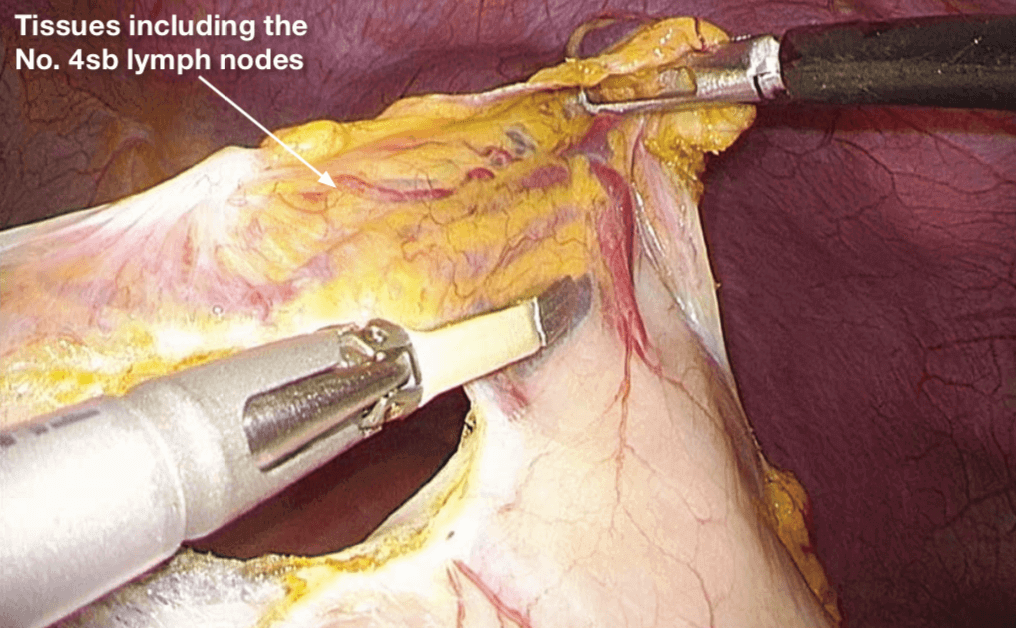
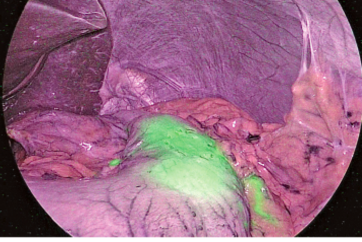
2.Dissection of No. 4sb lymph nodes
The main trunk of the left gastroepiploic vein is transected at the level of the greater omental branch.
At this time the remaining side of the main trunk of the left gastroepiploic vein is singly clipped, and the THUNDERBEAT™ device alone is used to cut the resected side of the vein.
The assistant uses both hands to apply traction ventrally to the adipose tissues that will be dissected, and the watershed region formed on the posterior wall of the stomach is confirmed. In addition, dissection of the No. 4sb lymph nodes is performed in the caudal to rostral direction from the watershed region.
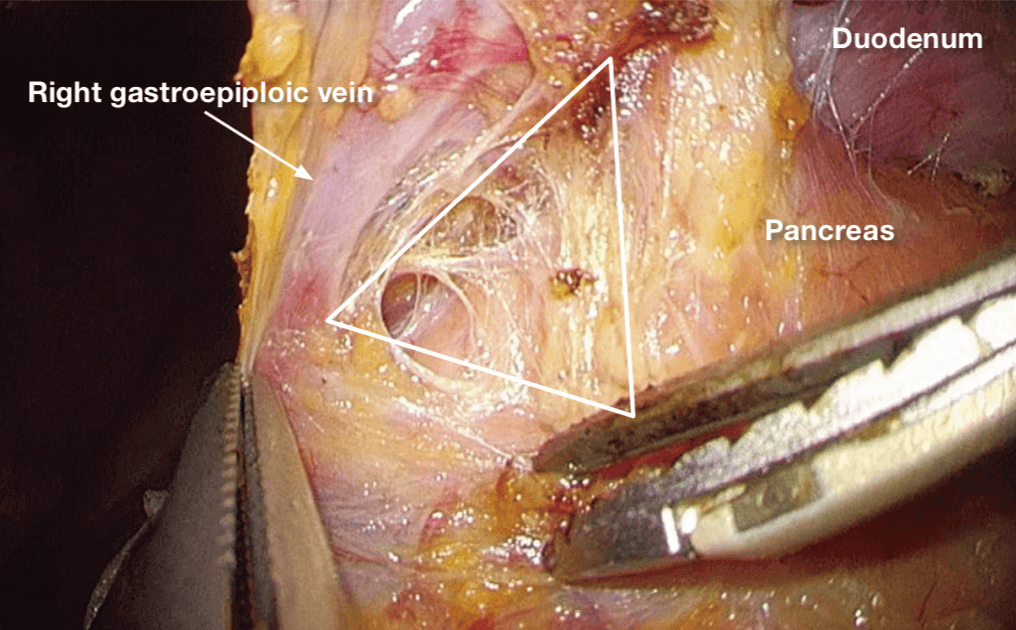
3.Dissection of No. 6 lymph nodes
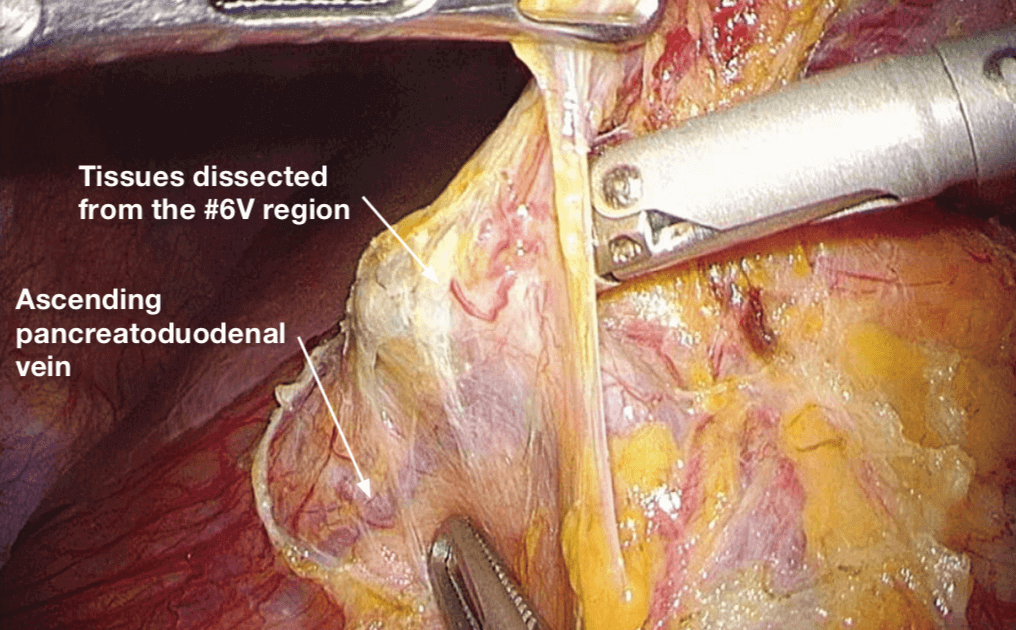
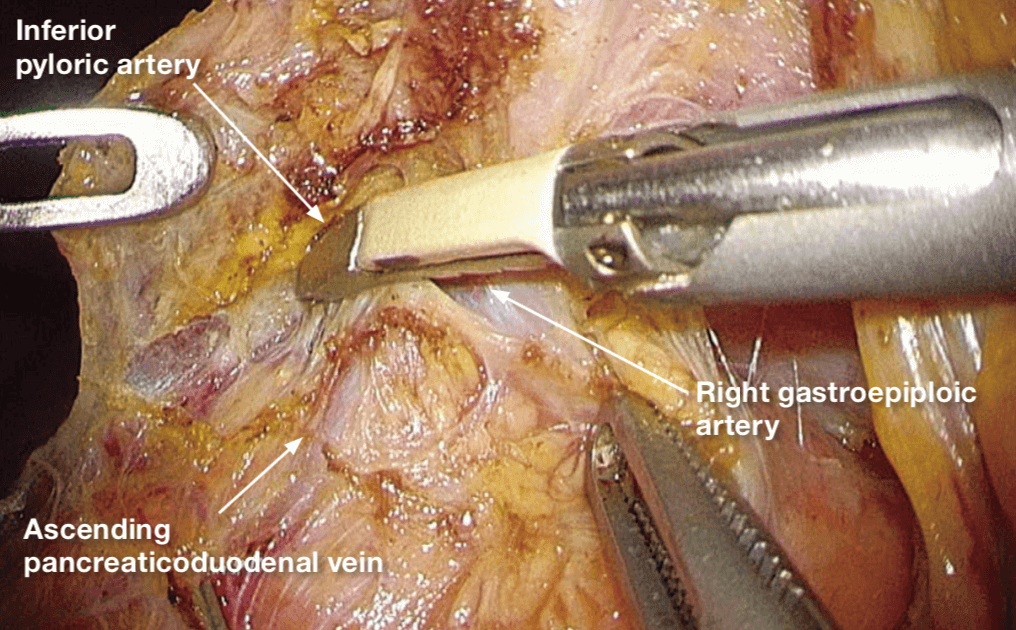
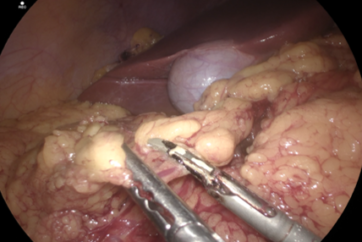
The right gastroepiploic blood vessels run alongside one another peripherally, but at the site where the gastroepiploic artery bifurcates from the gastroduodenal artery, a delta-shaped gap exists between the artery and nerve close to the bottom of the pancreatic parenchyma (indicated by the white triangle). The comparatively thick autonomic nerves that run parallel to the right gastroepiploic artery bifurcate into a reticulate network on the anterior surface of the pancreas and cover the anterior surface of the ascending pancreaticoduodenal vein. The connective tissue surrounding the layer of nervous tissue on the anterior surface of the pancreas is the correct layer of dissection. This layer can be dissected easily by blunt approach from the aforementioned delta-shaped space between the vessels.
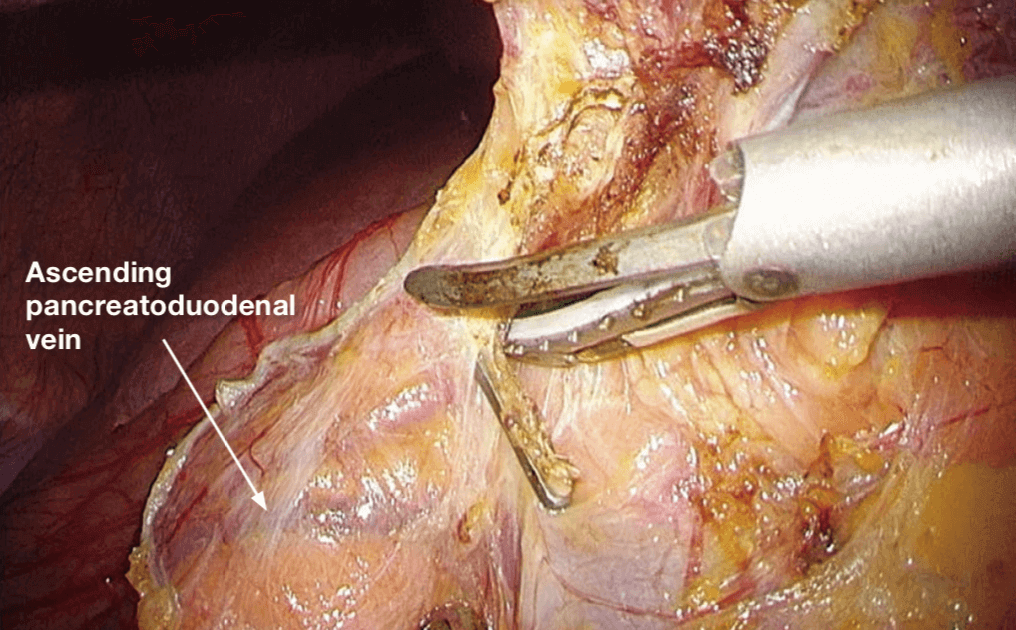
Dissection is performed in a somewhat diagonal and dorsal direction from the delta-shaped gap between the artery and vein. During blunt dissection, the ascending pancreaticoduodenal vein is used as an indicator, and it becomes possible to elevate the tissues that should be dissected (#6V region) from the layer of nervous tissue on the anterior surface of the pancreas. If the right gastroepiploic vein is cut inadvertently, the tissues shrink and dissection becomes difficult; therefore, the artery and vein should be cut before dissection.
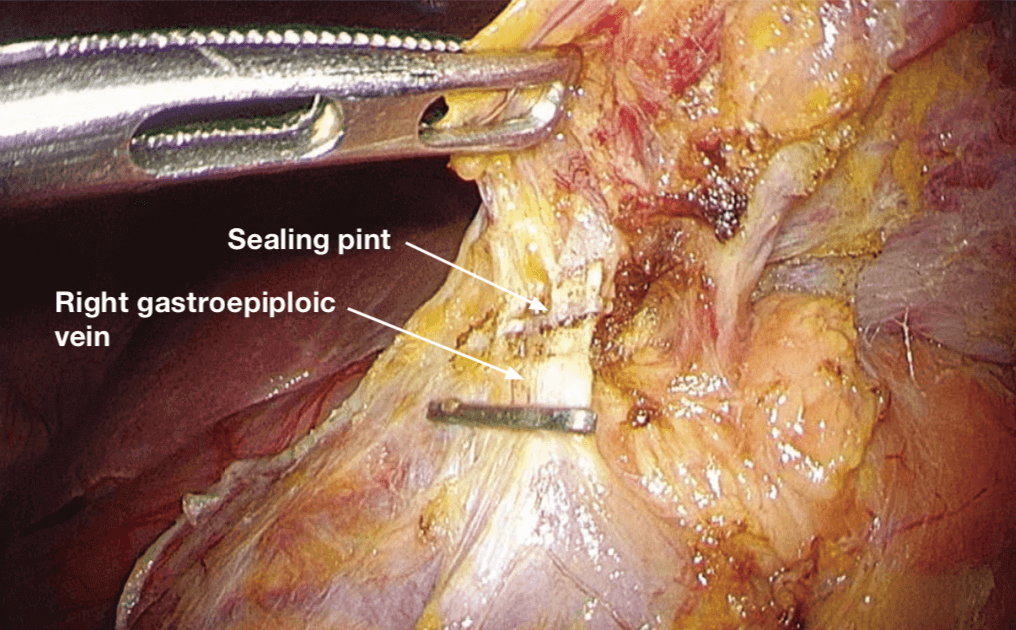
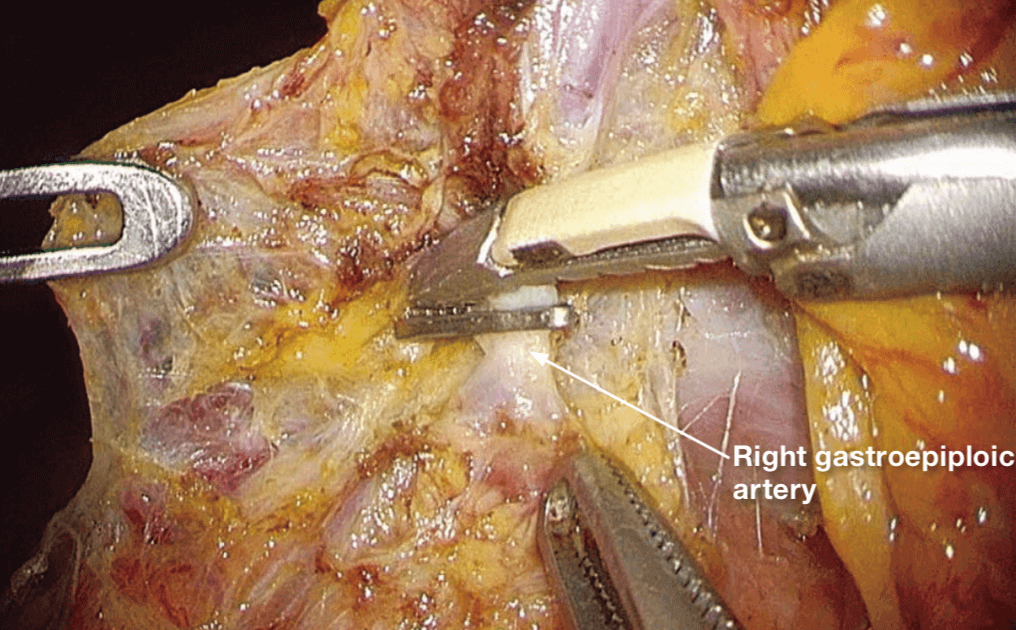
Clipping the root of the right gastroepiploic vein.
Because the vein has been cut dorsally, it is not necessary to dissect the whole circumference of the vein. The THUNDERBEAT™ device is used in sealing mode to coagulate the resected side of the vein trunk.
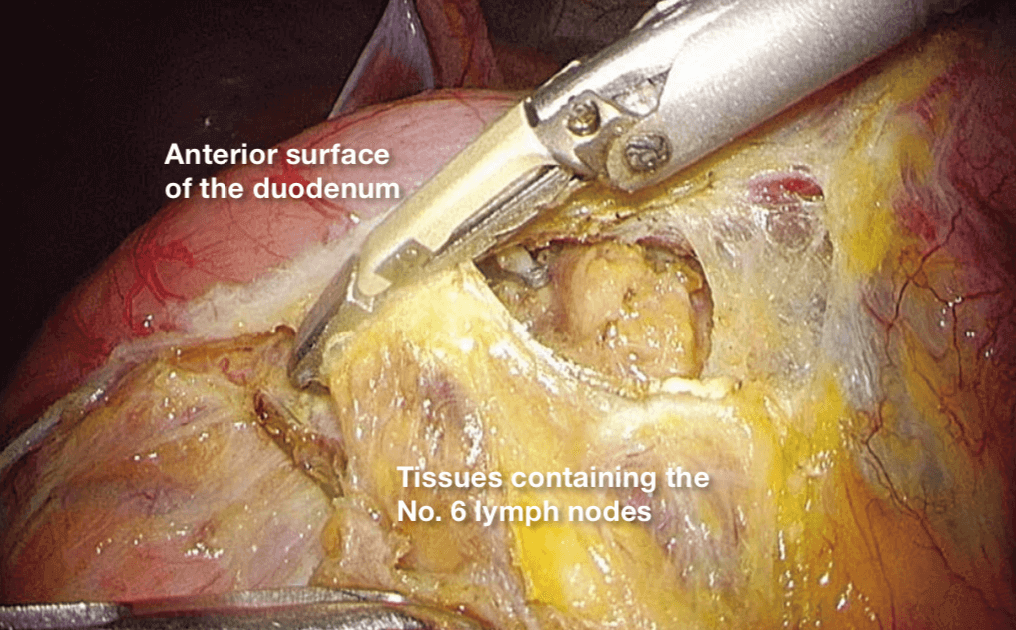
The dissected tissues, which have already been lifted with the tissue layer overlying the anterior surface of the pancreas (#6V region), are cut along the ascending pancreaticoduodenal vein in the direction of the duodenum.
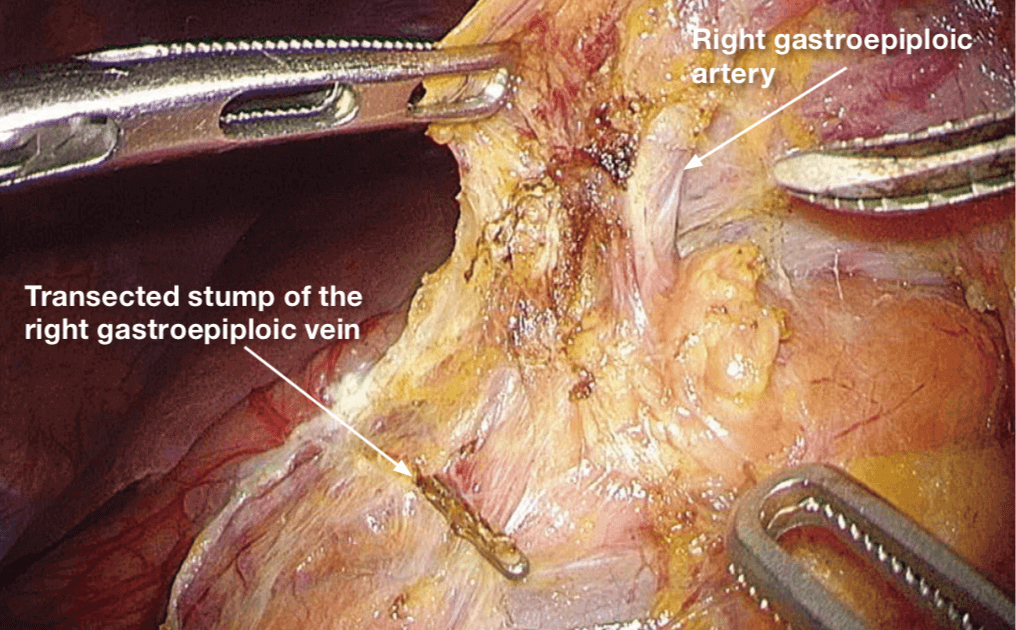
When the right gastroepiploic artery is cut, the clipped stumps obstruct transection of the inferior pyloric artery. For this reason, the right gastroepiploic artery is not dissected after it is transected, but the inferior pyloric artery is dissected. If the inferior pyloric artery is not exceptionally thick, it is not clipped; instead, it is transected with the THUNDERBEAT™ device.
After the inferior pyloric artery has been transected, the root of the right gastroepiploic artery is transected. The remaining side is singly clipped, and the resected side (peripheral vessel) is cut with the THUNDERBEAT™ device.
When tissues are dissected from the duodenum, they are usually dissected after ventral elevation, but because the surgeon is standing on the patient’s right side, it is usually easiest to dissect away from the pylorus, moving ventrally via the duodenum.
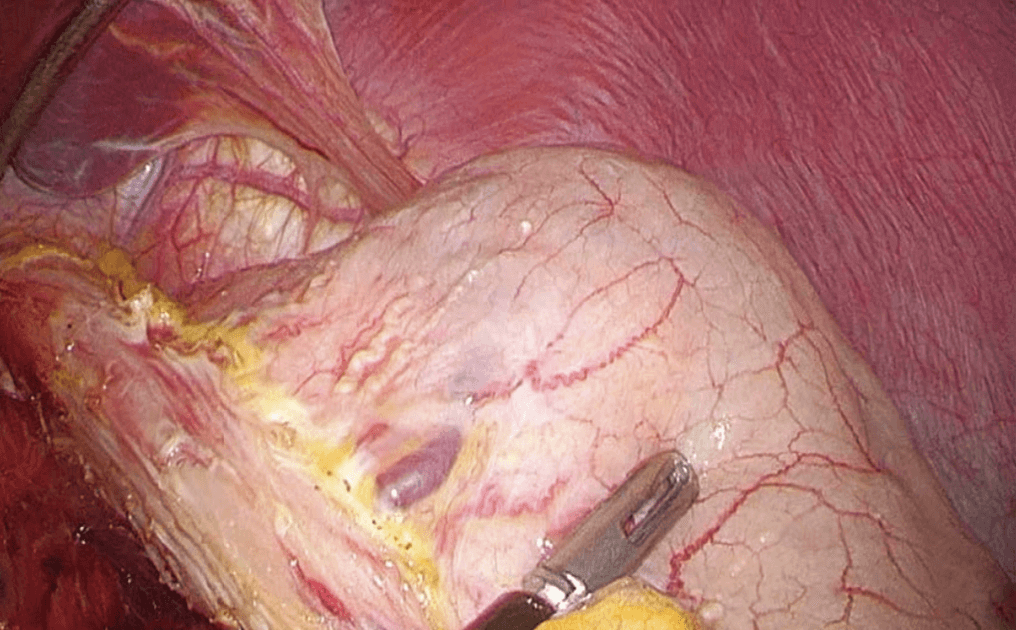
4.Dissection of No. 1 and No. 3 lymph nodes (anteriorsurface of the stomach)
After the duodenum is cut, the mesogastrium is cut, and the presence or absence of an accessory hepatic artery is ascertained.
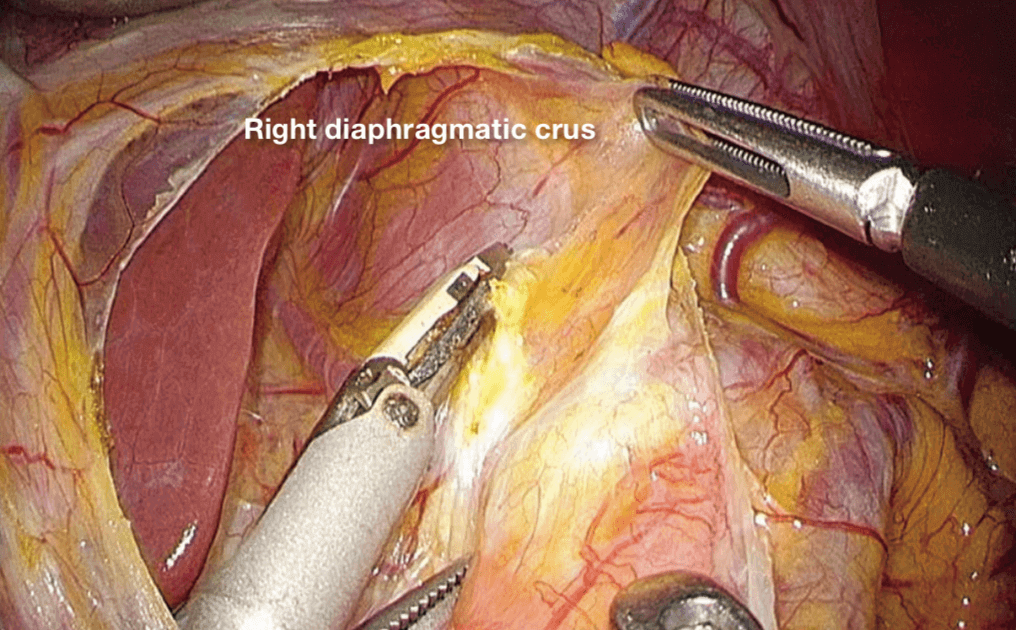
Thereafter, dissection of the retroperitoneum is advanced along the right diaphragmatic crura, and the No. 1 lymph nodes are dissected to the upper limit rostrally.
Dissection occurs on the anterior surface of the stomach in a somewhat caudal to rostral direction along the superior branch of the left gastric artery.
The dissection is stopped before the posterior surface of the stomach is reached.
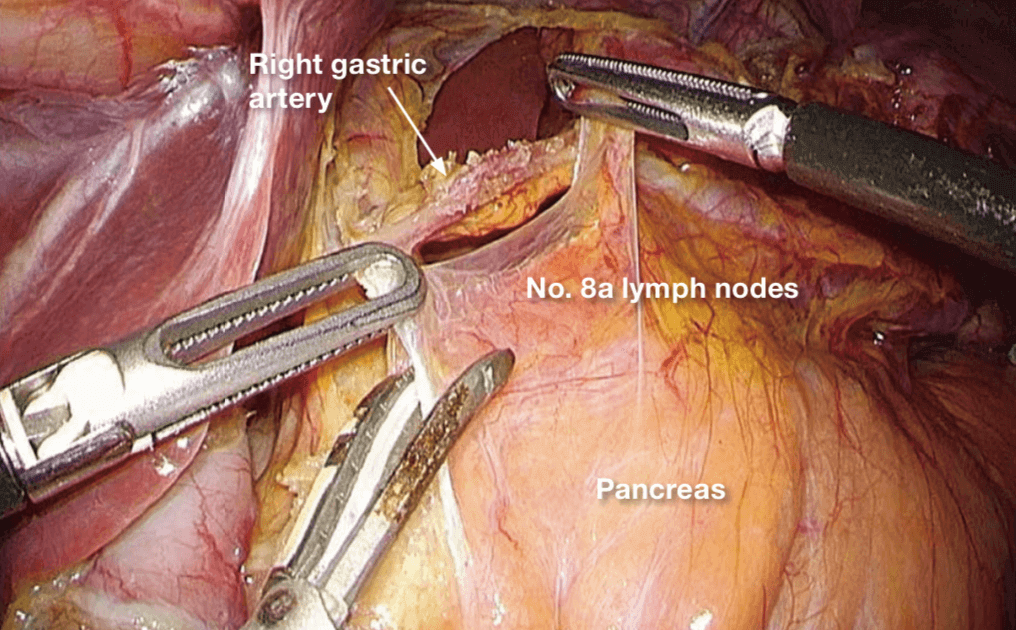
5.Dissection of lymph nodes along the superior pancreaticmargin (No. 8a, 5, and 12a lymph nodes)
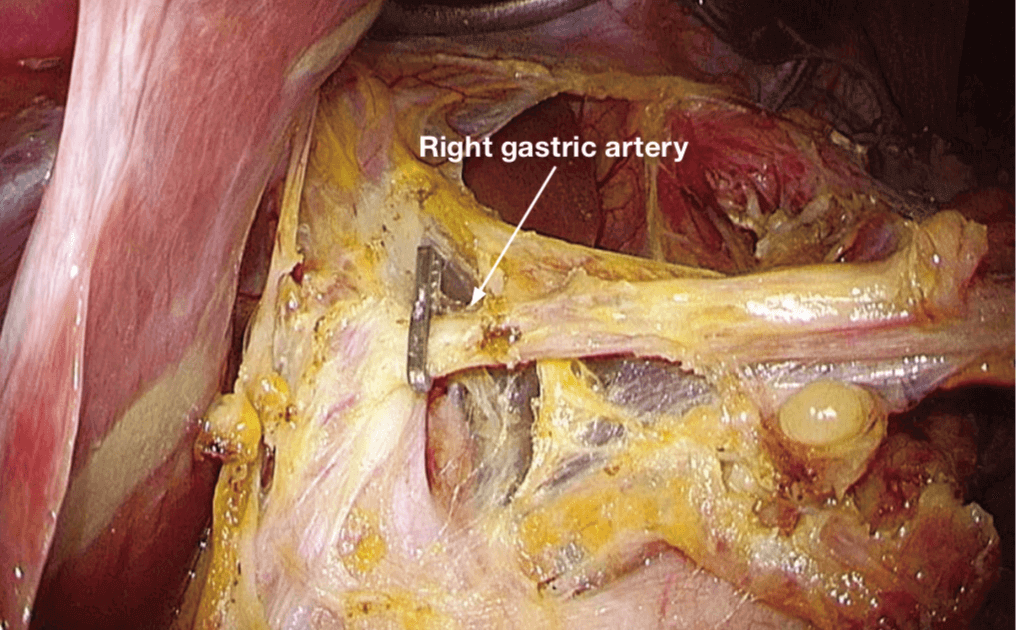
When the surgeon starts dissection from the superior pancreatic margin, the assistant swipes the gauze on the edge of the pancreas with his/her left hand, grasps (right hand) the right gastric artery and exposes the area. This step is performed at several institutions. We perform a similar maneuver, but the assistant grasps (right hand) the peritoneum near the No. 8a lymph nodes and applies traction. The peritoneum is cut at the superior pancreatic margin.
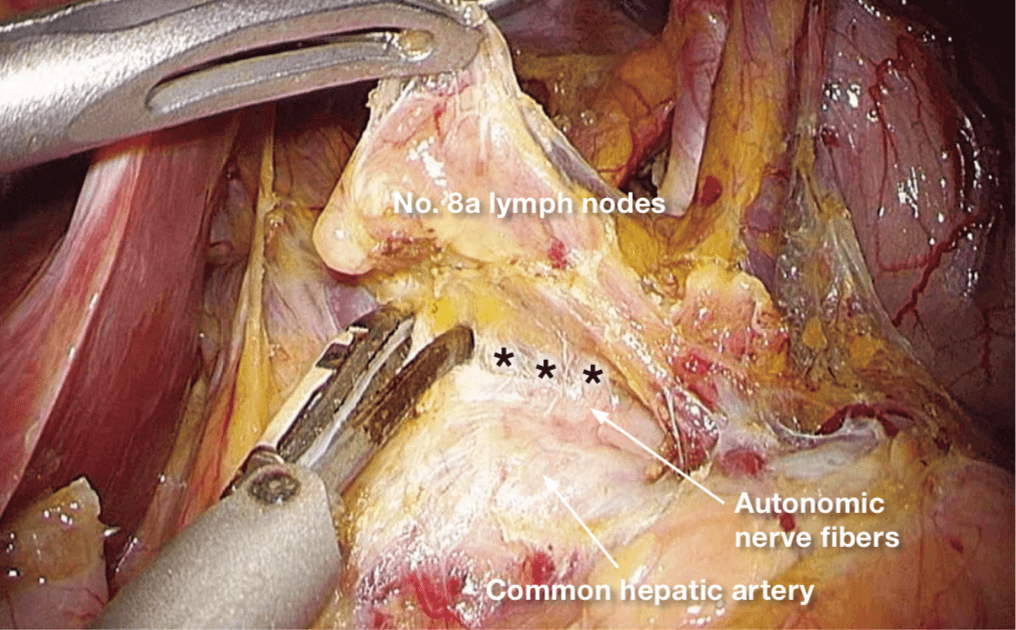
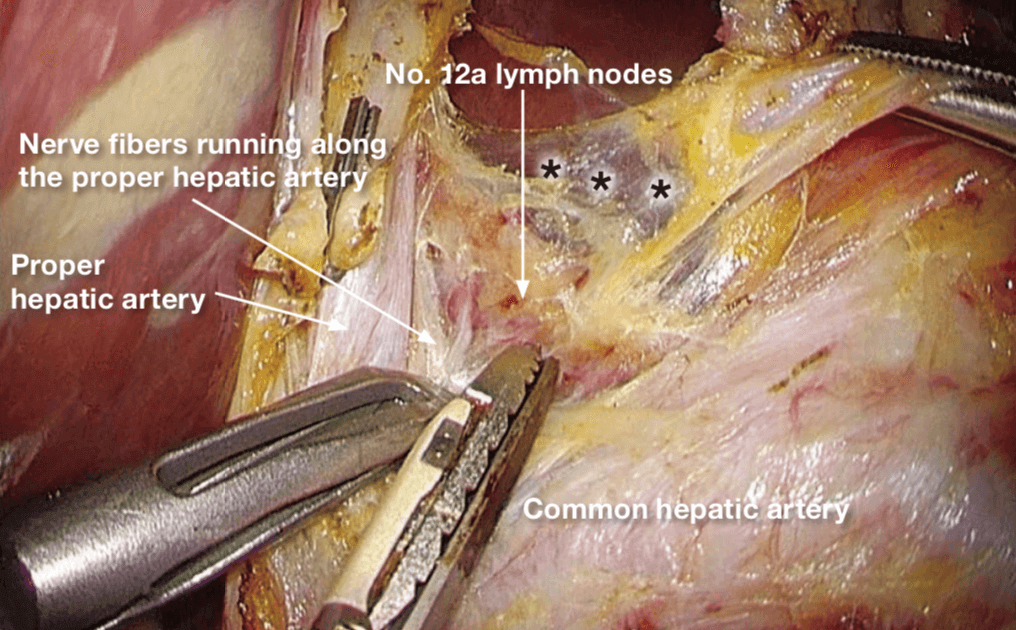
The No. 8a lymph nodes are elevated, and the connective tissue layers are carefully separated in a dorsal direction on the anterior surface of the common hepatic artery. Loose connective tissue (***) can be confirmed between the dissected tissues and the nerves. This is the outermost, and correct, layer of dissection.
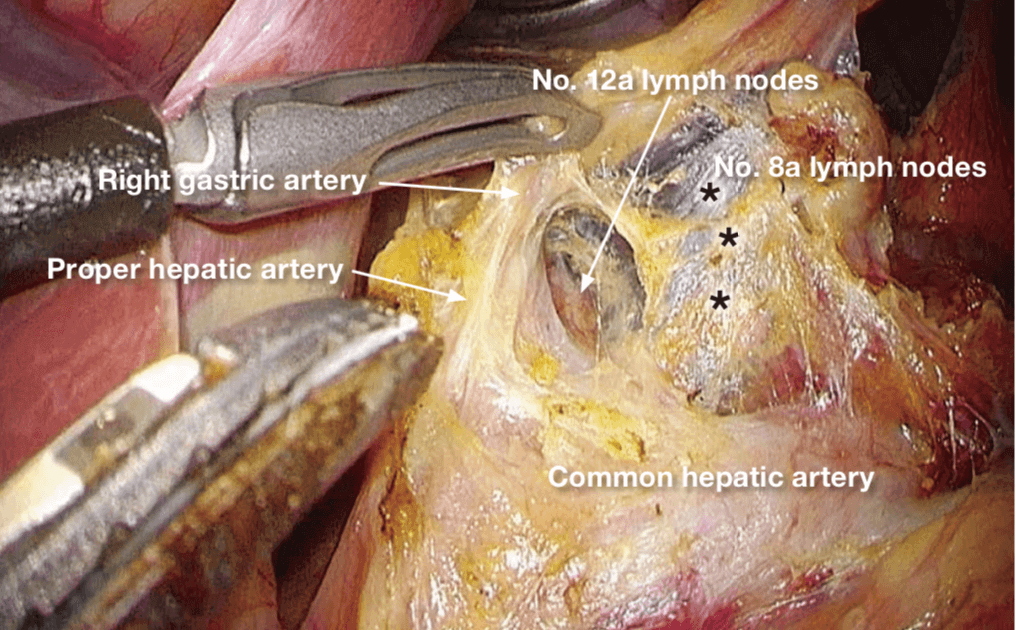
The dissection is advanced from the common hepatic artery along the lateral surface of the proper hepatic artery and vein and is continued until the lateral surface of the right gastric artery is sufficiently exposed. The No. 8a lymph nodes will be enclosed in a thin layer of peritoneum (***). To avoid injuring the No. 8a lymph nodes, it is important to perform the following No. 12a lymph node dissection.
After the right gastric artery Is transected and clipped, the resected side is cut, and the No. 5 lymph nodes are dissected.
The assistant applies (left hand) traction to the peritoneum (***) covering the No. 8a lymph nodes, and the surgeon grasps (left hand) and applies traction to the nerves that run parallel to the proper hepatic artery. The No. 12a lymph nodes lie dorsal to the proper hepatic artery and are removed without traction being applied; therefore, dissection is advanced along the outermost layer.
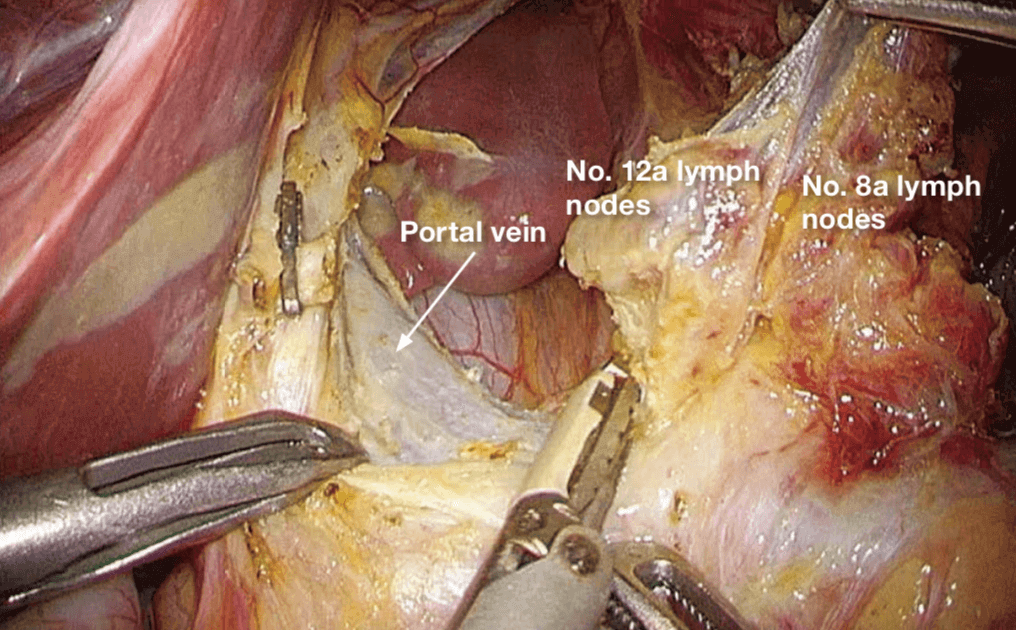
The portal vein is confirmed, and the No. 12a lymph nodes are dissected along the left side of the portal vein. Formerly, we used a medial approach, and the No. 12a lymph nodes were dissected after the left gastric artery was transected, but we now dissect the nodes after transecting the right gastric artery.
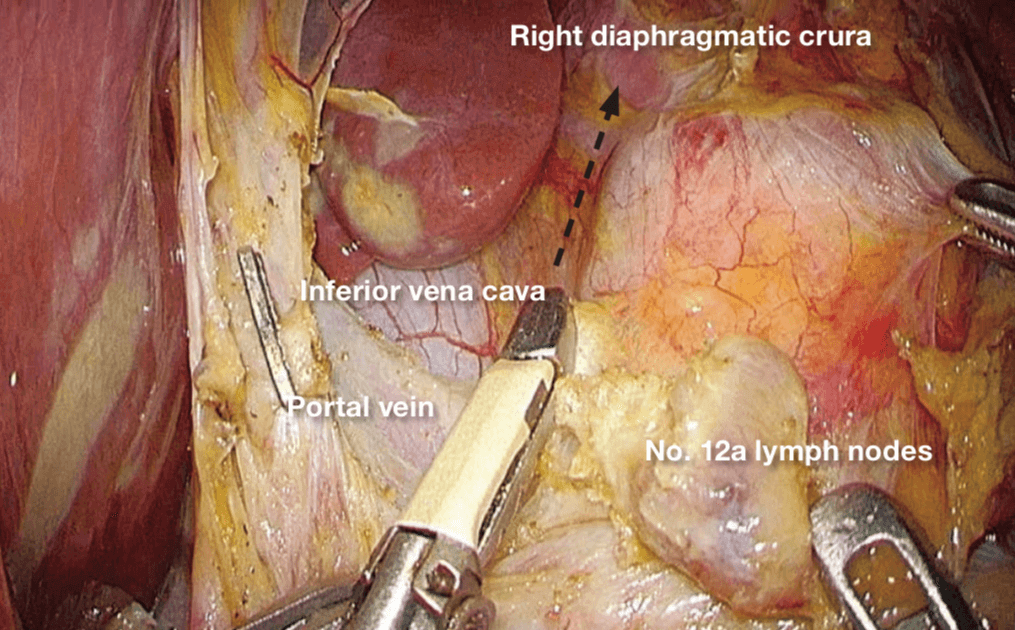
The assistant applies traction (both hands) to the dissected No. 8a and No. 12a lymph nodes, and the peritoneal incision at the site of No. 12a lymph node dissection is continued to the right diaphragmatic crus. Care must be taken to avoid the inferior vena cava. Furthermore, the dissected tissues are bluntly dissected in a lateral to medial fashion, i.e., from the inferior vena cava to the aorta. In doing this, care must be taken to prevent injury to the inferior right phrenic artery. By performing this step, good mobility of the No. 9 lymph nodes that lie to the right of the celiac artery is obtained. We call this the lateral approach, and it precedes the medial approach.
6.Lymph node dissection along the superior pancreatic margin(No. 9 and No. 7 lymph nodes to the right of the celiac artery)
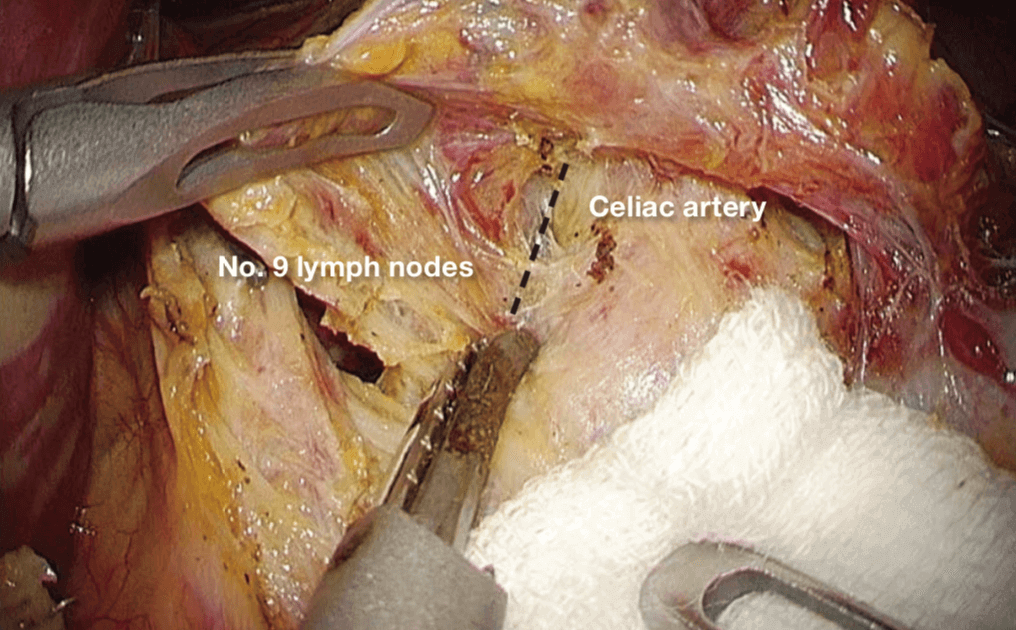
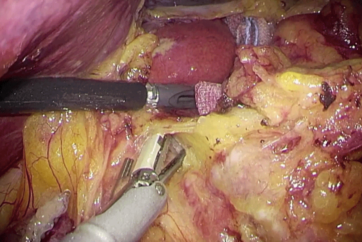
The assistant applies traction (right hand) in a direction ventral to the gastropancreatic fold and then “rolls” (right hand) the pancreas using gauze, exposing the area. The outermost layer of the anterior surface of the common hepatic artery (black dotted line) is stretched by dissection between the celiac artery and the No. 9 lymph nodes via a medial approach.
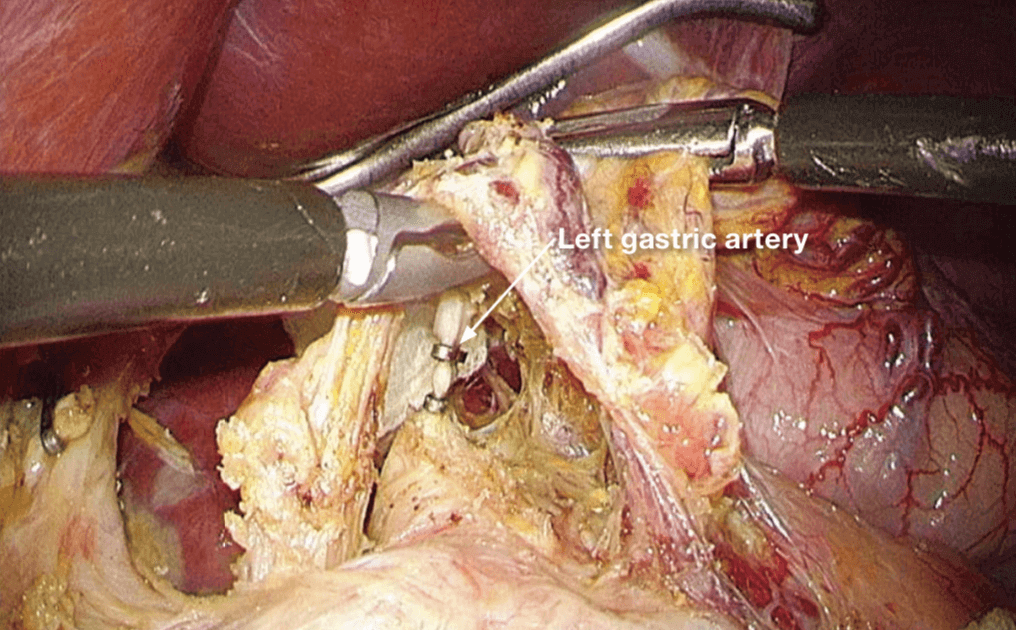
After the outermost layer to the left and right of the left gastric artery is dissected, the root of the left gastric artery is transected.
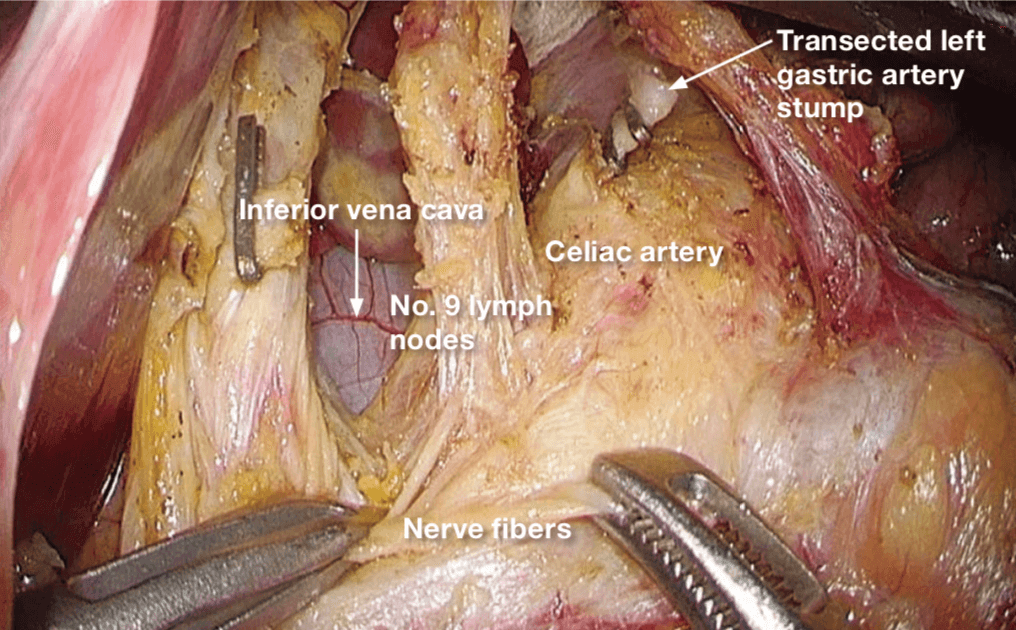
The assistant grasps the nerve fibers around the common hepatic artery in two places and, moving caudally, applies traction to the No. 9 lymph nodes for dissection by the surgeon in a ventral direction, and the area is exposed.
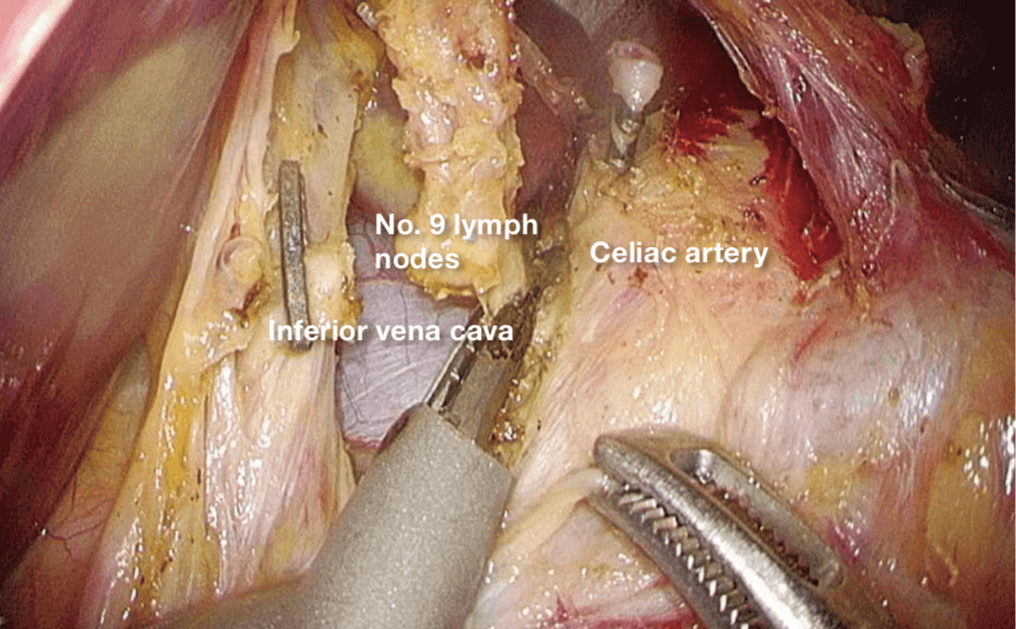
The No. 9 lymph nodes, which are continuous with the lymph nodes between the great vessels, are cut away, and dissection is completed.
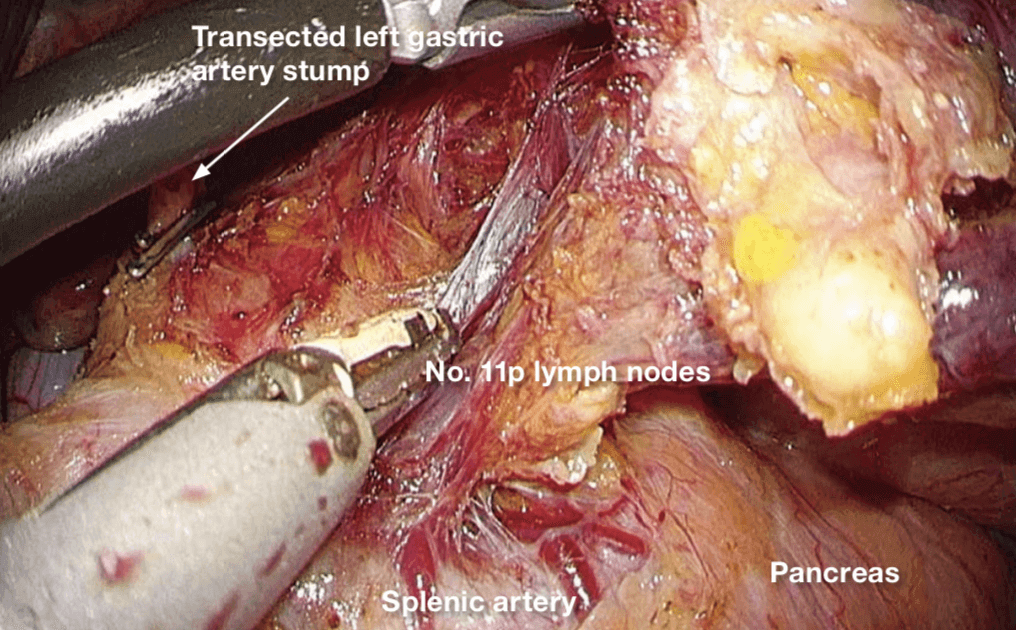
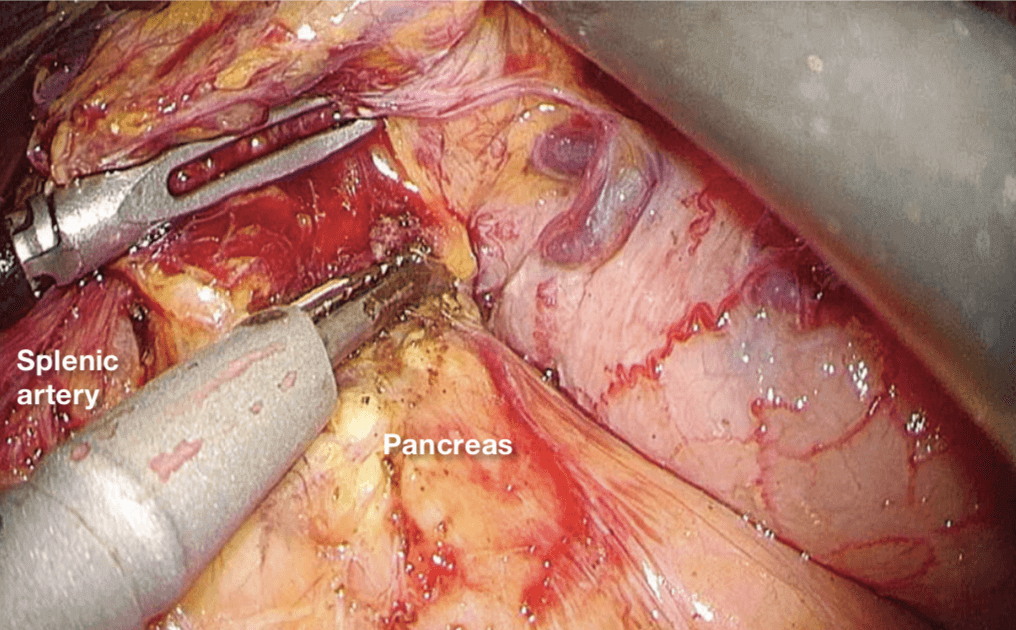
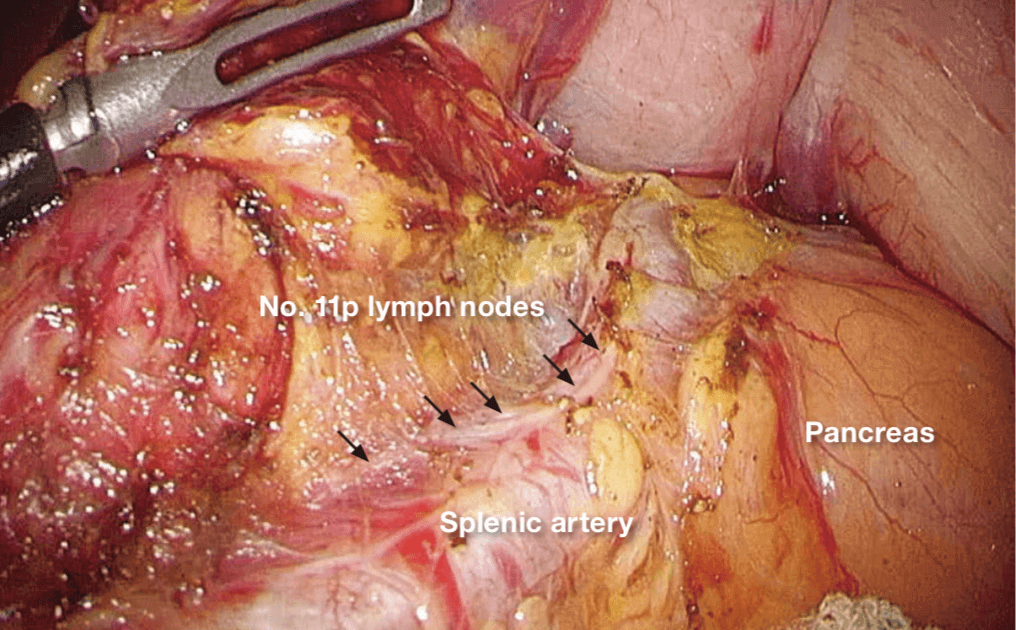
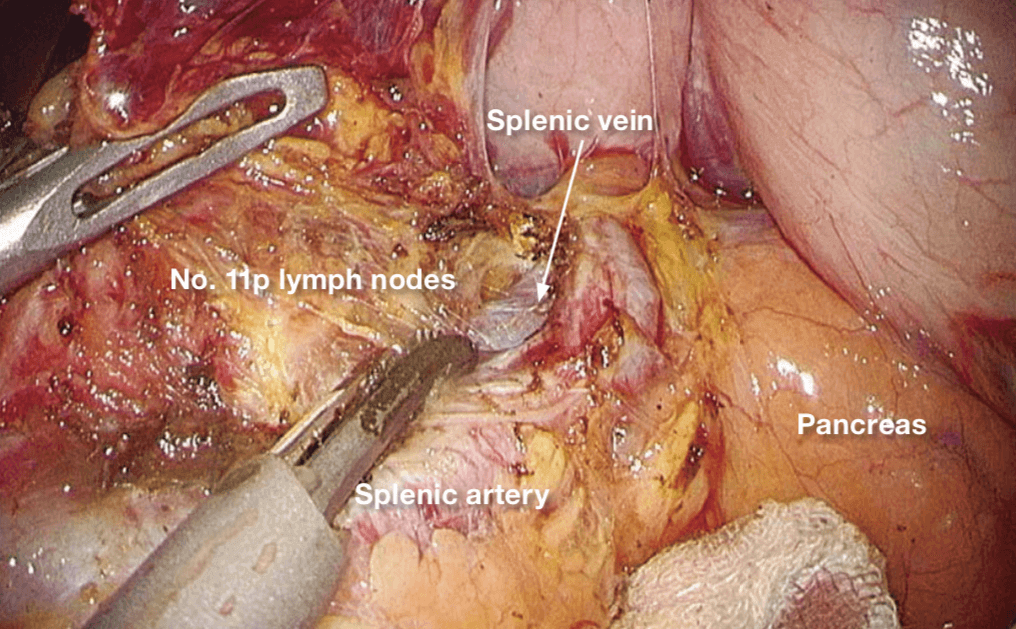
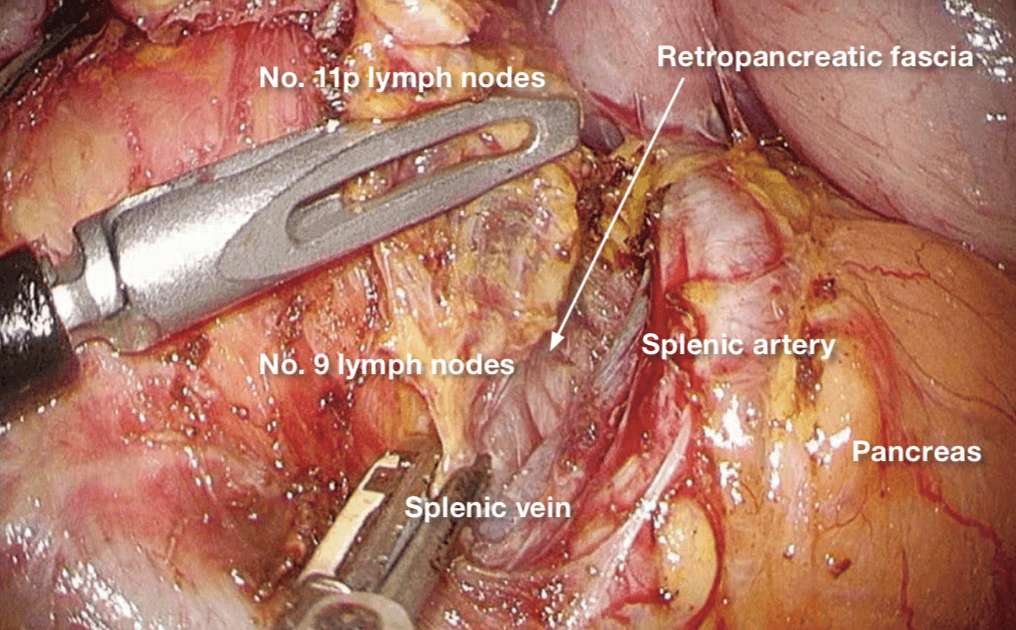
7.Lymph node dissection along the superior pancreaticmargin (No. 9 and No. 11p lymph nodes)
The dissected tissue contains the No. 11p lymph nodes, and this is separated from the anterior lobe of Gerota’s (prerenal) fascia, further mobilizing the dissected tissues.
The surgeon grasps the plank-shaped dissected tissue, including No. 11p lymph nodes, and applies traction, and the assistant elevates (right hand) the stomach, using the left hand to “roll” the pancreas with gauze and expose the area. Thereafter, the superior pancreatic margin is cut, and dissection is advanced until the nerve fibers (see image 7C) that run cranially from the anterior surface of the splenic artery are confirmed.
The surgeon confirms the comparatively thick nerve fibers rostral to the splenic artery. If the dissection has been completed, the method for exposing the area should be changed. Up to this point, the assistant has used the right hand to hold the stomach and apply traction in a ventral direction, but the assistant now uses both hands to hold the gauze and perform the so-called rolling of the pancreas at two points. The surgical field that includes the cranial side of the splenic artery is widely exposed. If exposure of the area is insufficient, the assistant does not use gauze to “roll” the pancreas but instead applies direct traction to the nerve fibers on the cranial side of the splenic artery and “rolls” the arteries. In the case pictured here, we were able to secure an adequate visual field by rolling the pancreas.
Dissection of the dorsocephalic splenic artery is advanced, and the No. 11p lymph nodes are dissected while the pancreatic parenchyma or splenic vein is exposed.
Finally, the No. 9 lymph nodes are dissected most deeply in the area of the lateral aortic lymph nodes to the left of the celiac artery, and dissection of the No. 9 and No. 11 lymph nodes is completed.
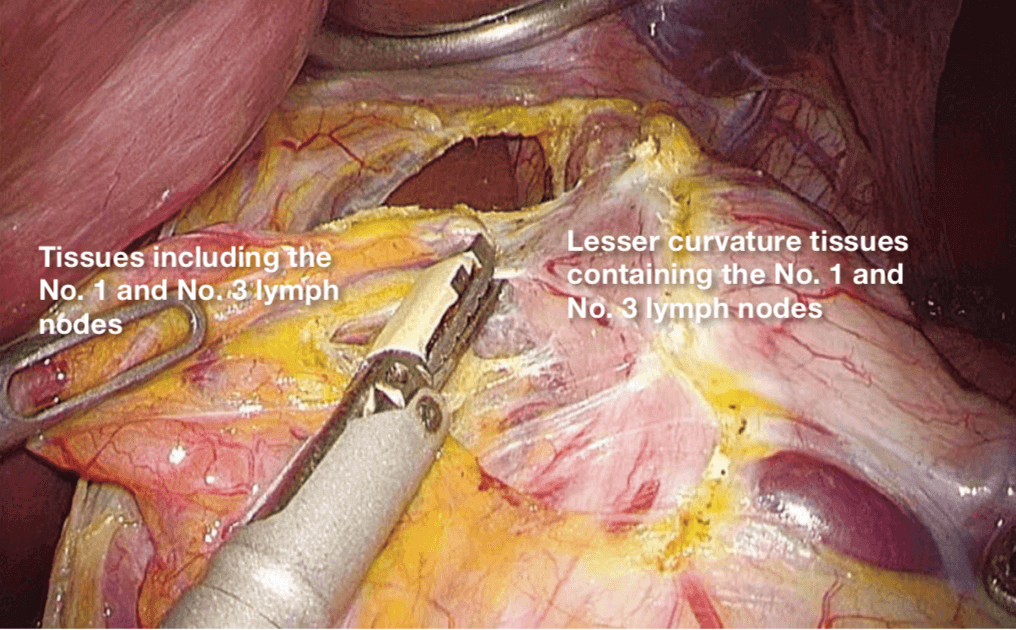
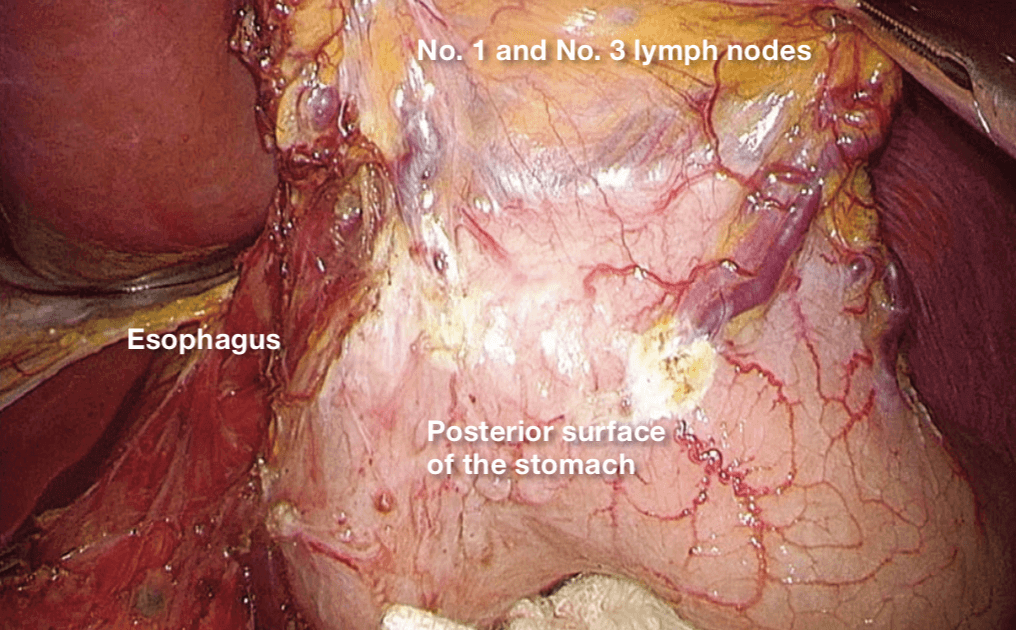
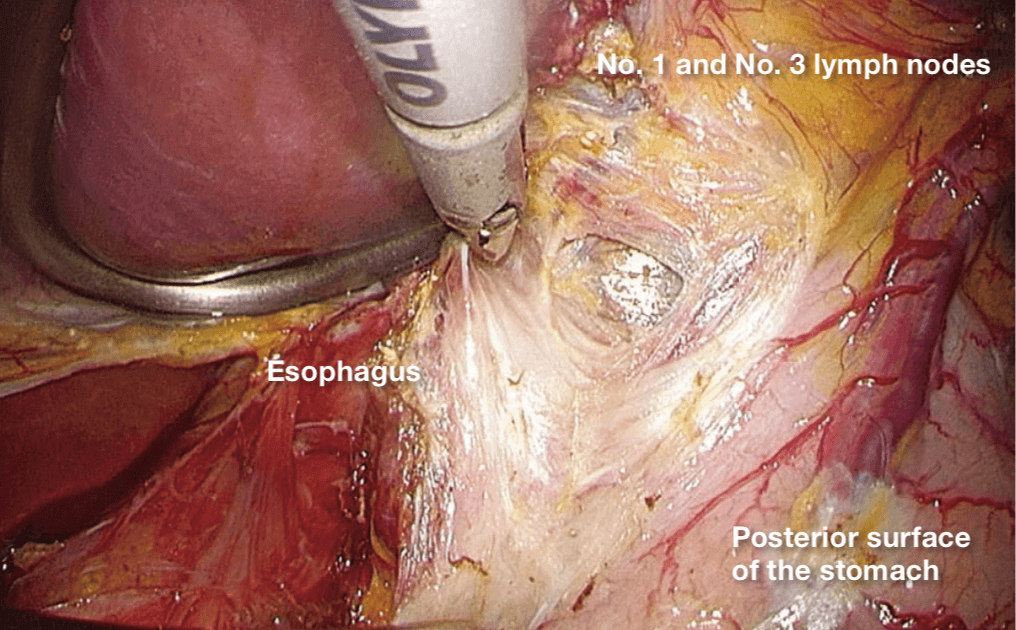
8.Dissection of No. 1 and No. 3 lymph nodes on the posterior surface of the stomach
The assistant uses both hands to grasp the tissues containing the No. 1 and No. 3 lymph nodes and applies traction ventrally to expose the area.
The surgeon holds the posterior surface of the stomach while resecting the tissues for dissection from the lesser curvature of the stomach.
Images of completed D2 lymph node dissection performed during distal gastrectomy
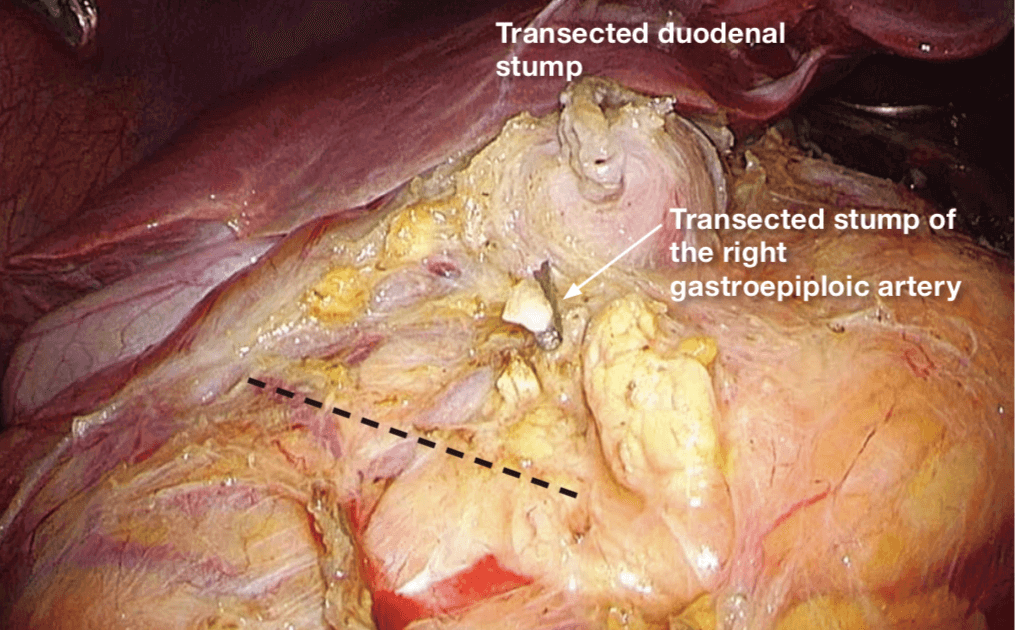
Image of a completed No. 6 lymph node dissection. The fusion fascia, indicated by the black line, is cut. This line is the inferior margin of dissection.
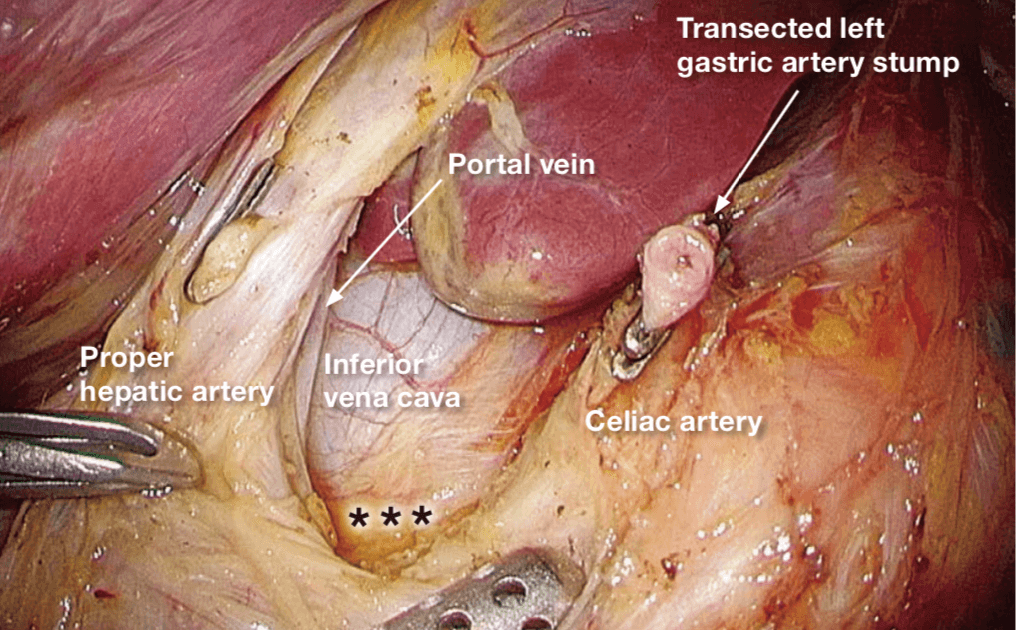
Image of completed lymph node dissection along the superior pancreatic margin on the right side of the celiac artery. Dissection of the No. 9 lymph nodes is at the level of the inferior vena cava, and it is performed carefully in the deeper layers (***) that are continuous with the paraaortic lymph nodes that lie between the great vessels.
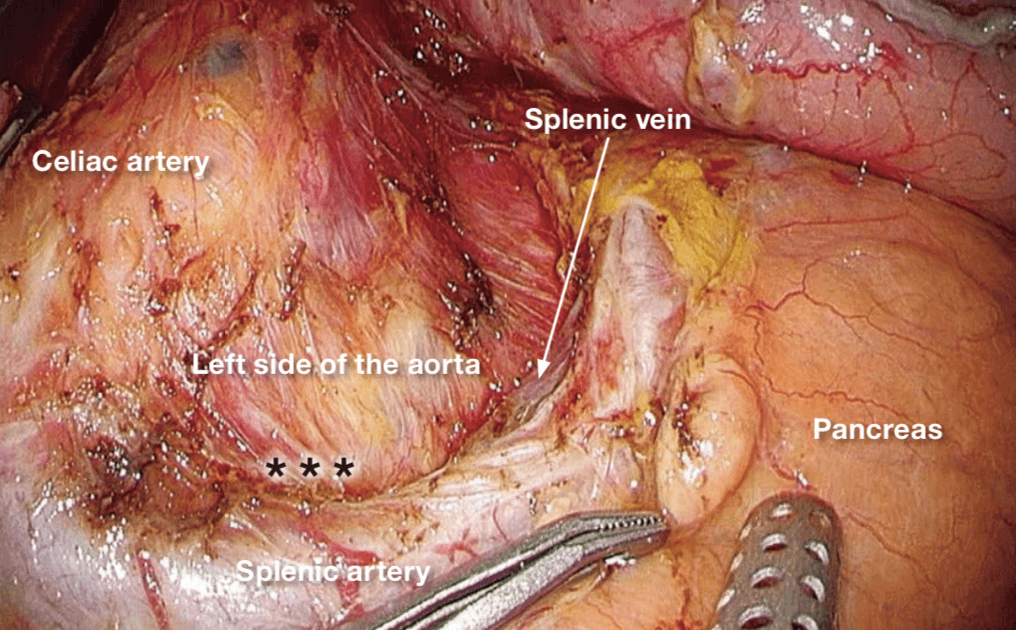
Image of completed lymph node dissection along the superior pancreatic margin on the left side of the celiac artery. Dissection of No. 9 lymph nodes is performed carefully in the deeper layers (***) that are continuous with the paraaortic lymph nodes that lie between the great vessels.
Conclusion
Preventive D2 lymphadenectomy performed during laparoscopic distal gastrectomy has become a standard procedure. Going forward, we will need to act economically by shortening the operation time in addition to ensuring safety. Even from this perspective, the THUNDERBEAT™ device is an exceptionally useful energy device.
September 2014
Dr. Ichiro Uyama
Chairman, Department of Surgery, Upper GI Division
Fujita Health University
- Content Type