Author
Dr. Hitoshi Niikura, Associate Professor and Department Head, Gynecology, Medical Sciences Reproductive and Developmental
Medicine Gynecology, Tohoku University Graduate School of Medicine, and Gynecology Department, Tohoku University Hospital
Biography
Graduated from Tohoku University in 1988. Became associate professor in the Gynecology Department at Tohoku University Hospital in April 2012. Dr. Niikura has been involved in minimally invasive surgery over the years, particularly sentinel lymph node navigation surgery for gynecologic cancer, and he currently aims to achieve minimal invasive surgery by integrating navigation surgery with laparoscopic surgery and robot-assisted surgery.
Introduction
Biopsy of sentinel lymph nodes for endometrial cancer is recommended under category 2A as a procedure for detecting lymph node metastasis in the NCCN Guidelines, 2018 version, and its utility has been recognized overseas. In Japan, although it is a procedure that merits consideration, it is recommended to be carried out as a clinical study. The cervix is often selected as the location for administering the tracer for endometrial cancer, and the combined use of a radioactive isotope (RI) with a dye (e.g. patent blue) has had the highest identification rate of all tracers used until now, as well as being highly safe. More recently, data from meta-analysis and multicenter prospective studies has also appeared, showing that the use of ICG as a fluorescent dye is more effective. As it is also compatible with laparoscopic surgery and robot-assisted surgery, ICG is expected to be the main tracer in the future.
Laparoscopic Sentinel Lymph Node Biopsy for Endometrial Cancer Using IR Observation
In our department, we have recently been identifying sentinel lymph nodes laparoscopically using ICG together with the RI we had been using before.
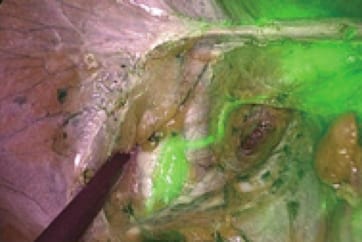
Using IR observation, the lymphatic ducts are clearly shown, and lymph flow is easier to ascertain than it is with dye, so it is particularly convenient for laparoscopic surgery.
Currently, in our department, we are performing a clinical study that consists of sentinel lymph node biopsies targeting G1 and G2 endometrioid carcinoma as the histological type, with lesions localized to the uterine body, and estimated myometrial invasion not exceeding ½. Mapping is performed on both sides, and systematic lymph node dissection is omitted in cases where intraoperative frozen section diagnosis is metastasis-negative.
For RI, 99mTc-phytate is injected into the cervix in four locations on the day prior to surgery.
For ICG, a concentration of 0.5 mg/mL, 4 mL in total, is administered to the cervix during surgery, prior to the opening of the retroperitoneal space.
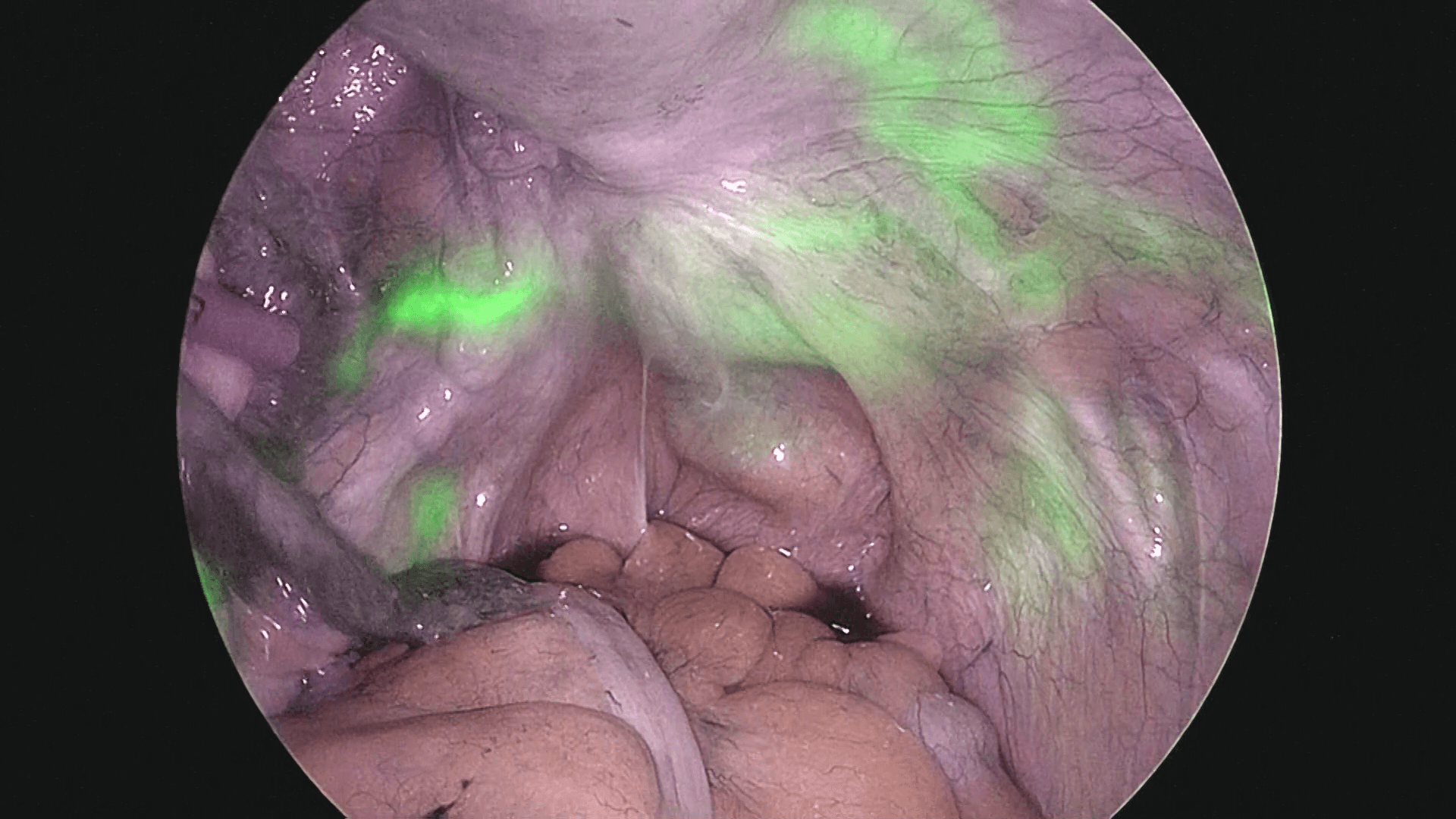
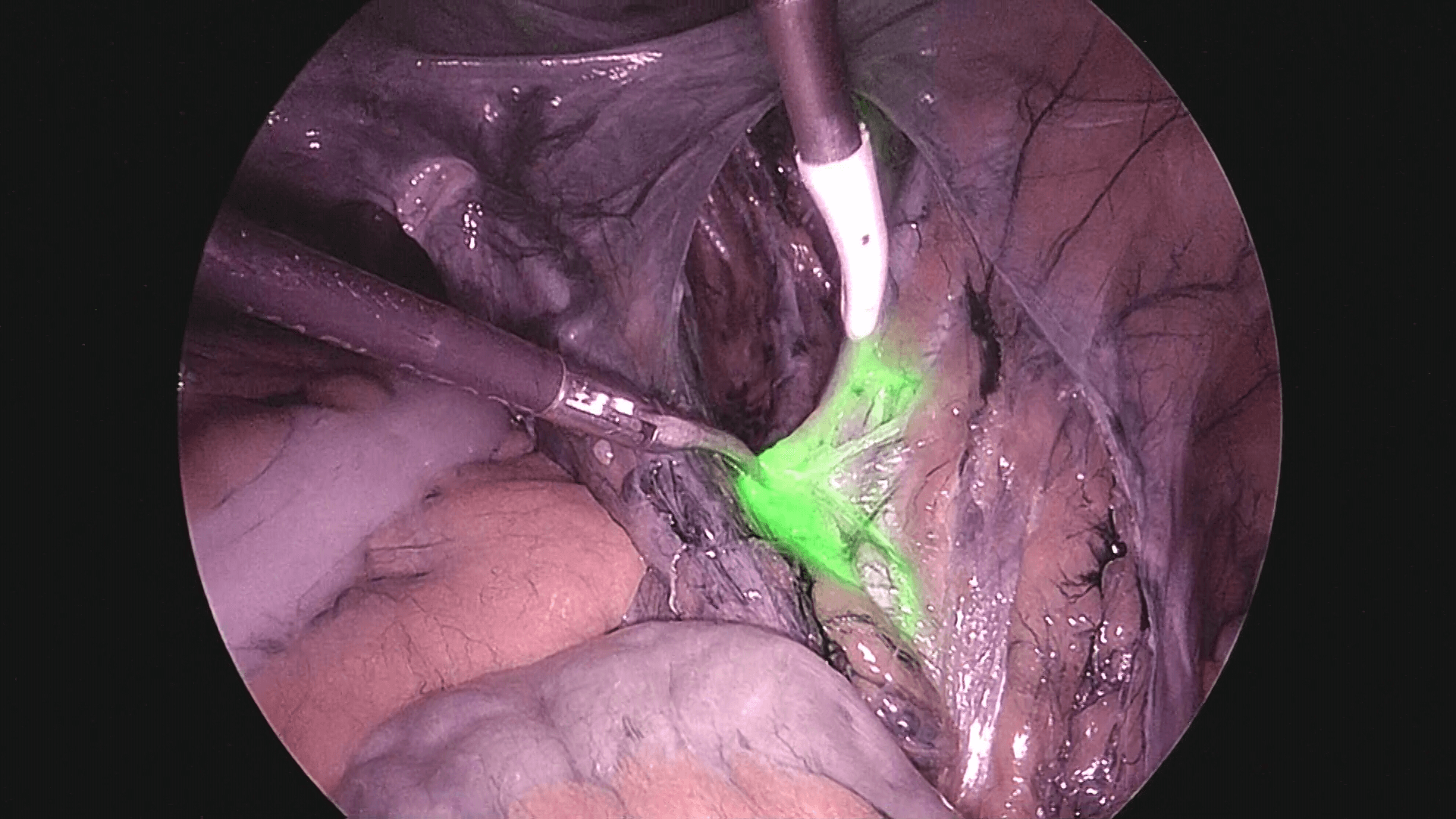
After observing the interior of the abdominal cavity with the laparoscope, a washing cytology sample is taken, and after ICG is administered at the 8-o’clock and 10-o’clock sites of the cervix, 1 mL each, the right retroperitoneal space is opened, and sentinel lymph nodes in the right pelvis are identified. Next, ICG is administered to the 2-o’clock and 4-o’clock sites of the cervix similarly, 1 mL each, and then the left retroperitoneal space is opened. The flow of ICG across the peritoneum to the periphery is readily apparent (photos 1 and 2), so after confirming that flow, the retroperitoneal space should be opened.
Using the method described above to administer tracers to the left and right sides separately, it is possible to identify sentinel lymph node location for each side individually.
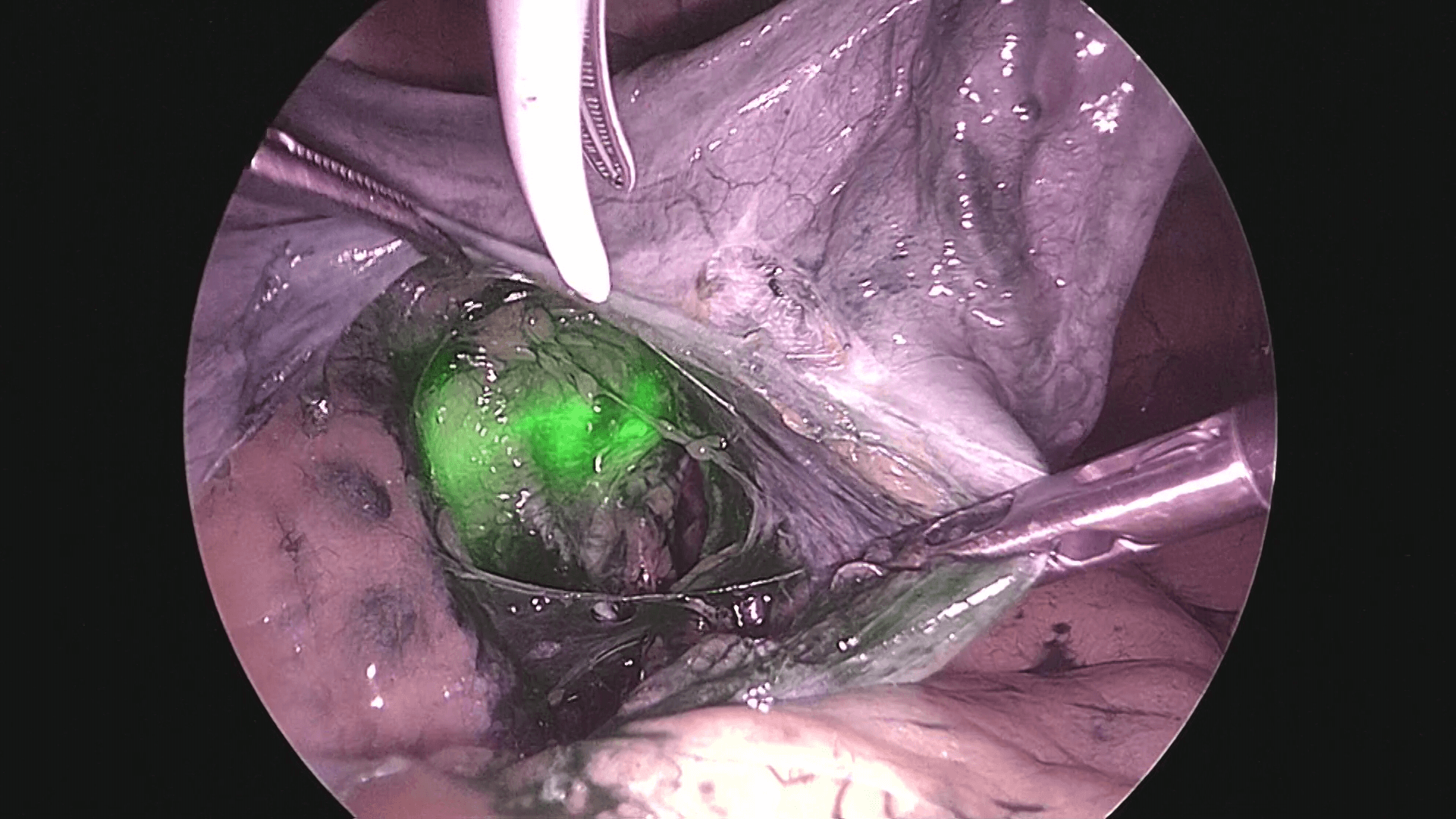
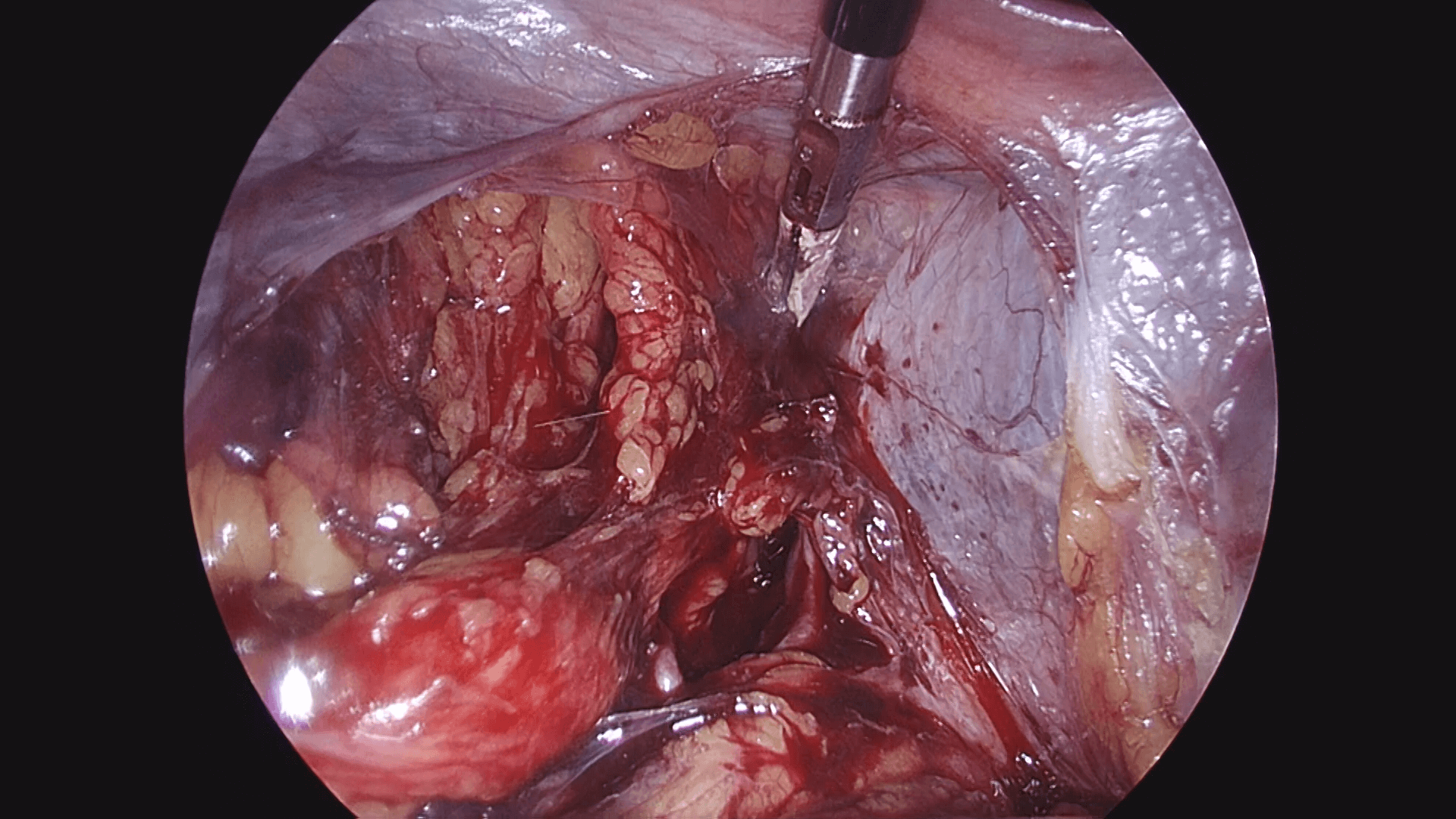
As shown in photo 3, the external iliac nodes are easy to remove, but in the case of obturator nodes as shown in photo 4, it is safer to open the pararectal space and paravesical space, visually confirming the obturator nerve before removal.
When we use VISERA ELITE II, a new IR observation system, to check fluorescent dye, its comparatively complete field of view under bright conditions also makes it possible to perform normal separation, dissection, etc., without delaying surgical operations (photo 5: IR observation mode and white light mode).
When opening the retroperitoneal space, it is important to consider the separation layers and to proceed in a manner that prevents damage to the lymphatic ducts. Additionally, by biopsying the target sentinel lymph nodes while sealing the lymphatic ducts, there is no lymph leakage and ICG diffusion does not disturb the field of view.
After the biopsy, the lack of residue is confirmed by the lack of reaction with the radioactive isotope (photo 6).
Unlike blue dye, when performing the required bladder dissection and other procedures during uterus removal, there is no visual penetration of the dye into the cervix making it difficult to see, so surgery can be performed easily as usual.
Suggestions and Cautions
The main lymph flow detected during cervical administration consists of outward flow along the obturator artery, external iliac vein, and common iliac nodes; and inward flow along the internal iliac vein and external sacral nodes. If a radioactive isotope is not also used, careful observation of the lymph flow is required in order not to miss the inward flow. If detection is weak, it is possible to add more ICG.
Lastly, as of April 2018, it should be noted that the use of ICG for fluorescent imaging to identify sentinel lymph nodes in endometrial cancer is currently off-label use in some countries including in Japan.
- Content Type