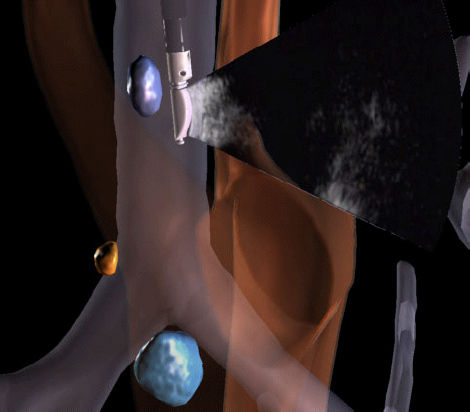
EBUS-TBNA: Procedure and Landmarks
Authors:
Prof. Felix JF Herth, MD, PhD, DSc,Mark Krasnik, MD,
Thoraxklinik, University of Heidelberg, Germany Rigshospitalet, Copenhagen University Hospital, Denmark Gentofte Hospital, Copenhagen University Hospital, Denmark
Source:
DVD-ROM ‘Endoscopic Ultrasound – Diagnostics and Staging of Lung Cancer’, Olympus Europa SE & Co. KG, 2013
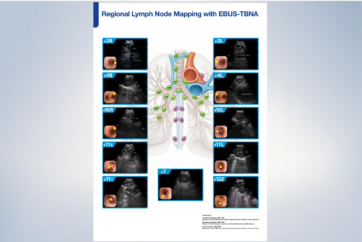
This article aims at providing orientation in finding lymph node stations during EBUS-TBNA. The underlying nomenclature is following the 7th edition of the TNM classification of malignant tumours as proposed by IASLC. With reference to the primary lung tumour, the required N-staging has to follow the N3 → N2 → N1 rule, assuring that overstaging or spreading of tumour cells is avoided.
Nodal staging in case of a primary tumour in the left lung follows this sequence:
11R → 10R → 4R → 2R → 2L → 3p → 4L → 7 → 10L → 11L
Nodal staging in case of a primary tumour in the right lung follows this sequence:
11L → 10L → 7 → 4L → 2L → 2R → 3p → 4R → 10R → 11R
The sequence of lymph node stations in this article follows the N-staging sequence to be used in case of a primary tumour in the left lung.
Although reachable by endoscopic ultrasound the proposed anatomic borders of lymph node station 1 (Low cervical, supraclavicular and sternal notch nodes) cannot be recognized with endoscopic ultrasound. Nodes of LN Station 1 are situated in extrathoracic location, an endoscopic approach is technically difficult and uncomfortable for the patient. Positive staged LN1 define a N3 stage disease.
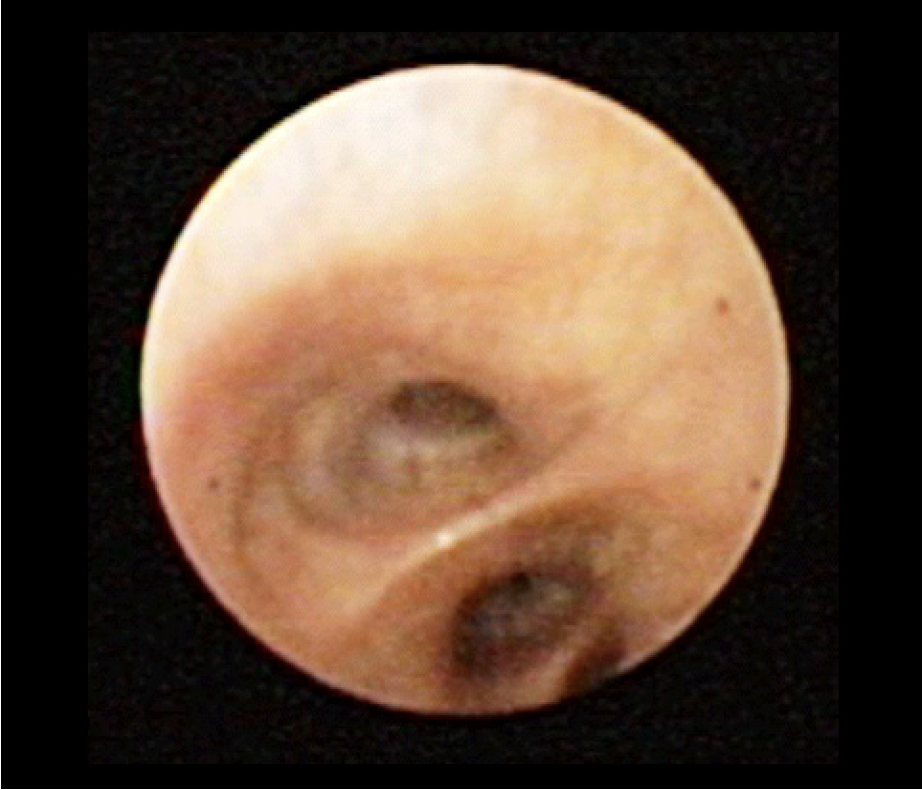
To start the endoscopic staging procedure, the endoscope is introduced to the patient following the trachea. The posterior part of the trachea is vertically structured (resembles long vertical plies) easy to distinguish from the arch shaped cartilage structure (horizontal support of the bronchial tree). The trachea then separates in two main bronchi (left and right), the intersection is the main carina.
The main carina in conjunction with the structure of the trachea simplifies distinction of the left main bronchus and the right main bronchus. When in doubt, the right main bronchus is short and the opening to the right upper lobe is seen just after entering the right main bronchus.
By lifting the distal end of the endoscope and a slight turn to the right the endoscope slides into the right main bronchus. Verification for successful insertion of the endoscope to the right main bronchus is obtained from the view to the right upper lobe which branches off the right main bronchus only a few (2-3) centimetres after the main carina was passed.
Having visualised the right upper lobe — but not entering it — and after straightening the endoscope, the intermediate bronchus is followed distally. The intermediate bronchus is unique for the bronchial structure of the right side of the body — here the middle lobe and the lower lobe branch off.
The endoscope follows the intermediate bronchus until – due to the decrease of diameter of the tubular system of the bronchial tree – it cannot be advanced any further. This is usually the case at the level beyond the subcarina which branches off into middle lobe and right lower lobe (in case of enlarged airways e.g. chronic bronchitis the endoscope might be advanced further down beyond the carinas of the basal group).
The area beyond the carina at the 2-4 o’clock position is congruent with lymph node station 11R (Interlobar nodes). The area of lymph node station 11R marks the starting point for nodal staging in case of a primary lung cancer in the left lung. The underlying question to answer is, whether positive tissue samples prove a N3 stage disease. Lymph node position 11 is in most cases the most distant accessible node for EBUS-TBNA.
NOTE: With the 7th edition of the TNM nomenclature (IASLC) an optional division between 11s and 11i on the right side was proposed. The former indicate the nodes between upper lobe and intermediate bronchus, the latter are situated in between middle and lower lobe. Ultrasound landmarks are not available, use the endoscopic view to identify the relevant bifurcation.
The endoscope is slightly withdrawn just beyond the entrance to the right upper lobe. The endoscopic image shows the area of the subcarina dividing into right upper lobe and intermediate bronchus.
After confirmation of the right placement the ultrasonic examination continues at the level of lymph node station 10R (Hilar nodes):
Any lymph node in this area would be expected at the 2 o’clock position.
The hilar nodes of station 10R are situated immediately adjacent to the mainstem bronchus but caudal to the inferior border of azygos vein. The inferior margin of station 10R is the interlobar region, a unique ultrasound landmark is missing. Use the endoscopic view to locate the secondary carina or the upper lobe split off which serves as a landmark of the lower border of 10R.
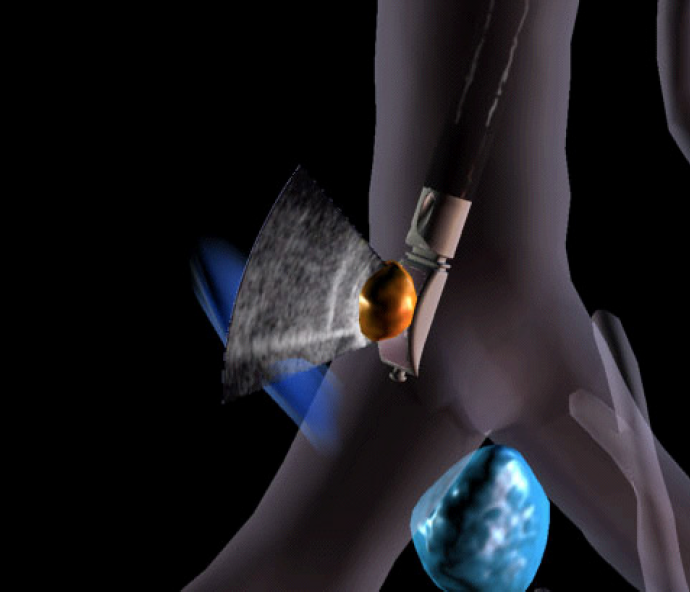
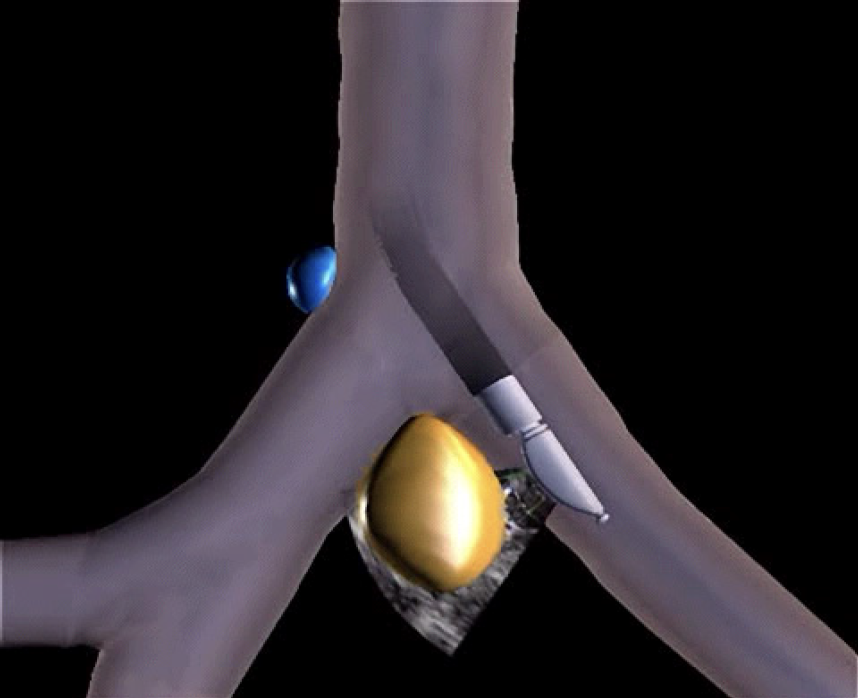
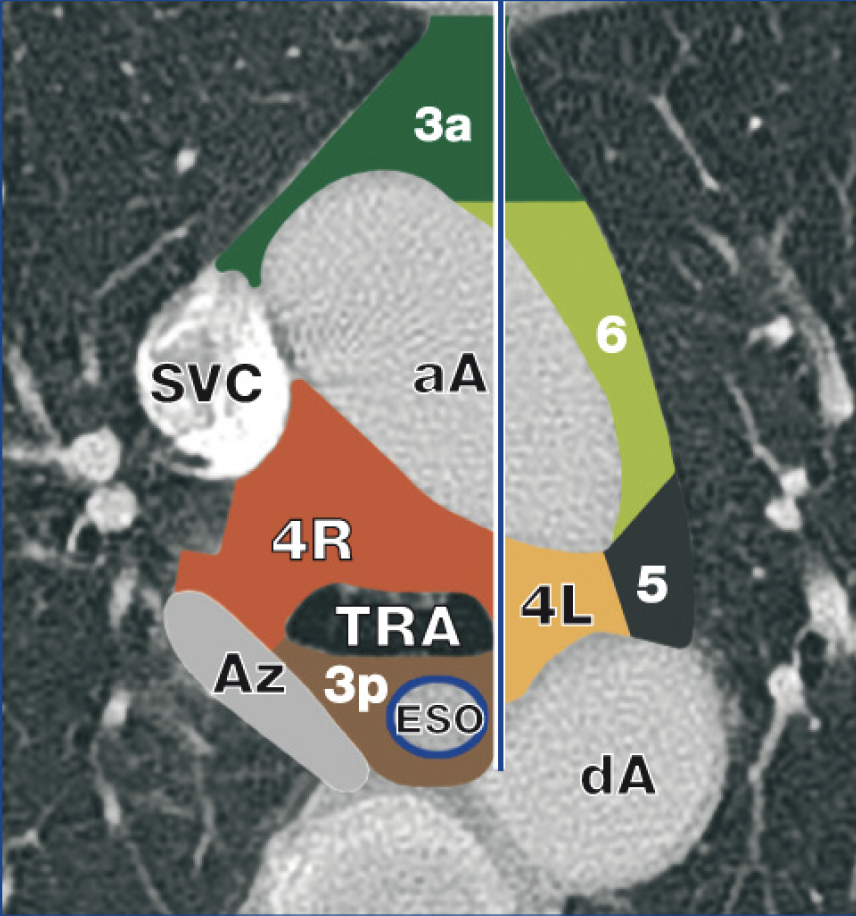
By withdrawing the endoscope just beyond the main carina and by turning it to the 3 o’clock position, lymph node station 4R (Lower paratracheal nodes) can be found. LN4R is close to the vena cava and azygos vein.
Lymph node station 4R includes right paratracheal nodes, and pretracheal nodes extending to the left lateral border of trachea.
Upper border: intersection of the caudal margin of the innominate vein with the trachea
Lower border: the lower border of the azygos vein
4R nodes are situated posterior to the superior vena cava or the ascending aorta. The inferior border of LN4R is defined by the lower border of the azygos vein.
NOTE: the 7th edition of the TNM classification by IASLC defines the midline between 4R and 4L at the left lateral border of the trachea.
The bronchoscope is pulled back beyond the carina. In the middle trachea the probe is pressed against the right tracheal wall at the 3 o’clock position, where we would expect lymph node station 2R (upper paratracheal nodes) of the right side of the body.
Upper border: apex of lung and pleural space and, in the midline, the upper border of the manubrium:
Lower border: intersection of caudal margin of innominate vein with the trachea:
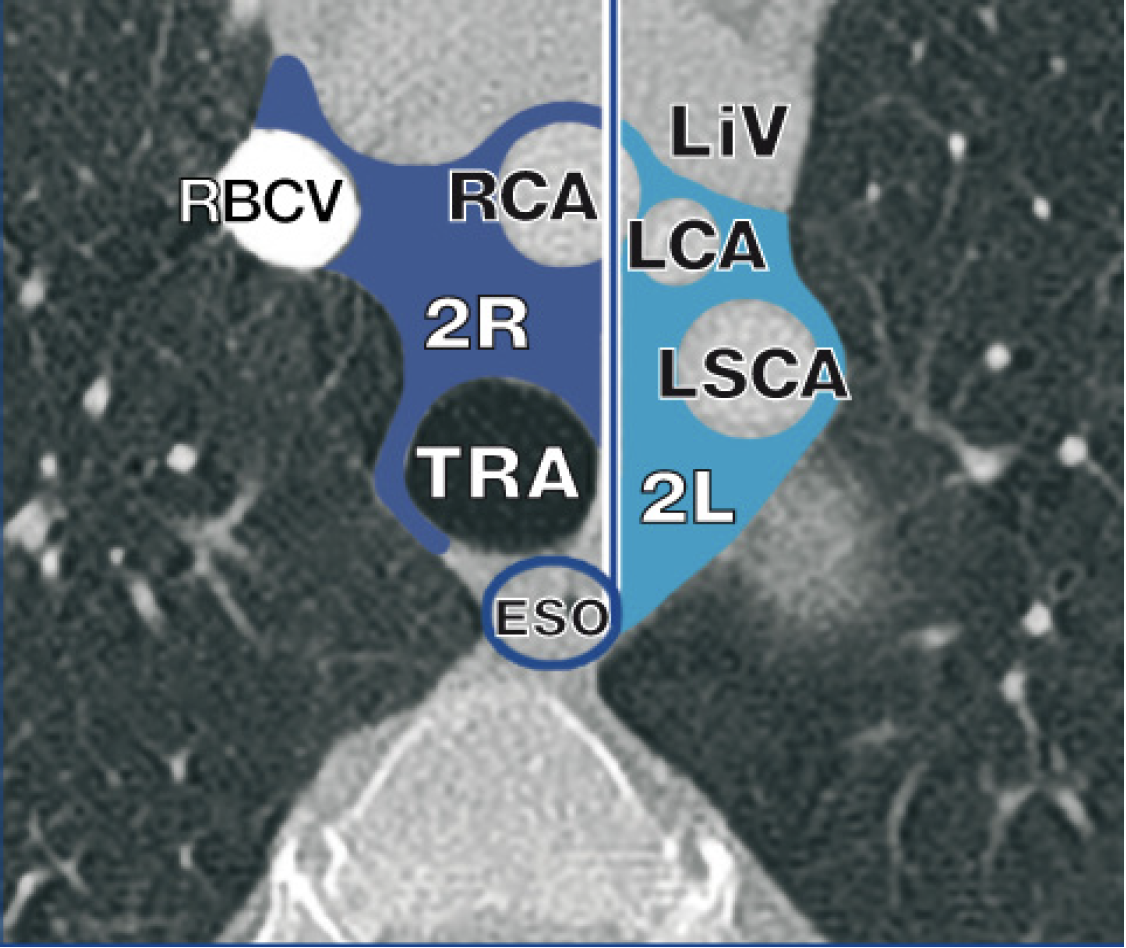
NOTE: the 7th edition of the TNM classification by IASLC defines the midline between 2R and 2L at the left lateral border of the trachea.
The inferior border of station 2R is the intersection of the caudal margin of the brachiocephalic vein with the right-sided border of the trachea.
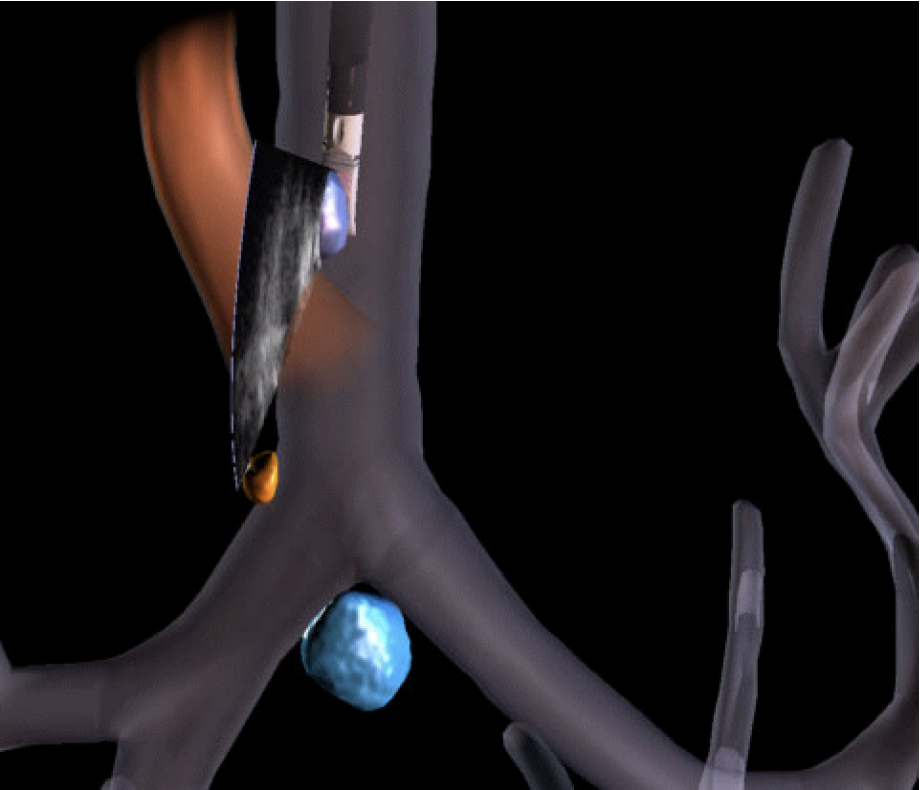
By turning the endoscope to the contralateral side of the tracheal wall to the 9 o’clock position, lymph node station 2L (Upper praratracheal nodes) can be scanned. This is the area above the aortic arch. Lymph node station 2L – assuming a primary tumour in the left lung – is as well as LN3p, LN4L, LN5 and LN7 are stations that could define a N2 stage disease.
Upper border: apex of the lung and pleural space in the midline, the upper border of the manubrium
Lower border: superior border of the aortic arch
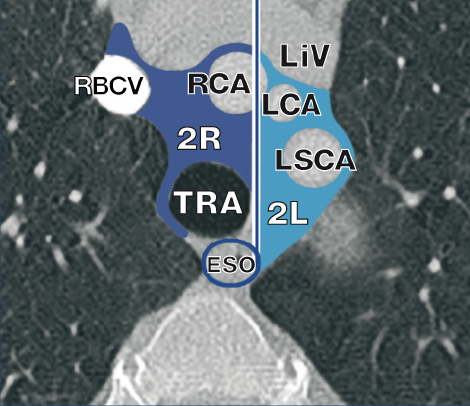
NOTE: the 7th edition of the TNM classification by IASLC defines the midline between 2R and 2L at the left lateral border of the trachea.
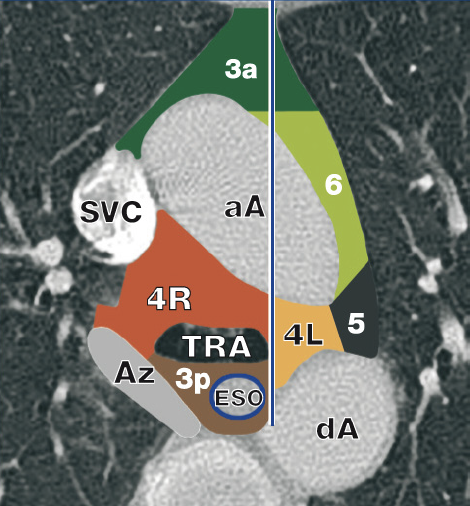
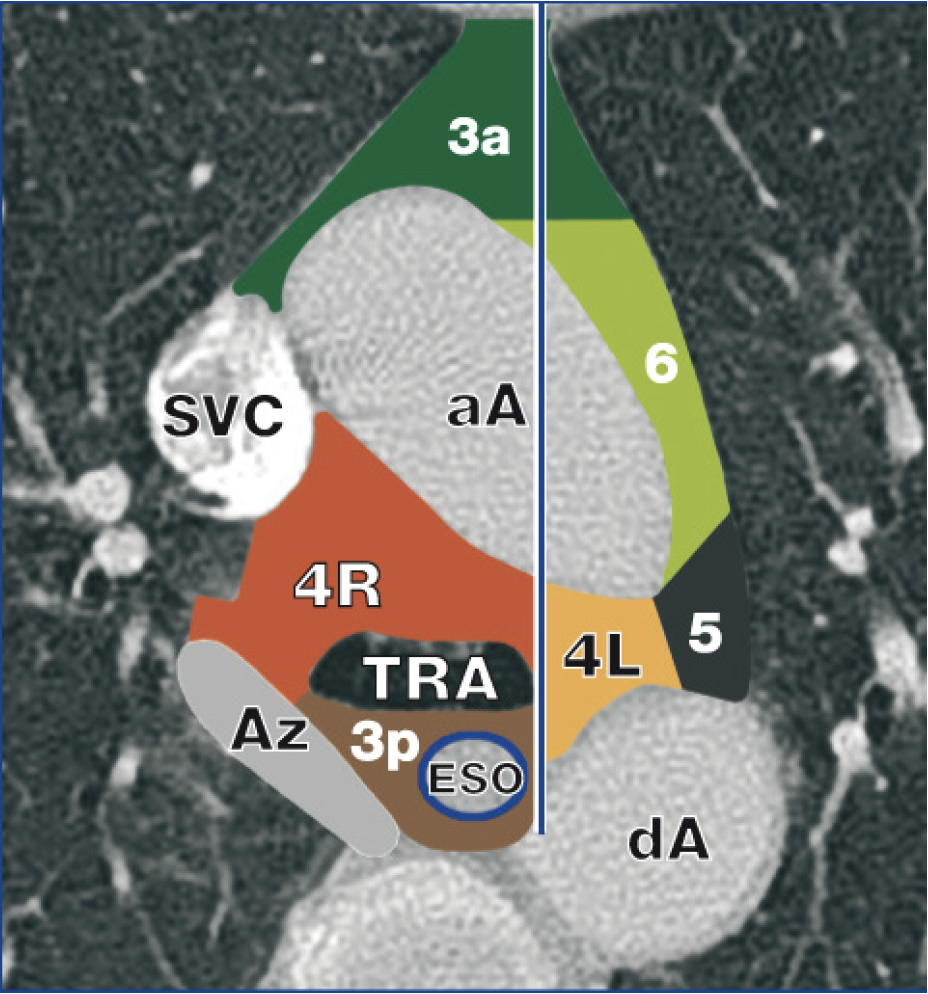
Introducing the endoscope further distal and rotating it to the 6 o’clock position places the endoscope at the area of lymph node station 3p (retrotracheal nodes).
Lymph node station 3p is situated in the space between pars membranacea tracheae and the vertebrae. Without a corresponding ultrasound landmark for the superior border of LN3p the lower border corresponds with the main carina and the main stem or left pulmonary artery. The border of LN3p towards LN2 and LN4 is the right and left posterior tracheal corner, which can be identified by ultrasound and in the endoscopic image.
NOTE: Station 3 lymph nodes are defined with an anterior part being the prevascular nodes (LN3a) and a posterior part being the retrotracheal nodes (LN3p). The anterior LN3 nodes are situated ventrally in front of the large vessels. Using endoscopic ultrasound, these nodes remain out of reach.
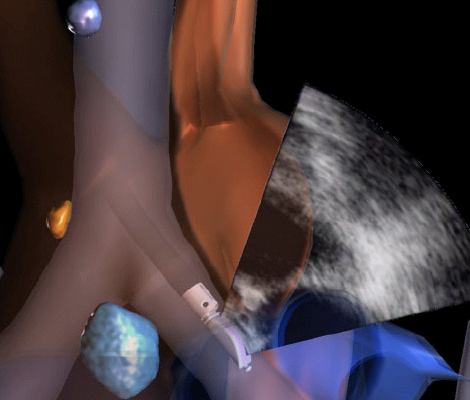
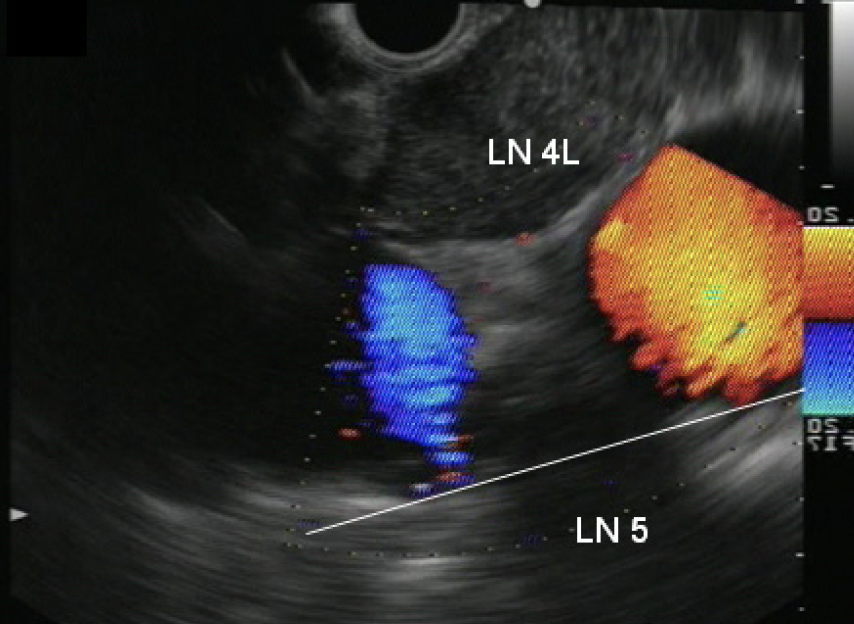
Turning the endoscope to the 9 o’clock position, the aortic arch is visualised which is the area of lymph node station 4L (Lower paratracheal nodes). The aortic arch can be followed posteriorly to the aortopulmonary window, with the aortic arch proximally and the left pulmonary artery distally. Lymph node station 4L includes nodes that are situated beyond the left lateral border of the trachea, medial to the ligamentum arteriosum.
Upper border: upper margin of the aortic arch
Lower border: upper rim of the left main pulmonary artery
NOTE: The midline of 4R and 4L is the left lateral border of the trachea.
Lymph node station 5 (Subaortic nodes) is situated laterally to station 4L nodes with the ligamentum arteriosum as anatomic border. LN5 nodes are located caudal to the inferior border of the aortic arch. Differentiation between 4L and 5 can be difficult as the ligament cannot be visualized by endoscopic ultrasound. Using EBUS-TBNA these nodes usually remain out of reach.
Lymph node station 6 (Para-aortic nodes) is located lateral to the ascending aorta. Using endoscopic ultrasound, these nodes remain out of reach.
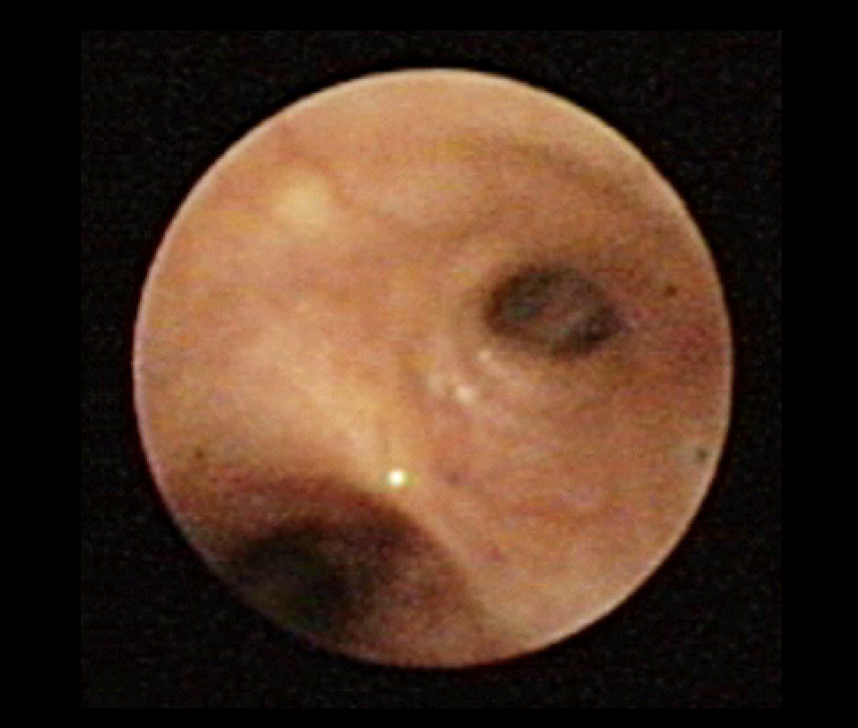
The endoscope is placed close to the main carina. By lifting the distal end of the endoscope and a slight turn to the right the endoscope is advanced into the right main bronchus. Verification for successful insertion of the endoscope to the right main bronchus is obtained from the view to the right upper lobe which branches off the right main bronchus only a few (2-3) centimetres after the main carina was passed. Switching back to the endoscopic view the image shows the upper lobe carina.
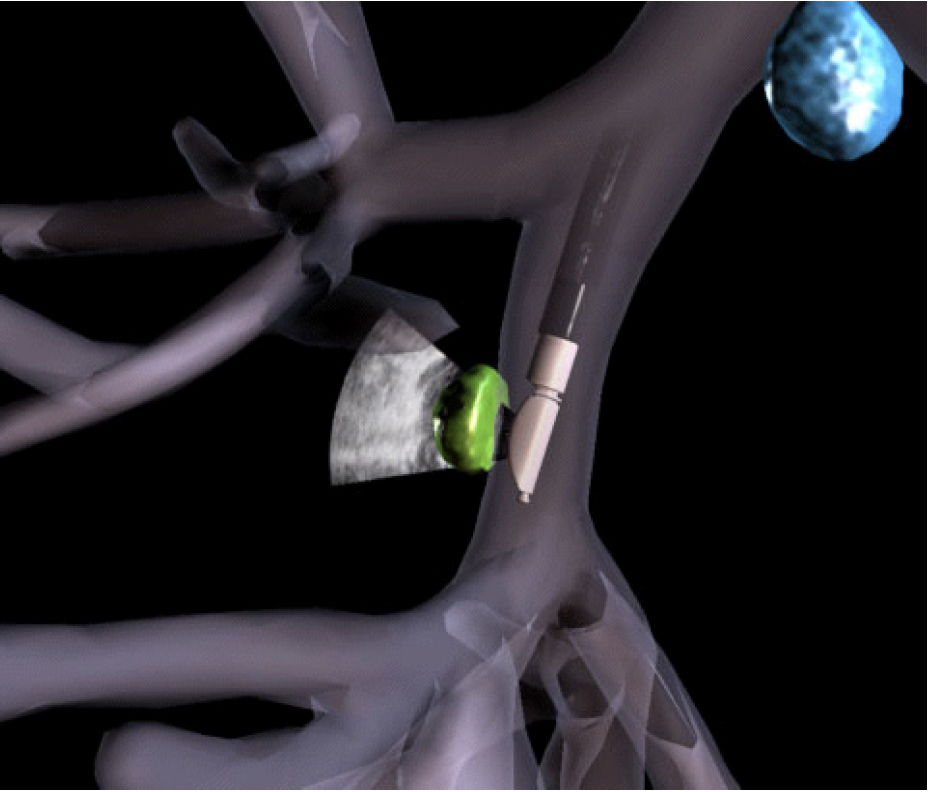
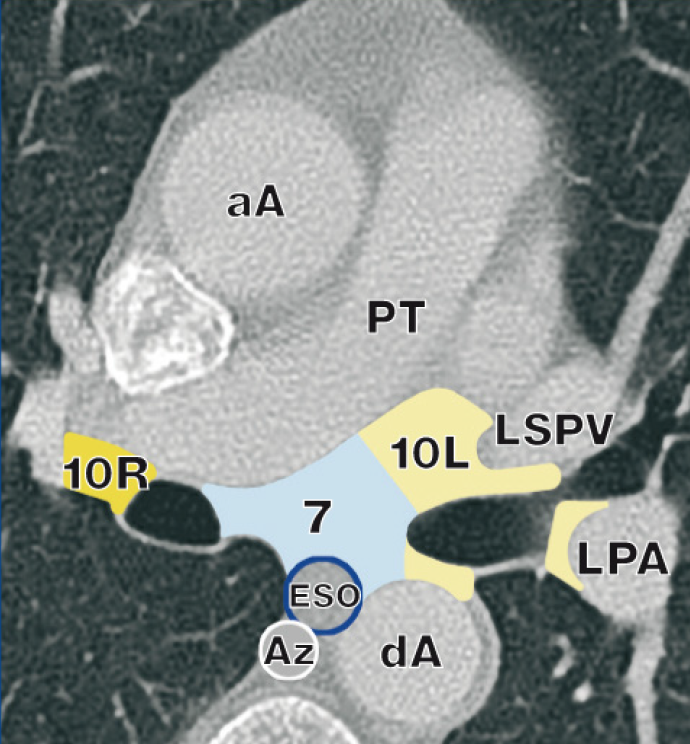
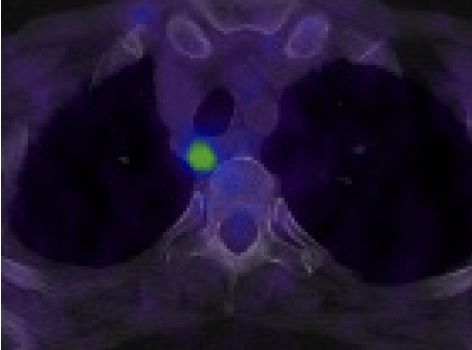
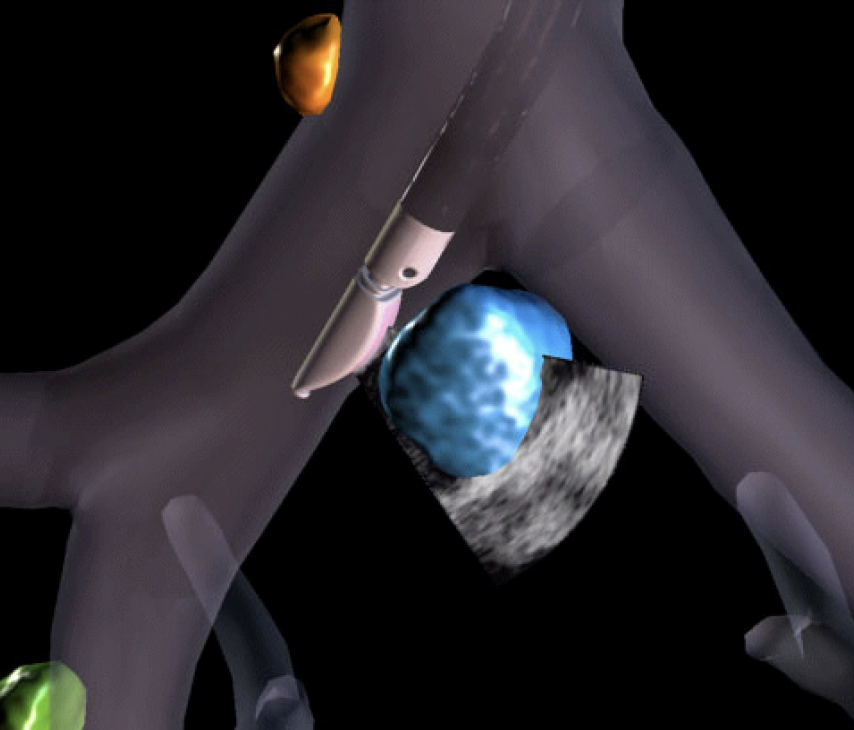
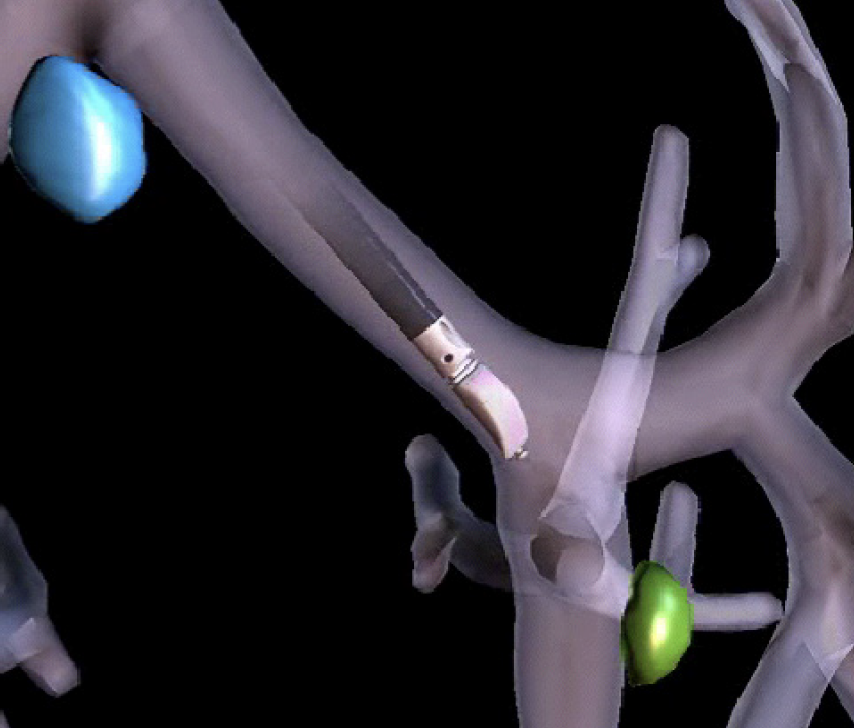
The endoscope is turned to the 9 o’clock position and the transducer is pressed against the bronchial wall of the right main bronchus below the main carina, which is the level of lymph node station 7 (Subcarinal nodes).
Upper border: the carina of the trachea
Lower border: the upper border of the lower lobe bronchus on the left; the lower border of the bronchus intermedius on the right
Use the endoscopic image to localise the borders of station 7.
This station should also be examined with the endoscope entering the left main bronchus. With a turn to the 3 o’clock position the area of station 7 can be examined from the left side.
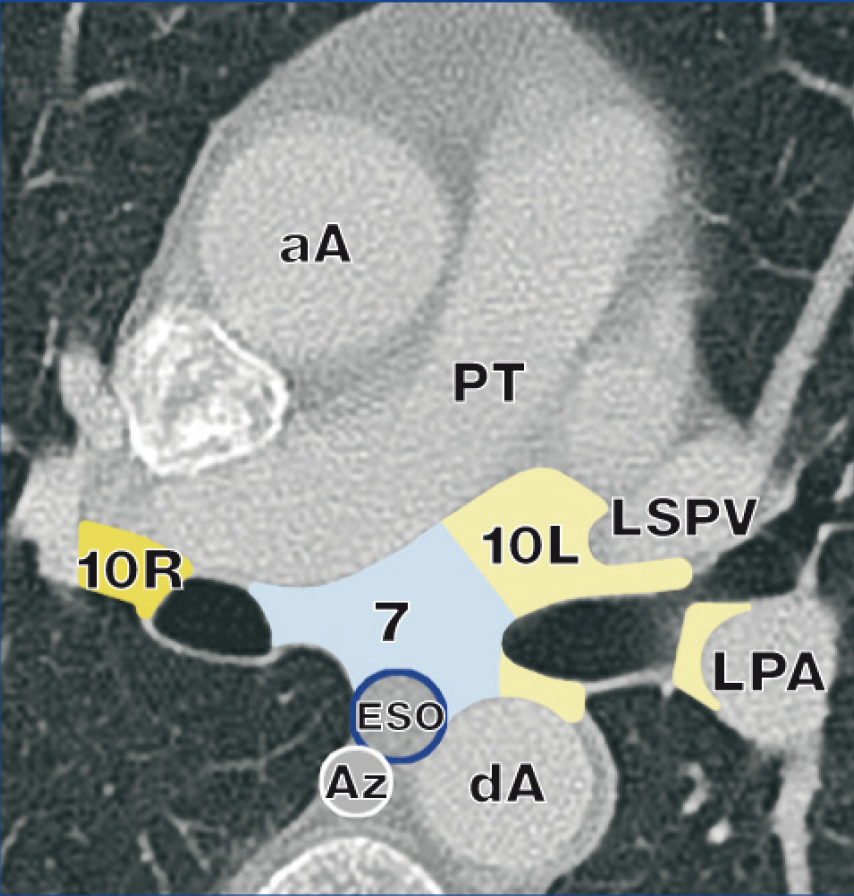
NOTE: Using EUS-FNA the left atrium despite being easily recognisable in endoscopic ultrasound might be too restrictive to serve as lower anatomic border for LN7. The relation of the left atrium or pulmonary artery to the bronchus intermedius and the left lower lobe bronchus can be variable.
Lymph node station 10L – assuming a primary tumour in the left lung – is as well as LN11L (LN12L, etc.) a station that could define a N1 stage disease.
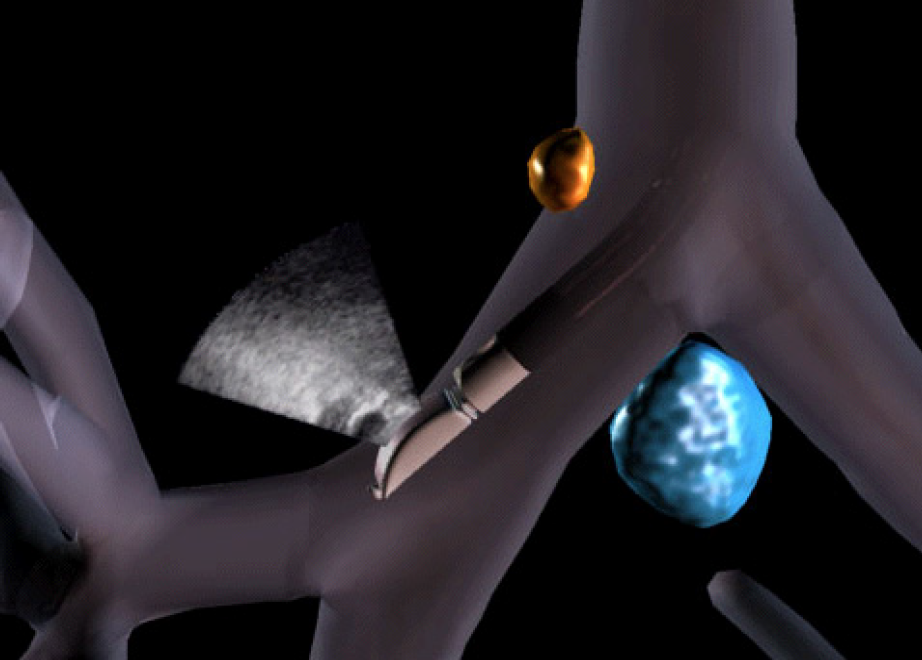
Under endoscopic view the endoscope is further pushed into the left main bronchus towards the carina of the left upper lobe and the left lower lobe. The transducer is pressed to the bronchial wall at the 11 o’clock position, the area of lymph node station 10L (Hilar nodes).
Station 10L includes nodes immediately adjacent to the mainstem bronchus and hilar vessels including the proximal portions of the left superior pulmonaryvein and the left pulmonary artery.
upper border: upper rim of the left pulmonary artery
lower border: interlobar region bilaterally
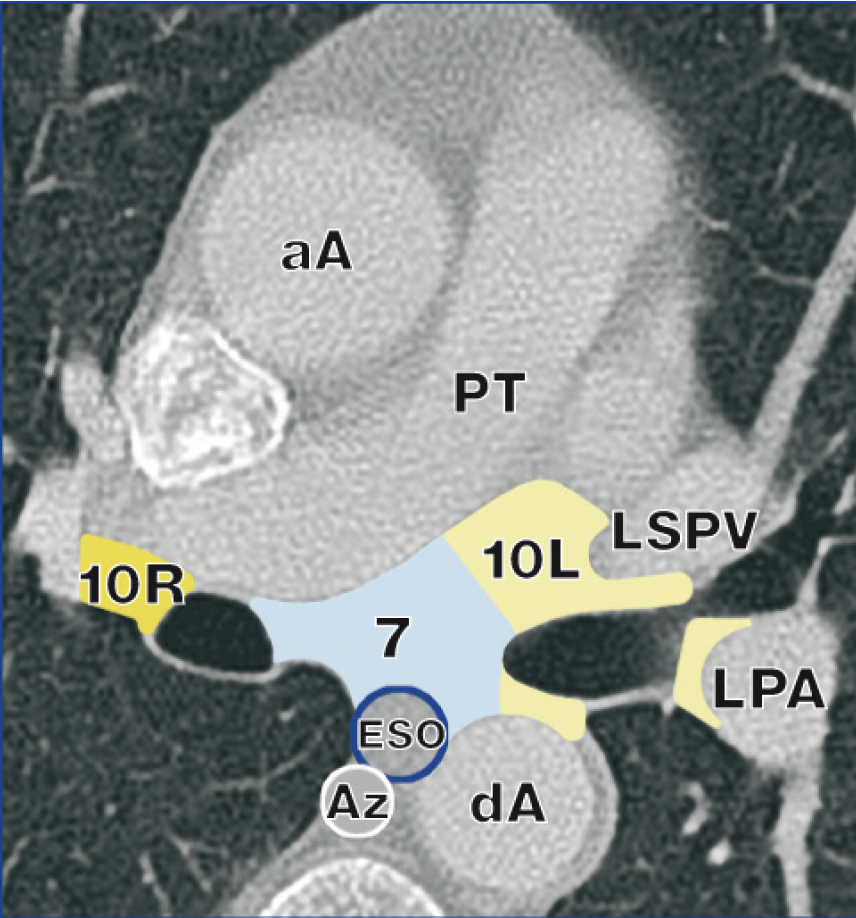
There is no unique ultrasound landmark that defines that border. Use the endoscopic view to locate the secondary carina or the upper lobe split off which serves as a landmark of the lower border of 10L nodes.
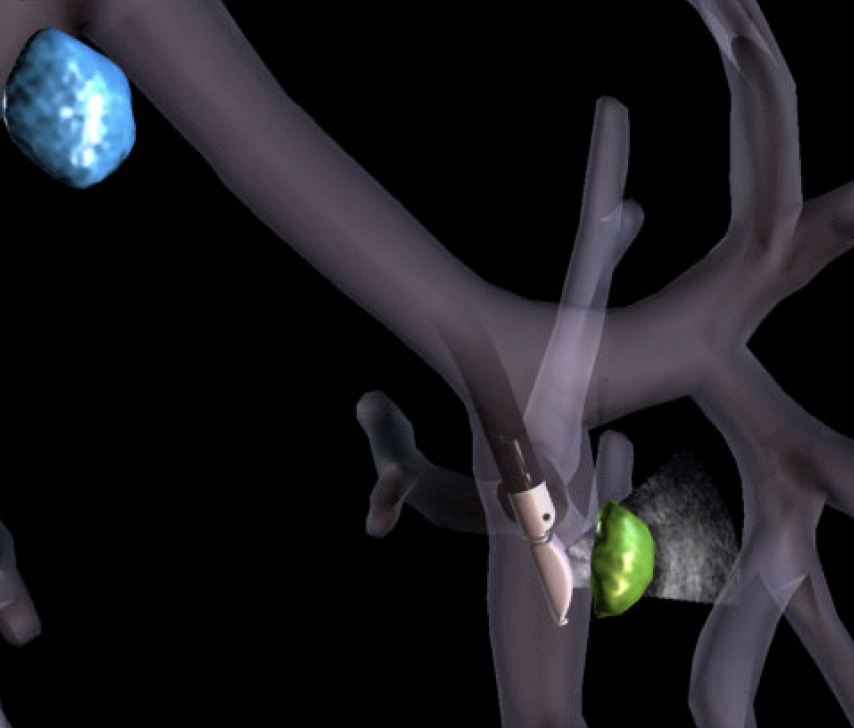
The endoscopic image still focuses on the wall of the left upper lobe. Then the endoscope is turned and approaches the left lower lobe. The endoscope rotates to the 2 o’clock position at the level of the proximal part of the lower lobe. This is the area of lymph node station 11L (interlobar nodes).
Once the secondary carina is reached, station 11L lymph nodes (interlobar nodes) are encountered. Use the endoscopic view to identify the bifurcation of upper and lower lobe.
Once the lobar bronchi originate, lymph node station 12L (Lobar nodes) is reached. There are no unique ultrasound landmarks. Use the endoscopic view for guidance.
Lymph node station 13L (Segmental nodes) and lymph node station 14L (Subsegmental nodes) frequently cannot be approached with EBUS-TBNA due to the instrument size.

After having completed the lymph node staging using EBUS-TBNA, the primary tumour can be sampled.
Note: For further differentiation of ingrowth versus compression a radial ultrasound miniature probe should be used as its higher ultrasound frequency allows differentiation of wall layer structures.
ADDENDUM:
EBUS-TBNA is defined to be a procedure using the tracheobronchial route. The endoscope however, can also be used in a second procedure in the same diagnostic session to approach mediastinal lymph nodes via the oesophagus (EUS-FNA). This can be especially valuable for the approach of LN station 5, 8 and 9.
Lymph node station 5 (Subaortic nodes) is situated laterally to station 4L nodes with the ligamentum arteriosum as anatomic border. LN5 nodes are located caudal to the inferior border of the aortic arch. Differentiation between 4L and 5 can be difficult as the ligament cannot be visualized by endoscopic ultrasound.
Using endoscopic ultrasound, these nodes usually remain out of reach.
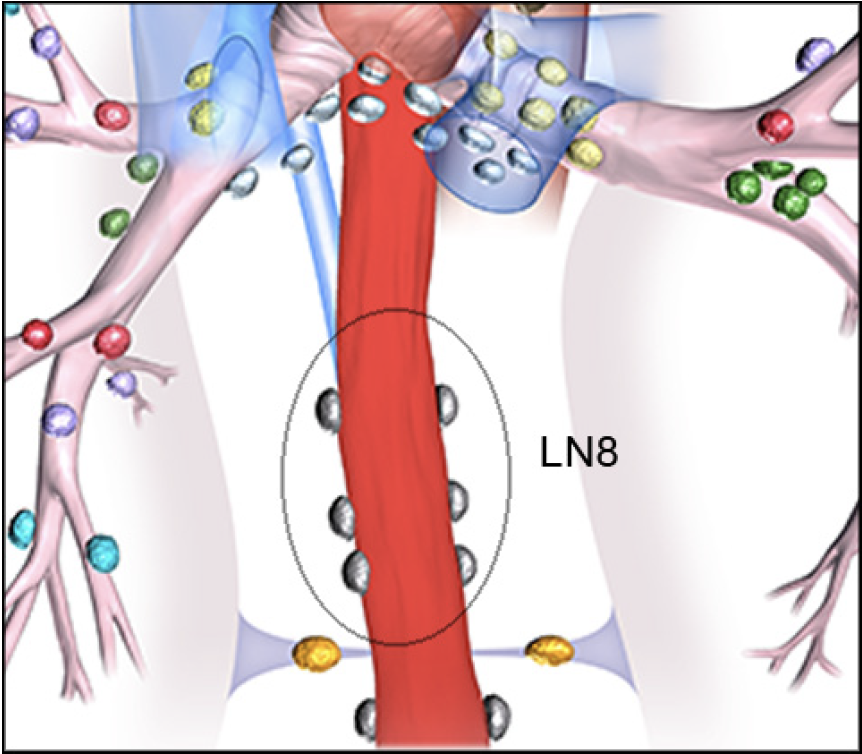
Lymph node station 8 (Para-oesophageal nodes)
Nodes lying adjacent to the wall of the oesophagus and to the right or left of the midline, excluding subcarinal nodes.
upper border: the upper border of the lower lobe bronchus on the left; the lower border of the bronchus intermedius on the right
lower border: the diaphragm
Station 8 nodes are located along the left atrium. The discrimination between the left- and right-sided nodes is the midline of the oesophagus.
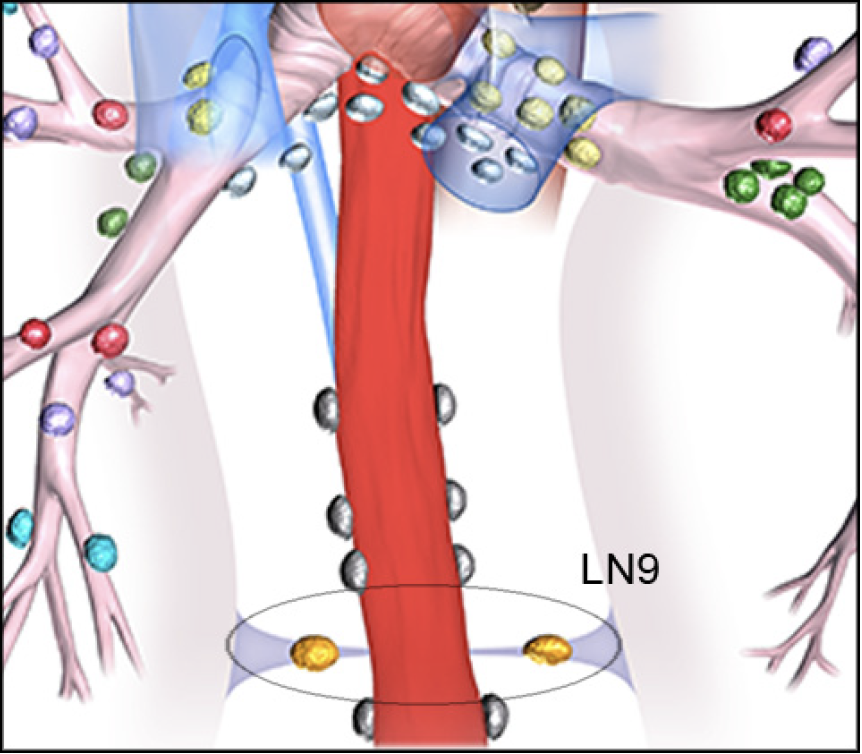
Lymph node station 9 (Pulmonary ligament nodes)
Nodes lying within the pulmonary ligament.
upper border: the inferior pulmonary vein
lower border: the diaphragm
As the pulmonary ligament cannot be identified with endoscopic ultrasound, search cranial to the diaphragm for lymph node station 9. The discrimination between the left- and right-sided nodes is the midline of the oesophagus.
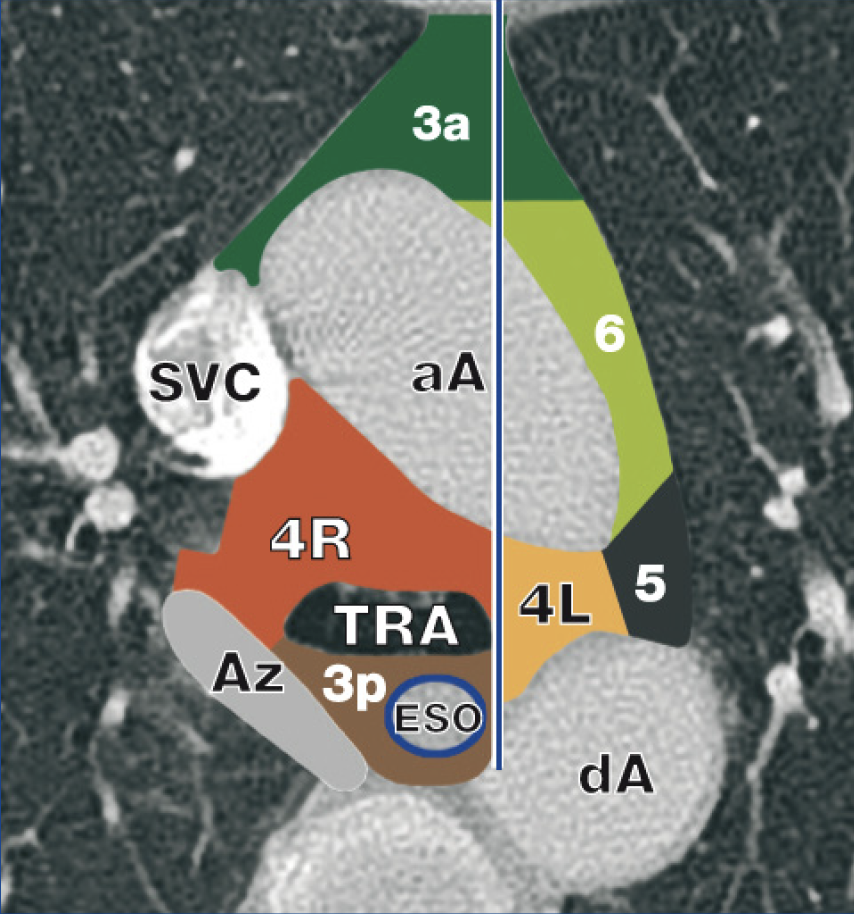
aA = Ascending aorta
LiV = Left innominate vein
RBCV = Right brachiocephalic vein
Az = Azygos vein
LPA = Left pulmonary artery
RCA = Right carotid artery
dA = Decending aorta
LSCA = Left subclavian artery
SVC = Superior vena cava
ESO = Esophagus
LSPV = Left superior pulmonary vein
TRA = Trachea
LCA = Left carotid artery
PT = Pulmonary trunk
- Content Type