Description of Endobronchial Ultrasound Transbronchial Needle Aspiration (EBUS-TBNA) in Pulmonary Medicine
Authors:
Prof. Peter Vilmann, MD, DSc, HC, Herlev Hospital, Copenhagen University Hospital, Denmark
Gentofte Hospital, Copenhagen University Hospital, Denmark
Source:
DVD-ROM ‘Endoscopic Ultrasound – Diagnostics and Staging of Lung Cancer’,
Olympus Europa SE & Co. KG, 2013
Preparation of the patient:
Under normal conditions sedatives and topical pharyngeal anaesthesia as used for routine endoscopy are used also when EBUS-TBNA is performed. In most cases, the procedure can be done without any additional discomfort to the patient, and therefore analgesics are usually not necessary. In cases where complete relaxation is desired general anaesthesia may be recommended. Under general anaesthesia a rigid tube or a laryngeal mask is used to secure the airways and to facilitate the insertion of the EBUS-TBNA bronchoscope.
Lab tests are not routinely required and the procedure is performed on an outpatient basis. Prophylactic antibiotics are not used routinely. In patients where either puncture of a cystic lesion is indicated, antibiotics are recommended.
Outlining the target area:
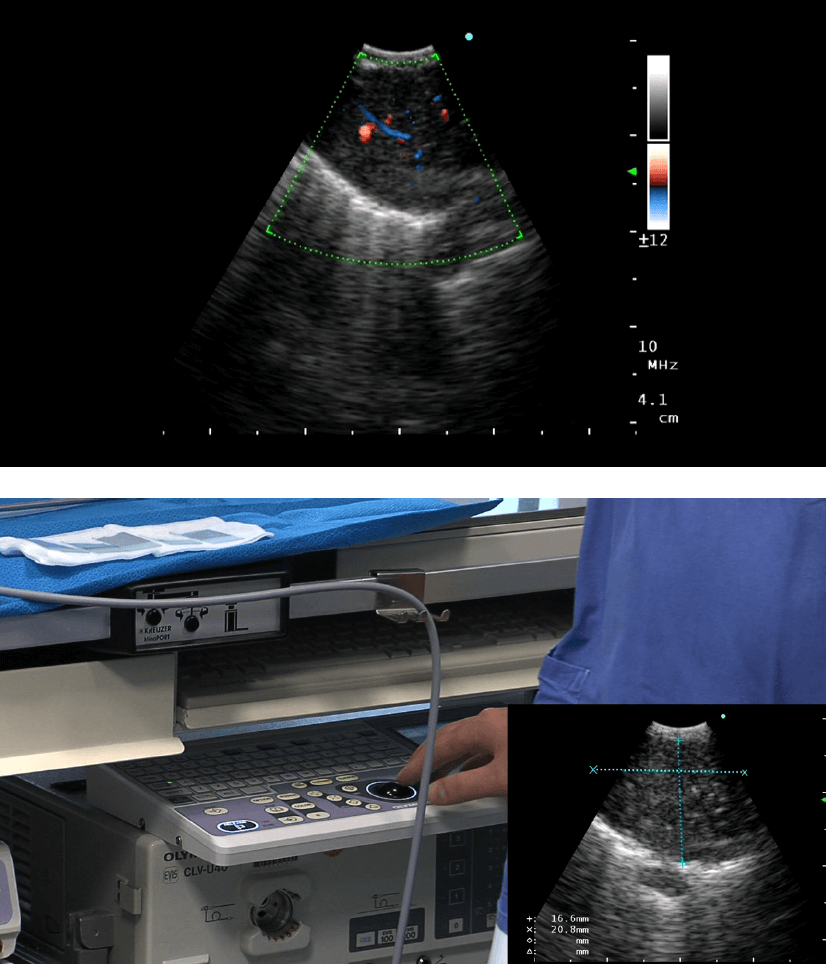
After the ultrasonic bronchoscope is inserted into the trachea the accessible lymph node station shall be explored and the lesions outlined. If available, Colour or Power Doppler examination of the target lesion as well as the anticipated path of the needle should be performed in order to avoid puncture of vessels to reduce the risk of bloody specimen with limited quality for the cytopathologist. It is important that the findings in the ultrasound image are exactly described and documented on video or by print-out. The following topics should be described:
– Location and orientation of the transducer
– Characteristics of the lesion:
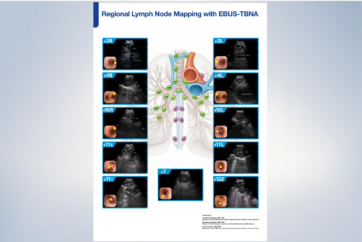
• location of a lesion (with reference to the IASLC staging nomenclature)
• size (long axis and short axis)
• shape (round, oval, triangular)
• demarcation (irregular/unsharp/sharp)
• echogenicity (echo poor/rich, mixed)
• number of lesions
• relation to lesions or organs and vessel structures
In cases with unclear location due to difficult anatomical situations, the uncertainty should be openly described.
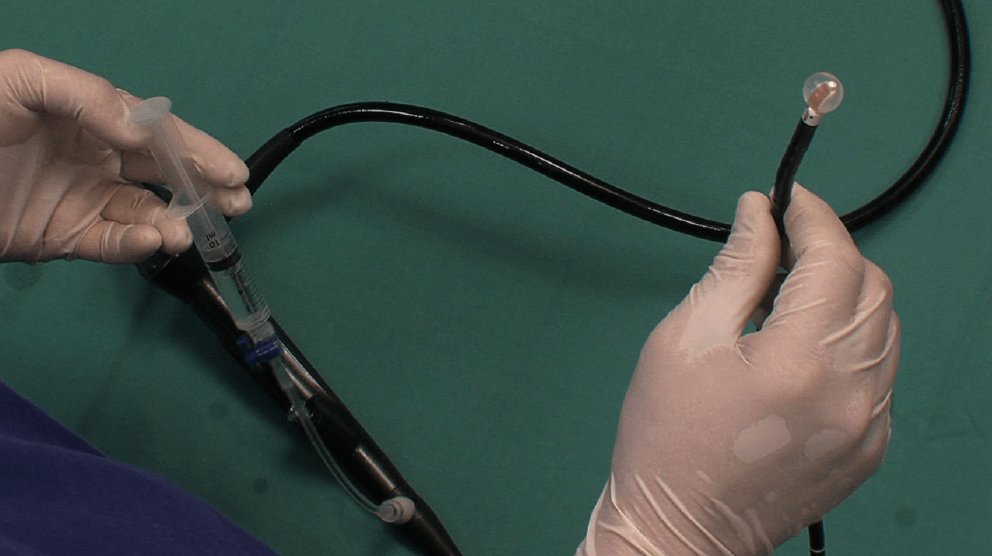
To outline the lesion and for full control during the needle aspiration, the ultrasound transducer has to be held in firm contact with the bronchial wall. This may sometimes be difficult due to the hard cartilage rings. The use of the optional balloon allows a better coupling of the transducer of the endoscope with the bronchial wall. The balloon also reduces stimulus to the cough receptors during the procedure under local anaesthetics, compared to when touching the bronchial wall directly with the rigid transducer of the endoscope. The balloon should therefore be prepared before the initial insertion of the endoscope into the patient.
Which lesion should be punctured first?
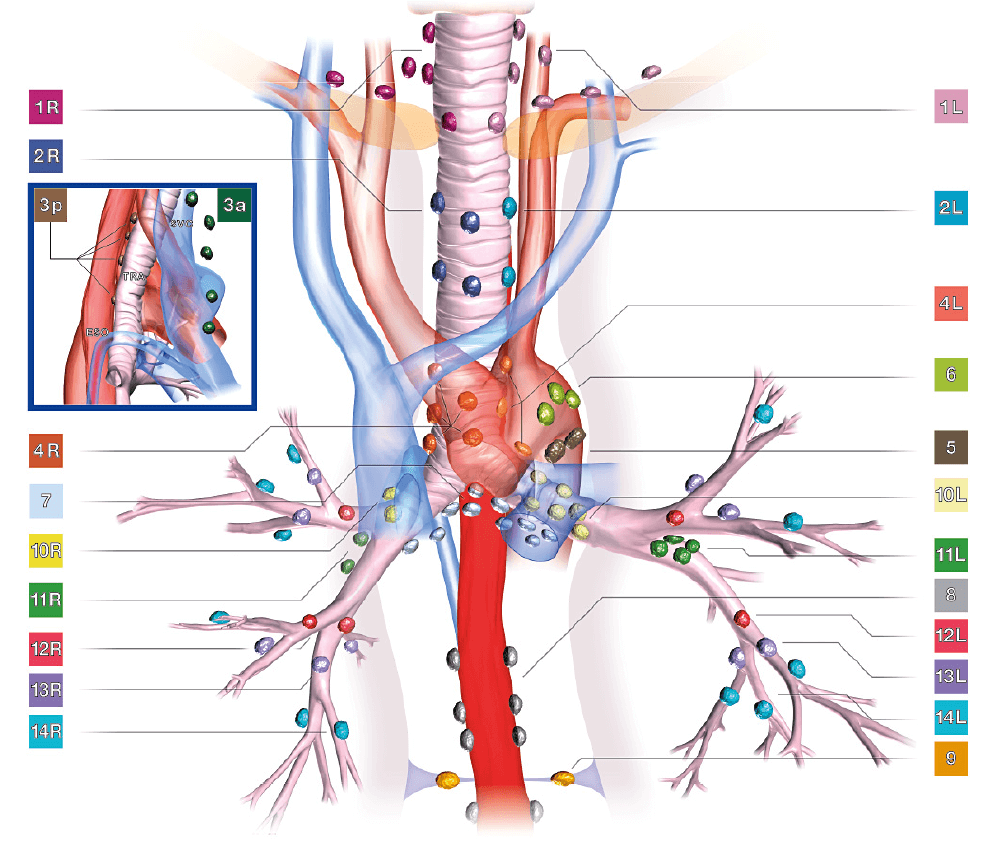
Patients with suspicion of lung cancer require reliable staging. EBUS-TBNA has proven to be of great value especially in lymph node staging (N-staging). After a complete examination of the relevant areas, the decision which lesion should be sampled has to be made. Generally, in lung cancer staging the lesion considered the most distant to the tumour should be targeted first.
→N-3 lymph nodes before N-2 lymph nodes and finally N-1 lymph nodes.
Usually needles are not exchanged when this rule is adhered to. However, if this rule can not be fulfilled, a new needle should be used for each lesion in order not to seed malignant cells into non-malignant lymph nodes in more distant regions/stations. An example could be a biopsy in a patient sent for diagnosis of a suspected primary lung cancer located in the mediastinum in whom a possible N-2 lymph node is outlined after the first biopsy.In this case a new needle should be used for the second biopsy.
Frequently, several lymph nodes are outlined in the same patient in the same lymph node station. It may be difficult to target all these lymph nodes. In such cases, the following rules may be advisable: Generally the lymph nodes with most malignancy criteria should have the highest priority i.e. size more than 1cm, round, echo poor structure with sharply demarcated margins. It should be stressed that no scientific data support the described strategy. Until clear data are available it is advisable to sample as many lymph nodes as possible, irrespective of criteria of malignancy.
It may be that a lymph node is located deep to other less malignant looking lymph nodes and in these cases puncture through superficial lymph nodes may be necessary. Occasionally there will be lymph nodes that require passing the needle through a larger vessel. Care should be taken with suction used for aspiration as aspiration of blood would spoil the specimen obtained from the lymph node.
Equipment preparation and procedural steps
Refer to chapter ‘EBUS-TBNA – Step-by-Step’ to find the detailed description of the EBUS-TBNA procedure.
Difficult punctures
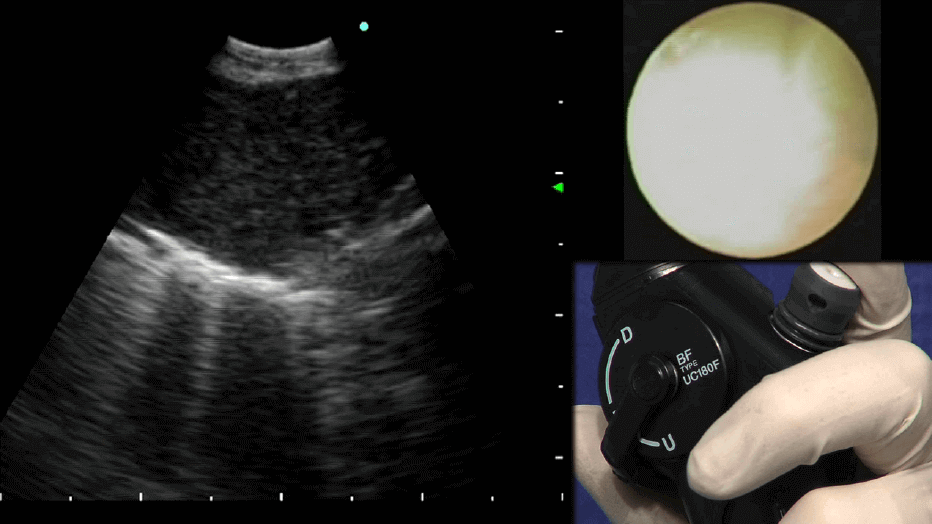
The importance of a steady position of the transducer related to the lesion to be punctured should be stressed. The needle tends to push the transducer away from its steady contact with the wall, particularly when hard lesions are punctured. This is, however, not a major problem, since adjustment of the transducer position usually regains the ultrasonic contact with the needle rather easy. There are 6 ways of improving this contact during puncture.
1. stronger angulation of the endoscope tip increases the transducer contact with the bronchial wall.
2. an assistant should hold the insertion tube of the bronchoscope to prevent a backward movement of the tube during first needle penetration.
3. using the balloon (filling it with de-aerated water) brings better acoustic coupling and thus an improvement of the ultrasound image in many cases.
4. moving the needle slightly backwards usually restores the ultrasound image.
5. in hard tissue (or lymph nodes embedded in soft tissue) short strong needle pushes might help to push the needle inside the lesion.
6. occasionally a cartilage ring may preclude the penetration of the needle. If so, another transducer position has to be found, usually moving just a few millimetres up or down.
In cases of inadequate needle monitoring the needle is withdrawn at first to a location beneath the transducer, but still outside the needle sheath. If the needle is not fully visible by then, the needle is completely withdrawn before a new puncture procedure is initiated.
Biopsies through vessels should be avoided but they are seldom a problem.
Movement of the heart is rarely a problem since the distance from the transducer to the lymph node is short, making biopsies of even minute lesions less than one centimetre in diameter possible.
- Keyword
- Content Type