Colonoscope Series
Points Related to the Application of Endocyto to Diagnosis of Colorectal Lesions in Real Clinical Practice
Dr. Masashi Misawa
Showa University Northern Yokohama Hospital, Digestive Disease Center
I. Characteristics of Endocyto and Clinical Benefits in Endoscopic Diagnosis
Ultra-magnifying endoscopic observation opens the door to a new era of diagnostic methods
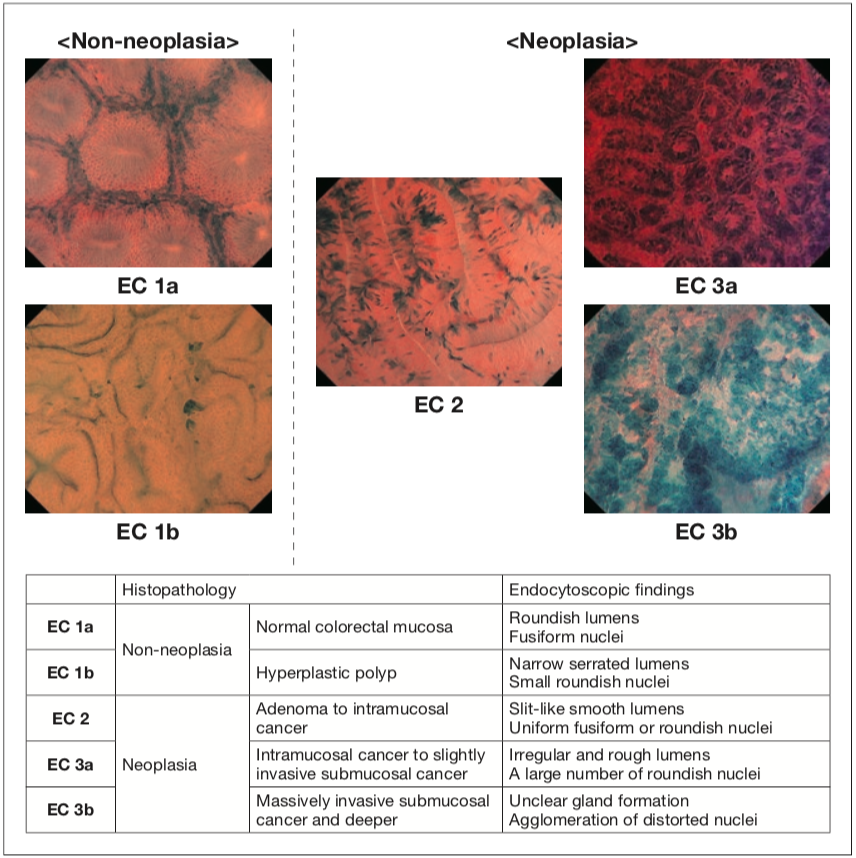
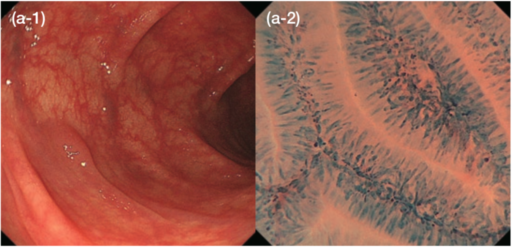
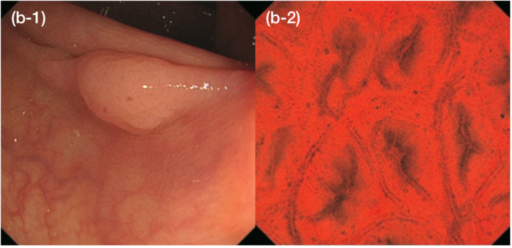
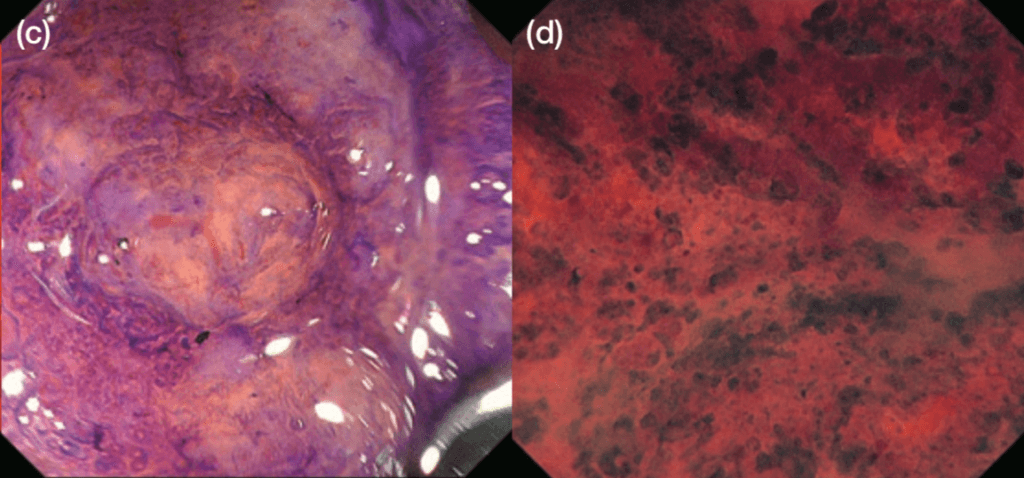
The emergence of Endocyto has enabled in vivo, on-site assessment of the cell nuclei and capillaries of colorectal lesions. The ability to obtain in vivo images that are virtually identical to pathological findings is a significant paradigm shift. This technology provides additional, reliable information on lesions difficult to obtain using conventional diagnostic methods. We believe more confident diagnoses can be made where there was previously uncertainty about differentiating neoplasia from non-neoplasia or about the depth of invasion of colorectal lesions. For example, when differentiating between neoplasia and non-neoplasia is difficult under white light, use of our EC classification (Figure 1) of findings obtained by ultra-magnifying endoscopic observation (endocytoscopy: EC) will facilitate discriminating between these possible diagnoses (Figure 4). When there is uncertainty about the depth of invasion with pit pattern diagnosis, EC observation can be added. If the EC findings indicate EC 3b, massively invasive submucosal cancer can be diagnosed with a high degree of confidence (Figure 5)1).
Observation with the combination of EC and NBI immediately provides more detailed vascular findings than magnifying NBI alone2), which is extremely useful clinically because this combination is very easy to use and does not require staining. Our procedure is first to assess a detected lesion using EC with NBI to determine whether it is a neoplasia or not and if an invasive cancer is suspected. Subsequently, methylene blue staining can be performed to enable observation of the cell nuclei by EC, thus enabling a more confident diagnosis.
Routine use of Endocyto from diagnosis to treatment is possible because it has a smaller diameter than conventional magnifying endoscopes
Endocyto allows adjustment of magnification from no magnification to EC observation with up to 520× magnification (when using with 26 inch monitor:OEV262H) by means of a series of zoom lever manipulations similar to those of conventional magnifying endoscopes. In addition, its diameter is smaller (12.8 mm: diameter at the distal end of the technology verifier) than the currently marketed magnifying colonoscope CF-HQ290Z thus, insertion is easy. In our facility, novices in colonoscopy readily use Endocyto as their routine practice, thus making optimal use of these features. If EC observation is freely available in the clinical setting for all patients, new and unexpected discoveries of academic interest may result.
Other important features of the Endocyto colonoscope besides the magnification include the water jet function and 3.2 mm forceps channel (the technology verifier). These features make it usable not only for observation, but also for endoscopic treatment. Many endoscopists think Endocyto is suitable only for particular purposes; however, we consider that the above characteristics make it eminently suitable, indeed preferable, for routine use. Consequently, it will be used for observations when an occult blood test has been positive and for routine checkups, not to mention close observation of detected lesions. Endocyto enables us to make on-site
diagnoses of detected lesions with comparable ability to that of a pathological diagnosis without changing scopes, determine the optimal treatment plan, and then to immediately administer the optimal treatment. We therefore regard this endoscope as versatile in a very wide range of situations.
Getting accustomed to using Endocyto
When Endocyto is used for EC observation, magnification is further increased as an extension of the usual magnifying observation, and EC images are obtained at the maximum magnification when the distal end of the scope is in contact with the mucosa. Therefore, endoscopists who have been using conventional magnifying endoscopes are unlikely to encounter any technical obstacles in handling the device. Notably, because observations are made in contact with the mucosa, EC observation does not require keeping the endoscope at a certain distance from a lesion, unlike with conventional magnification. This is a great advantage because EC images can be obtained relatively easily even when there is respiratory movement. However, in order to maximize the advantages of EC observation, endoscopists who lack experience of magnifying endoscopy do need to take some time to get accustomed to maneuvering the device. We recommend gradually getting used to maneuvering the device by starting with rectal lesions, which are relatively unaffected by respiratory movement, and then move on to master the use of Endocyto.
II. Procedure and Techniques for Observation with Endocyto
EC with NBI observation
In this section, we introduce our procedures for assessing colorectal lesions with Endocyto in our facility.
When observing colorectum with Endocyto, EC with NBI (or magnifying NBI) is preceded by observation under white light. The most basic of basics in all endoscopic observations, initial thorough washing of lesions, is also important when observing lesions with EC with NBI. Given the optical properties of NBI, a little residual mucus is unlikely to interfere with observation and good vascular images can be obtained relatively easily. However, considering that staining will subsequently be applied, the lesion should be washed thoroughly. After a complete view of the lesion has been captured under white light, EC with NBI images can easily be obtained by making contact with the lesion and zooming in fully. Because magnification can be changed progressively from none to ultra- magnification with Endocyto, NBI observation is also possible at a magnification near that of conventional magnifying endoscopes.
Methylene blue staining and EC observation
A more confident diagnosis can be made after observation with EC with NBI by applying methylene blue staining and making a diagnosis according to the EC classification. In our facility, we currently routinely use methylene blue staining alone for EC observation. However, of course adding methylene blue after crystal violet staining also yields good EC images and is not problematic.The specific procedure for methylene blue staining (Table) is as follows: Wash the lesion thoroughly to remove any mucus and then successively drop on small amounts of 1% methylene blue at a time with a spreading tube. Suction any excess stain slowly and pause briefly; the best images can be obtained when a staining time of about one minute has elapsed. Next wash the lesion again. Because methylene blue dyes the mucus on the surface layer, making it darker, good images can only be obtained subsequent to methylene blue staining after removing mucus again by thorough washing before further observation. After washing, bring the scope into contact with the lesion, zoom in fully and observe it with EC. If staining has been insufficient, perform additional staining according to the same procedure.
|
Below similar instructions are listed and numbered.
Table Nucleus staining with methylene blue stain in EC observation of the colon |
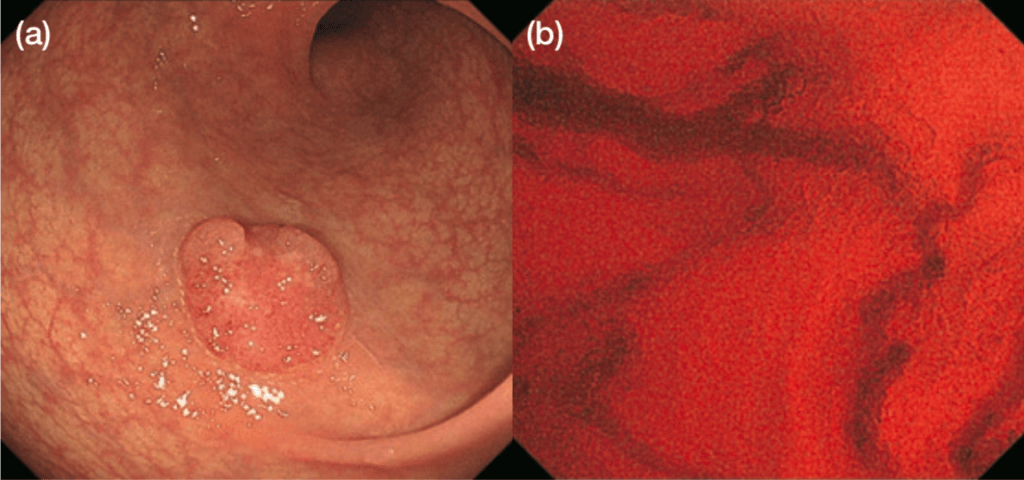
Adjustment of magnification with Endocyto and technique for contact observation with full zooming
The method for increasing the magnification for ultra-magnifying observation (EC with NBI or EC alone) (Figure 6) varies depending on the condition of lesions. There are two specific examples. One is the case where the lesion is relatively small and the whole lesion is found to be homogeneous, making it difficult to differentiate between neoplasia and non- neoplasia, and another one is the case where the lesion is large and inhomogeneous. In the former case, the findings will be the same anywhere within the lesion; therefore contact is made where it is easiest to do so, after which EC with NBI images or EC images are obtained with full zooming. In the latter case, the zoom lever is kept down slightly during magnifying observation and contact is made taking care not to lose the area of interest, after which EC with NBI images or EC images are obtained with full zooming. If the area of interest is lost, magnification should be dialed back until the target area is again located and then gradually increased again to refine the image.
When the scope is brought into contact with the mucosal surface of the lesion under full zooming, bleeding might occur and can interfere with EC observation. The lens of the Endocyto projects slightly further than those of conventional magnifying endoscopes, making it easier to bring the lens into contact with the mucosal surface. Therefore, the knack for avoiding bleeding is not to push the distal end of the scope hard but rather to make light contact. If bleeding occurs, washing as needed using the water jet function will prevent interference with observation.
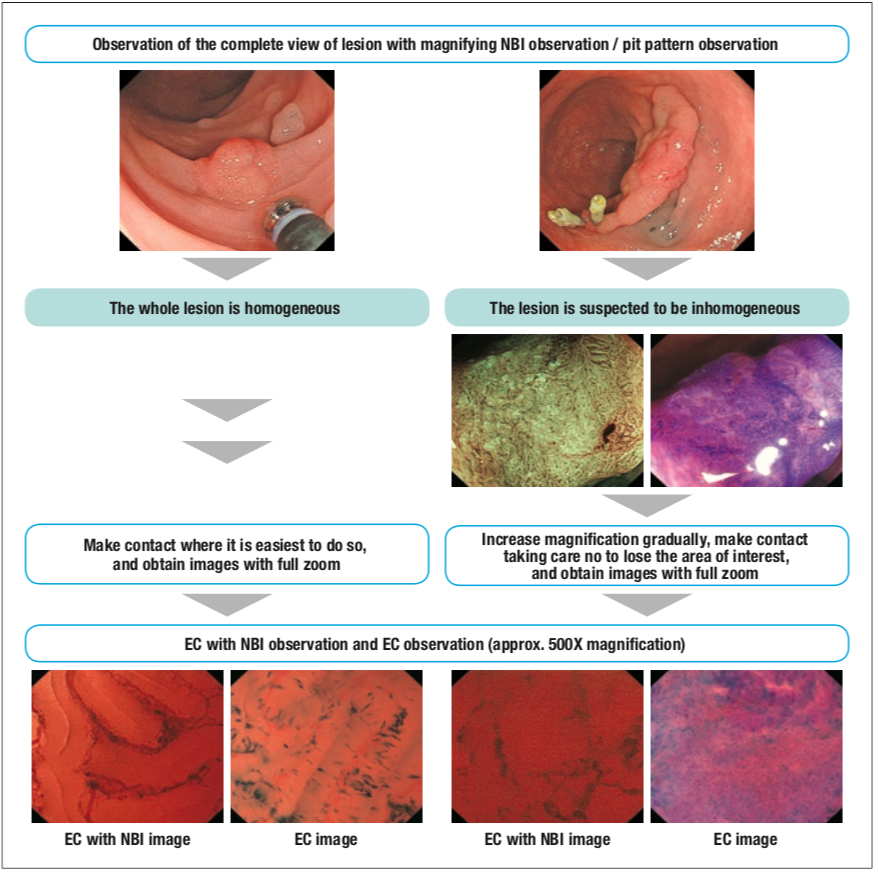
Figure 6 Magnification adjustment in EC with NBI and EC observation with Endocyto [based on reference 5]
III. Expectations Regarding the Further Advantage of Endocyto
Improved ability of endoscopic diagnosis and elucidation of pathologic characteristics of various gastrointestinal disorders
It has become clear that by far the greatest advantage of Endocyto in endoscopic diagnosis of colorectal lesions is high diagnostic ability. In a randomized comparative study using biopsy specimens as the gold standard, we demonstrated that the ability of EC observation to differentiate between neoplasia and non-neoplasia was not inferior to pathological diagnosis with accuracy of 96% in pathological diagnosis of biopsy and 94.1% in EC observation3). In other words, Endocyto may be capable of making in vivo and on-site pathological diagnoses. We have also shown diagnostic ability can be improved by adding EC observation to pit pattern diagnosis when ascertaining depth of invasion and whether the lesion is a massively invasive submucosal cancer1). We have reported many other studies supporting the advantages of Endocyto, including documenting the diagnostic ability of EC with NBI2, 4) and in evaluating inflammatory activity in ulcerative colitis.5).
We believe that Endocyto will prove to have even greater potential beyond this demonstration. We hope its high diagnostic ability will be exerted in the future not only for diagnosis of cancer, including assessment of differentiation grade and prediction of metastasis and relapse, but also for elucidation of pathological characteristics of diseases where conventional endoscopes fails to detect any abnormality, such as functional dyspepsia.
[References]
1) Kudo SE, Mori Y, Wakamura K, et al. Endocytoscopy can provide additional diagnostic ability to magnifying chromoendoscopy for colorectal neoplasms. J Gastroenterol Hepatol 2014;29: 83-90.
2) Kudo SE, Misawa M, Wada Y, et al. Endocytoscopic microvasculature evaluation is a reliable new diagnostic method for colorectal lesions (with video). Gastrointest Endosc 2015; 82:912-923.
3) Mori Y, Kudo S, Ikehara N, et al. Comprehensive diagnostic ability of endocytoscopy compared with biopsy for colorectal neoplasms: a prospective randomized noninferiority trial.Endoscopy 2013; 45: 98-105.
4) Nakamura H, Kudo SE, Misawa M, et al. Evaluation of microvascular findings of deeply invasive colorectal cancer by endocytoscopy with narrow-band imaging. Endosc Int Open 2016; 4:E1280-E1285.
5) Maeda Y, Ohtsuka K, Kudo SE, et al. Endocytoscopic narrow-band imaging efficiency for evaluation of inflammatory activity in ulcerative colitis. World J Gastroenterol 2015; 21: 2108.