Gastric Cases 6

Dr. Hisashi Doyama
Vice Director, Ishikawa Prefectural Central Hospital, Japan
TXI improves the visibility of lesions by enhancing the overall color tones (such as redness, discoloration, and yellowness) and textures (such as unevenness)
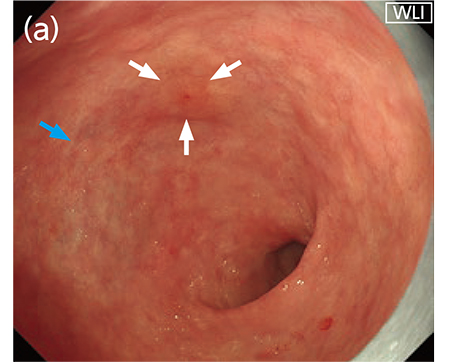
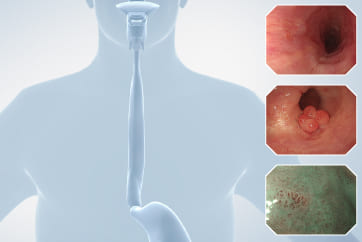
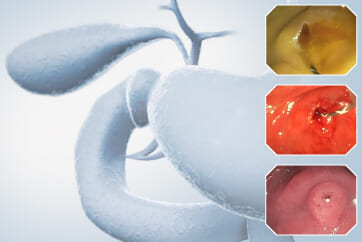
TXI (TeXture and color enhancement Imaging), a new image processing technology installed in the next-generation endoscopy system EVIS X1, was created to improve imaging performance. It is expected to contribute to the improvement of lesion visibility in gastric cancer screening by enhancing the changes in the color tone and structure of the mucosal surface. When I used TXI mode 1 to observe differentiated gastric cancer (which had been characterized by a faintly reddish and flat elevated lesion under WLI [white light imaging]), both the redness of the lesion and the discoloration of the perilesional gastritis were enhanced. The yellowness of the gastric submucosal tumors and xanthomas was also further enhanced under TXI (Fig. 1). Therefore, the standout feature of the color tone enhancement by TXI is that the entire color tone (including white and red) is enhanced.
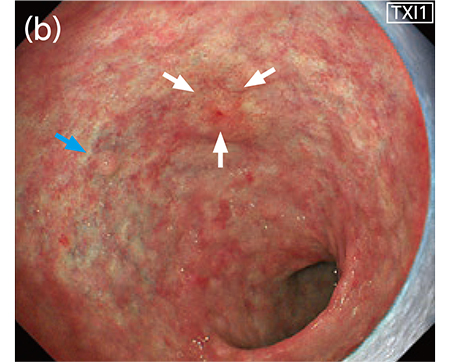
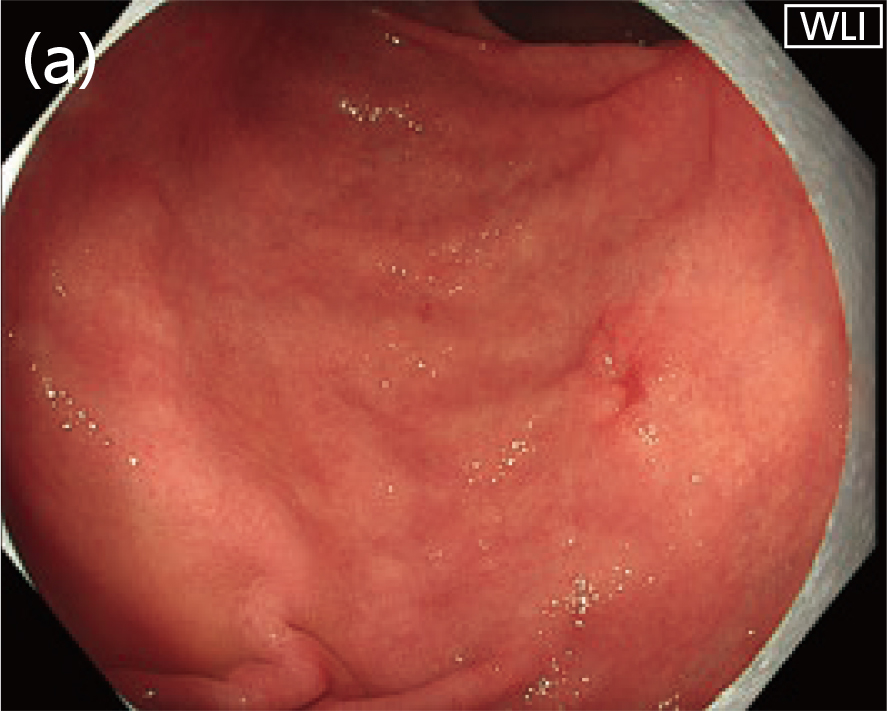
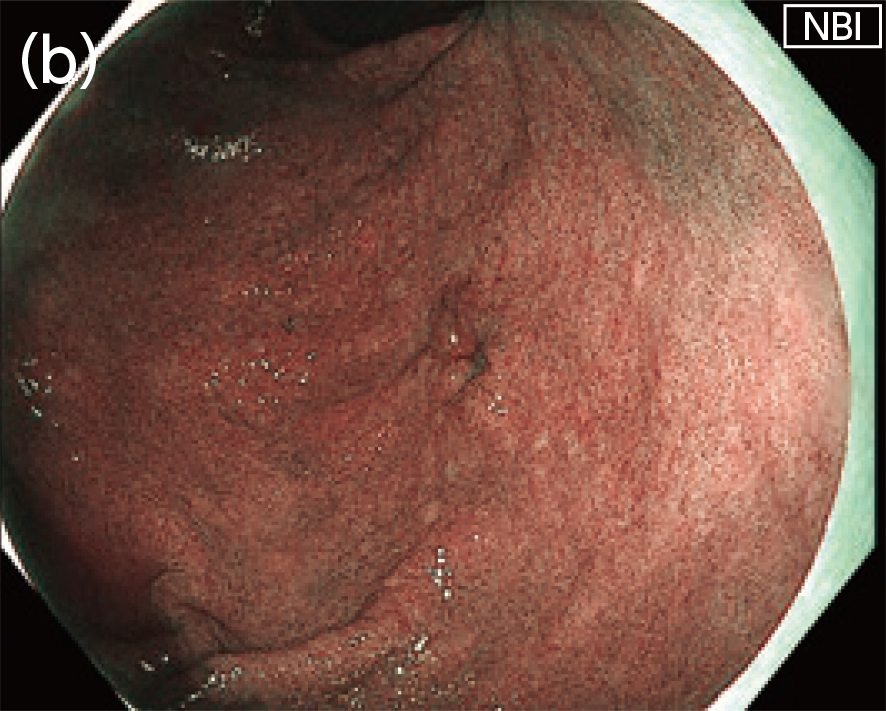
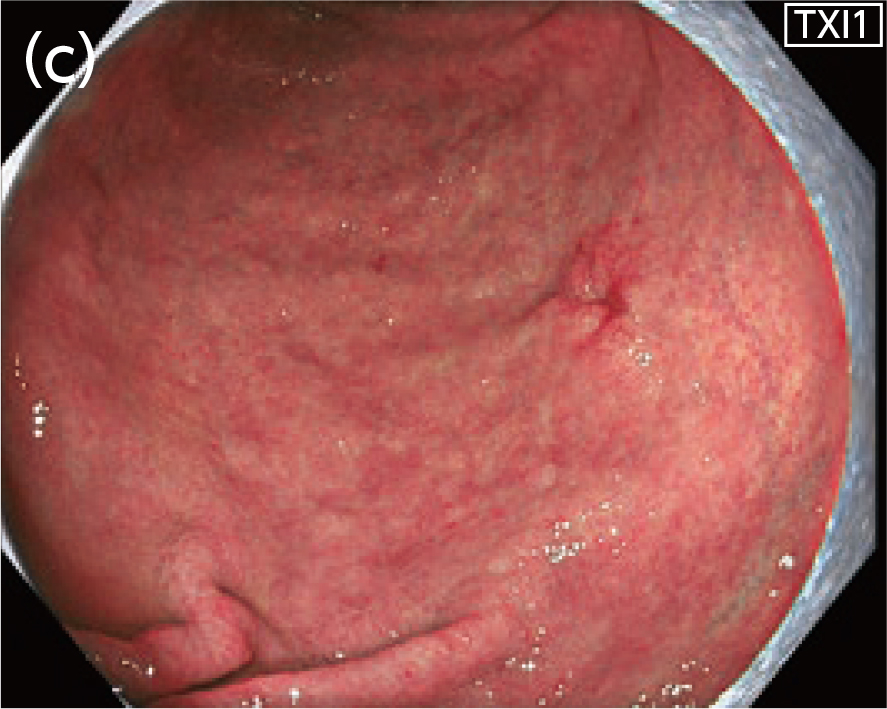
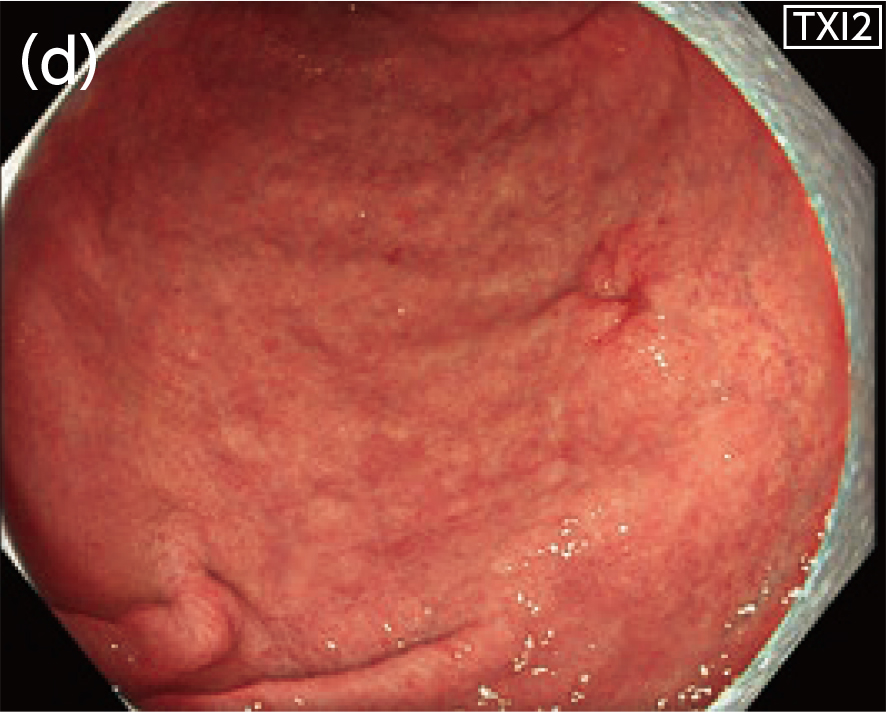
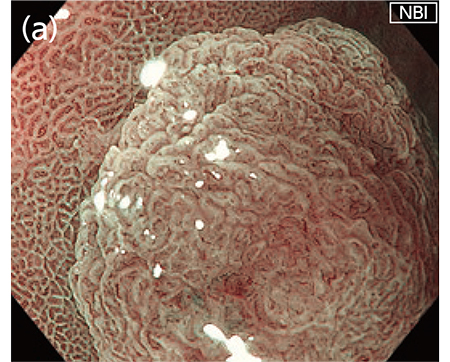
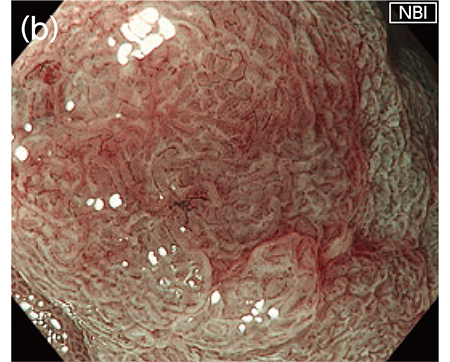
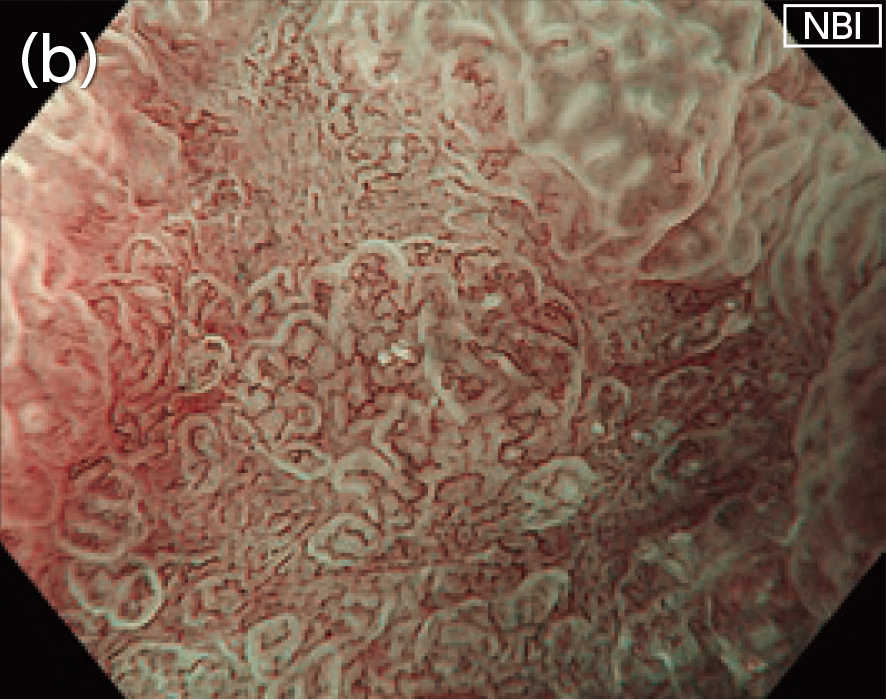
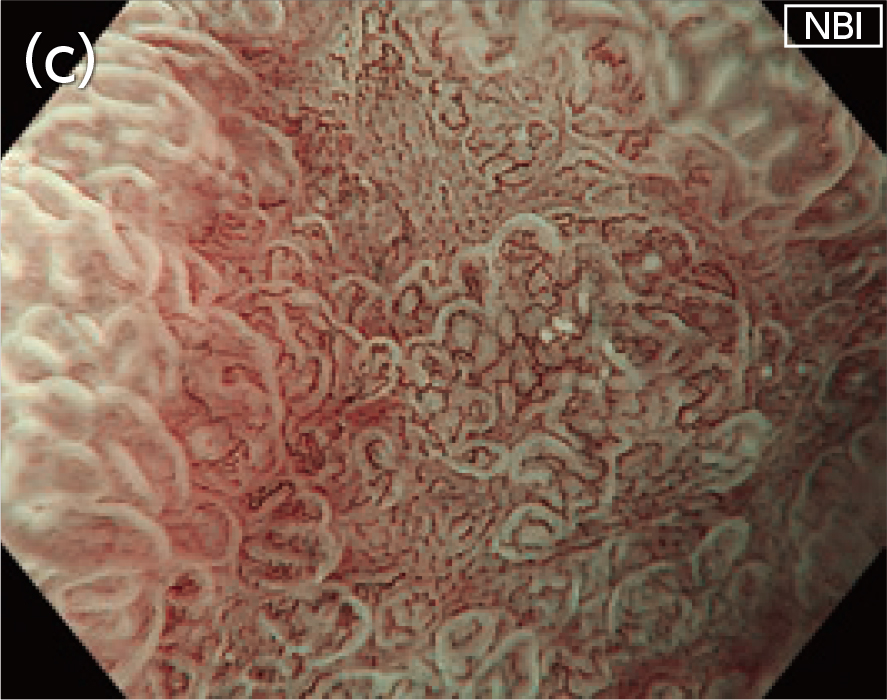
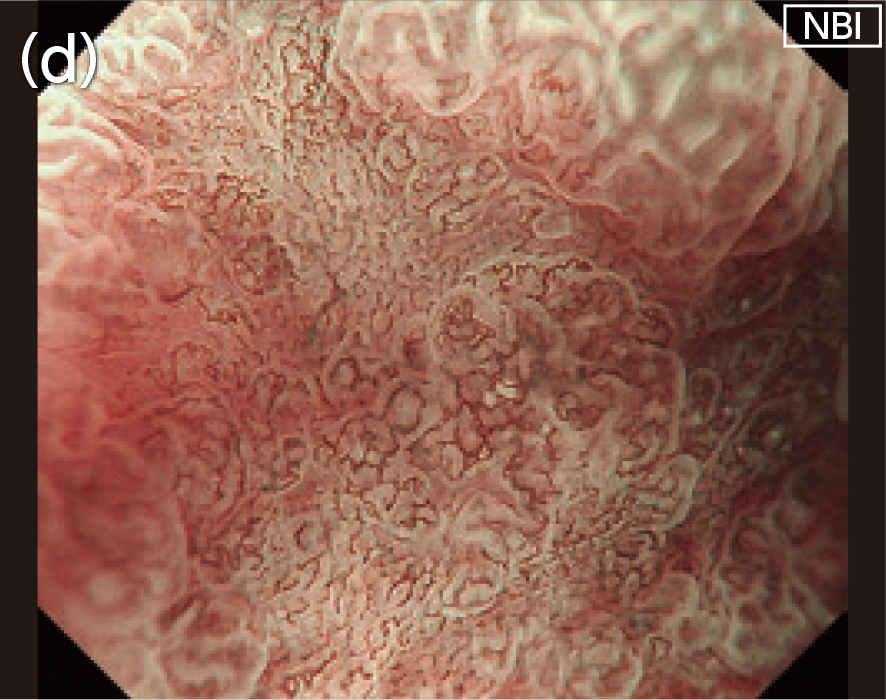
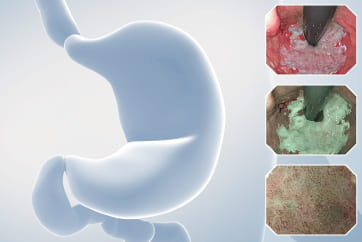
In patients with stage 0-IIc differentiated gastric cancer, TXI mode 1 enhances the redness and the clarity of surface unevenness, improving lesion visibility as compared to observation under WLI (Fig. 2). Under TXI mode 2, an image can be obtained that closely resembles one taken under WLI; however, I think that mode 1 is more advantageous for lesion detection because it emphasizes the color tone changes more clearly.
[Fig. 1] Images of a differentiated gastric cancer with flat elevation observed under WLI (a) and TXI mode 1 (b) Both white arrows: differentiated gastric cancer, blue arrows: submucosal tumor
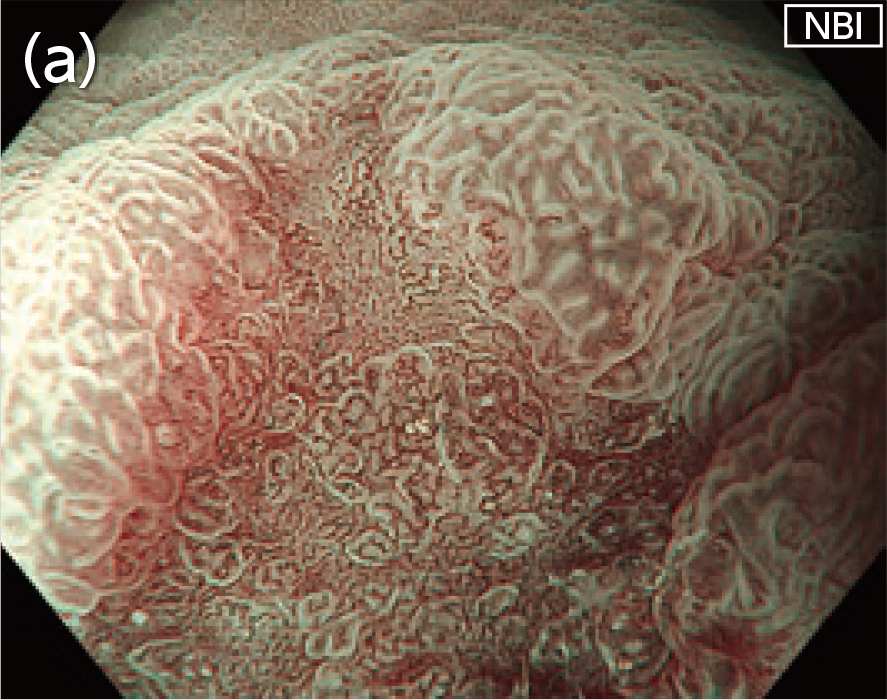
[Fig. 2] Images of 0–IIc differentiated gastric cancer observed under WLI (a), NBI (b), TXI mode 1 (c), and TXI mode 2 (d)
NBI is advantageous for flat lesions with little color tone changes under WLI, while TXI is advantageous for uneven lesions with clear color tone changes under WLI
In gastric cancer screening, NBI (narrow band imaging) has also been useful in detecting suspicious lesions. When comparing the performance of TXI and NBI, I find that TXI gives better visibility for such lesions that show slight surface unevenness and clear color tone changes, such as redness, under WLI (Fig. 2). In contrast, for lesions which are flat and exhibit little color change (such as discoloration) under WLI, I find that NBI provides superior visibility because those lesions can be clearly visualized and detected under NBI with a brown tone.
TXI and NBI have different characteristics. Thus, it is likely that the TXI and RDI technologies improve visibility for different types of lesions. Therefore, in the future, the verification and establishment of an appropriate combination of TXI and NBI in upper gastrointestinal cancer screening tests may lead to an improved lesion detection rate. For example, – based on the usage experience at present – a combined procedure (such as observing the pharynx and esophagus with NBI at the time of insertion, switching to TXI after reaching the stomach, and then switching to NBI and confirming once again) may become an established option. WLI and NBI are broadly used in the current screening test for early gastric cancer. We reported that the combined use of these two imaging methods could improve the detection rate of this type of cancer1). We hope that the benefit of the combination of TXI and NBI will be clarified in the future in a similar manner.
Using the EVIS X1 in combination with the GIF-EZ1500 upper gastrointestinal videoscope enables the use of EDOF, which is a depth- of-field expansion function that automatically obtains an image in which both the near and far points are in focus. This scope is equipped with the Dual Focus function that enables switching between the normal mode for observation in middle to long distance view and the near mode for close-up observation with a single button. Therefore, in use with EDOF, the GIF-EZ1500 allows easy focusing of endoscopic view regardless of non-magnifying or magnifying observation.
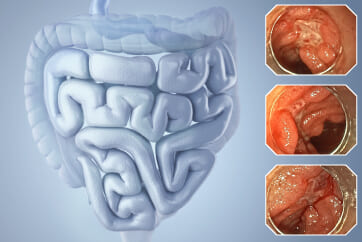
During the non-magnifying observation in middle to long distance view, this easy focusing will be useful in the detection of lesions in the area which requires a tangential approach (such as the esophagus). Expanded depth-of-field results in enlargement of the focused area in the endoscopic field of view, which possibly improves the lesion detection rate. Additionally, during close-up magnifying observation, images in which the entire endoscopic field of view is sharply focused on the elevated lesion can be easily obtained (Fig. 3). Therefore, it may be possible to narrow down the region of interest in a more efficient manner when wanting to observe closer at a higher magnification. However, in close-up magnifying observation, we should note that we need to approach towards the region of interest again from the exact frontal view for precise evaluation of the microvascular pattern and microsurface pattern.
[Fig. 3] Images of an elevated lesion taken in close-up magnifying observation with the EVIS X1 and the GIF-EZ1500
(a) Near mode with ~85x optical zoom;
(b) Near mode with ~85x optical zoom + 1.4x electronic zoom
Image quality of magnifying observation with additional electronic zoom in the GIF-EZ1500 near mode is close to that with a conventional manual zoom scope
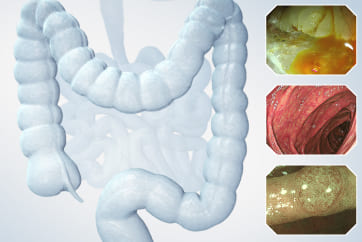
In the GIF-EZ1500 near mode close-up magnifying observation (Fig. 4a), there is an impression that its combined use with 1.4x (Fig. 4b) or 1.6x (Fig. 4c) electronic zoom makes it possible to obtain magnified images with the amount of information and similar image quality to the conventional manual zoom scope GIF-H290Z (Fig. 4d).
As for the procedure for the combined use, the observation is first made in the near mode, which provides an optical zoom with a maximum magnification of approximately 85x (when using the OEV262H), after which a 1.4x or 1.6x electronic zoom is used for qualitative diagnosis and borderline diagnosis. The 1.6x zoom is selected for more detailed observation. Even with this higher zoom magnification, we did not find degradation of the image quality caused by image granularity. It is expected that the combined use with electronic zoom would demonstrate diagnostic accuracy that is comparable to GIF-H290Z when conducting qualitative diagnosis or borderline diagnosis of early gastric cancer based on MESDA-G2).
[Fig. 4] Comparison of images taken in close-up magnifying observation with the GIF-EZ1500 at different magnification levels
(a) Near mode with 85x optical zoom;
(b) Near mode with 85x optical zoom + 1.4x electronic zoom;
(c) Near mode with 85x optical zoom + 1.6x electronic zoom;
(d) Reference image: 85x optical zoom in GIF-H290Z
Enabling a one-time endoscopic test from screening to detailed examination through a combination of the EVIS X1 and the GIF-EZ1500
The combination of the EVIS X1 and the GIF-EZ1500 will enable a one-time endoscopic test from screening for the detection of lesions to detailed examination (including qualitative/borderline diagnosis) while ensuring high diagnostic accuracy. This means that lesion detection with higher accuracy in the normal mode under TXI or NBI can be immediately followed by the qualitative diagnosis for the detected lesion with switching to near mode. A series of diagnostic steps can be conducted during a one-time endoscopic examination. EDOF makes it easy to obtain sharp, focused images regardless of non-magnifying or magnifying observation. Therefore, the GIF-EZ1500 in combination with the EVIS X1 seems to improve usability for endoscopists who are beginners in magnifying endoscopic observation or have some difficulties in operating a full-zoom magnifying scope. If, as a result of this modality, image-enhanced endoscopy (such as NBI and TXI) and magnifying observation in the Near mode become widely conducted from the screening examination stage, then further spread of magnifying endoscopic diagnosis is expected. This may lead to an improvement in the quality of endoscopic diagnosis and treatment.
In addition to TXI and EDOF, the EVIS X1 and the GIF-EZ1500 are equipped with several functions related to observation performance and operability, and their usability will change depending on how these operations are assigned to the touch panel and footswitches. It is important for each endoscopist to thoroughly examine the operation settings in advance and identify the most convenient ones, so that they can conduct optimal tests while making the most of the new functions.
The utilization of these technologies may promote the spread of magnifying endoscopic diagnosis and improve diagnosis of invasion depth for early gastric cancer
In the future, we need to evaluate the exact difference in the lesion detection rate of screening test between TXI installed in the EVIS X1 and conventional imaging (WLI and NBI). The level of accuracy ensured in the qualitative diagnosis of early gastric cancer with close-up magnifying observation in the GIF-EZ1500 near mode is also remained as an issue to be clarified. Furthermore, one expectable benefit of TXI observation is that texture enhancement will enable more accurate evaluation of the trapezoidal elevation findings in early gastric cancer, which may be beneficial in diagnosis of invasion depth. I expect that the accumulation of clinical experiences in using the EVIS X1 and the GIF-EZ1500 results in generation of clinical evidence for benefits of endoscopy using them, and that the generation of evidence leads to improvements in the quality of upper gastrointestinal endoscopy.
* Specifications, design and accessories are subject to change without any notice or obligation on the part of the manufacturer
1) Yoshida N, et al. Gut. 2021; 70:67-75.
2) Muto M, et al. Dig Endosc. 2016; 28:379-93.
Dr. Jae Young Jang Case 7: Two gastric neuroendocrine tumors (NET)
Dr. Khanh Do-Cong Pham
- Keyword
- Content Type