Introduction
Patients with biliary stenosis pose a challenge to gastroenterologists active in clinics. The draining bile ducts are divided into an intrahepatic, a perihilar and an extrahepatic part. A constriction in the bile duct that impairs the outflow of bile and leads to a consecutive dilation of the bile duct is called a bile duct stenosis. Etiologically, a distinction is made between benign and malignant bile duct stenoses, which require different diagnostic and therapeutic approaches. The most common causes of biliary stenoses are summarized in table 1.
The treatment of biliary stenoses is the domain of endoscopic retrograde cholangiography (ERC). The ERC can be used as a definitive endoscopic therapy, to bridge a gap leading to an operation or in a palliative setting. The implantation of self-expanding metal stents (SEMS), which can be used for therapy-refractory benign and malignant stenoses, is of particular importance. Other areas of application include the implantation in the event of bile duct injuries or leaks. A common problem with implanting SEMS, especially with coated SEMS, is stent migration or dislocation.1, 2
This case report describes the application of the innovative BMCL stent. With this completely coated
stent, the cover is provided with openings at various points, so that it is a hybrid version of a coated and uncoated stent. The incorporated openings are intended to help the stent to partially grow in, thus reducing stent dislocation. Since this kind of stent only grows in at certain points, it can still be removed. At the same time, the cystic duct can be drained through the openings that this stent provides.
Case Presentation — Treatment and Outcome
In the period between June 2019 and October 2020, the BMCL stent was implanted in different lengths in 12 patients. The technical success of implanting the SEMS was 100 % (12/12) without complications occurring. The most common indication was therapy-refractory benign bile duct stenosis with recurrent stone discharge (n = 5) or with chronic pancreatitis (n = 4). A completely coated SEMS was placed in 6 patients in advance, which afterwards dislocated in 4 patients.
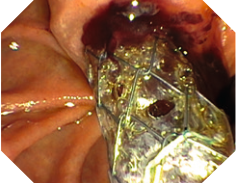
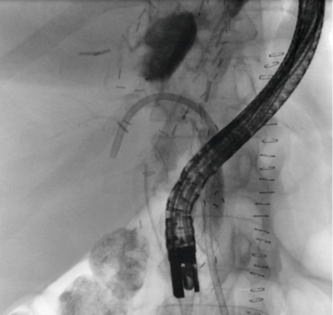
The other indications included a biliary leakage at the resection margin after left hemihepatectomy with distal biliary narrowing (n = 1) as well as the implantation of the BMCL stent via a transgastric bile duct access (BPD stent) in the case of stenosis at the hepatic bifurcation area (n = 1, patient request for stent removability). Another stent was placed in a patient with diffuse bleeding from biliary varices (n = 1). Figure 1 shows an example of the stent immediately after implantation.
Outcome
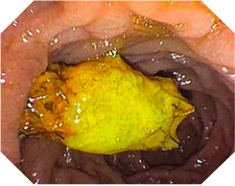
The stent was removed without problems in 9 of 10 patients after 3 to 6 months. The stent was removed with conventional grasping forceps. A hepatic bile duct bifurcation resection was performed in the further course of the patient treatment with the stent inserted transgastrally. No stent dislocation was detected during the observation period. In 2 patients (recurrent stone discharge), the distal end of the stent in the duodenum was clearly obstructed after 3 to 4 months, whereby the bile drainage in these patients was ensured through the openings in the cover in direct front of the insertion portion point to the major papilla (Figure 2).
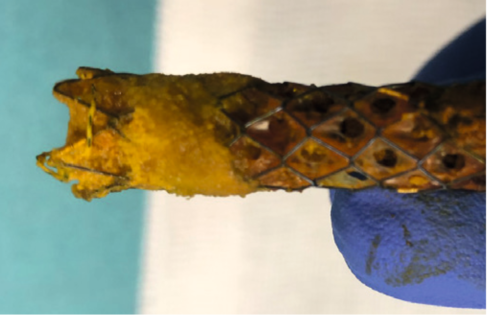
This stent area was not completely affected by the obstruction or deposition of lithogenic material (Figure 3).
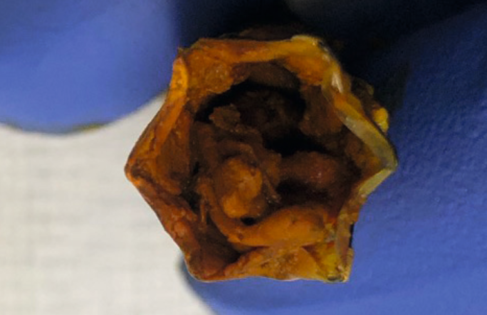
The cross section of the stent clearly shows that there has been significant deposition of sludge and concrement material with subtotal occlusion in the stent lumen (Figure 4).
There was no comparable change in the stent in the
other patients. In the patient with a biliary leak at the resection margin, the BMCL stent was placed with distal biliary narrowing in order to improve biliary drainage. A plastic stent was placed over the lying SEMS directed towards the intrahepatic position (Figure 5). After 3 months, the stents were removed without any problems and with no evidence of a persistent bile leak.
Summary
In summary, the implantation of the BMCL stent is user-friendly and was uncomplicated in this small case series. The innovative stent design appears to support the stent in maintaining its position. Without the presence of the openings, with complete stent obstruction, cholestasis-associated symptoms could have occurred in patients with recurrent stone discharge. Since this is not a controlled study setting, it cannot be conclusively assessed whether the stent design with the pores promotes the deposition of lithogenic material in the stent and thus the closure of the stent due to the changed biliary drainage.
There was no comparable change in the stent in the other patients. In the patient with a biliary leak at the resection margin, the BMCL stent was placed with distal biliary narrowing in order to improve biliary drainage. A plastic stent was placed over the lying SEMS directed towards the intrahepatic position (Figure 5). After 3 months, the stents were removed without any problems and with no evidence of a persistent bile leak.
This question will be evaluated in further studies. Nevertheless, the innovative BMCL stent expands the existing stent portfolio and helps to enable an individualized, patient-adapted therapy.
Table 1
Benign Biliary Stenoses
- Anastomotic stenosis after LTx
- Ischemic type biliary lesions after LTx
- Scarred stenoses after cholecystectomy
- Post radiogen
- Chemotherapy
Cholangiocarcinomas
Gallbladder carcinoma
Hepatocellular carcinomas
Major duodenal papilla carcinomas
Pancreatic cancer
Duodenal carcinoma
Chronic pancreatitis Lymphoma
Primary sclerosing cholangitis Metastases
- Ischemic / critically ill patients
- Medicinal / toxic
- Autoimmune (IgG4-connected, eosinophilic cholangitis)
- Recurrent cholangitis
Mirizzi syndrome
Choledochal cysts
Sarcoidosis
Infection-associated: Pericholedochal inflammation / abscesses AIDS (HIV-associated) cholangiopathy Tuberculosis, histoplasmosis
Quoted References
1Seo, D.W., et al. Covered and Uncovered Biliary Metal Stents Provide Similar Relief of Biliary Obstruction during Neoadjuvant Therapy in Pancreatic Cancer: A Randomized Trial. Gastrointest Endosc., 2019; 90(4):602-612.
2Xinjing Zhang et al. Effect of Covered Self-Expanding Metal Stents Compared with Multiple Plastic Stents on Benign Biliary Stricture: A Meta-Analysis. Medicine, 2018; 97(36):e12039.
As medical knowledge is constantly growing, technical modifications or changes of the product design, product specifications, accessories and service offerings may be required.
- Keyword
- Content Type