Background / Need for BPE / Indications
Since it was first described and performed in 2001, endoscopic ultrasound-guided biliary drainage (EUS-BD) has emerged as a valuable alternative procedure for achieving an endoscopic internal drainage in case of ERCP failure. Biliary drainage can be obtained by either a transduodenal extrahepatic approach through EUS-guided choledochoduodenostomy (EUS-CDS), or a transgastric intrahepatic approach, namely EUS-guided hepaticogastrostomy (EUS-HGS). We describe the case of a patient with locally advanced pancreatic cancer, jaundice and duodenal involvement successfully treated by EUS-HGS with placement of the newly designed HANAROSTENT BPE.
Patient Case & BPE Procedure
A 75-year-old male with locally advanced pancreatic cancer previously treated by ERCP with placement of a fully covered self-expandable metal stent (FC-SEMS), was referred to our centre due to jaundice recurrence, nausea and vomiting. An upper-GI endoscopy was carried out showing complete stricture of the duodenal bulb, thus making the papilla unreachable; an EUS-CDS was considered not feasable due to the extensive duodenal involvement: therefore, after multidisciplinary discussion, an EUS-HGS was planned.
By using an interventional echoendoscope, the left liver was visualized, and dilated hepatic bile duct was identified (Fig.1)
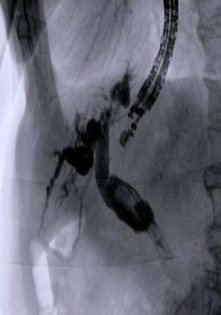
After puncturing the intrahepatic bile duct with a 19-gauge fine needle under combined fluoroscopic and ultrasound guidance, biliary tract opacification was obtained by contrast injection to confirm successful biliary access (Fig.2)
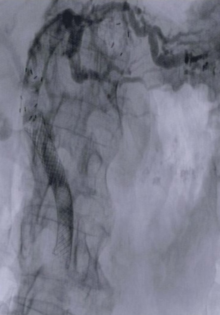
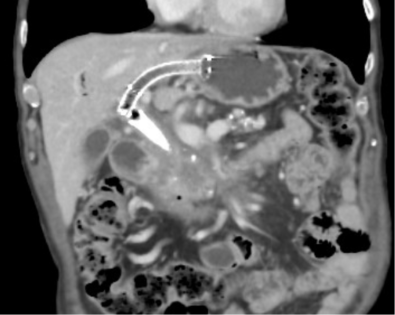
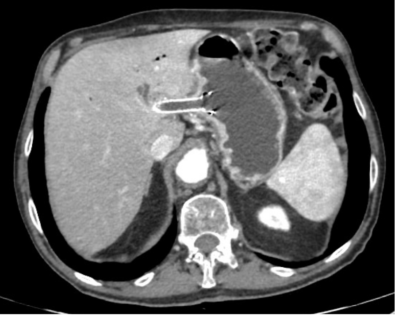
A 0.035-inch guide wire was gently manipulated and advanced into the biliary tree. An electrocautery dilation with a 6F cystotome was performed in order to allow insertion of the dedicated stent. Finally, under radiological and endoscopic control a 10x80mm HANAROSTENT BPE with an uncovered intra-hepatic end and antimigratory systems was placed using the intra-channel release technique. The rapid outflow of bile (Fig. 3) and contrast medium confirmed the correct placement of the stent (Fig. 4, 5, 6).
Background / Need for BPE / Indications
Since it was first described and performed in 2001, endoscopic ultrasound-guided biliary drainage (EUS-BD) has emerged as a valuable alternative procedure for achieving an endoscopic internal drainage in case of ERCP failure. Biliary drainage can be obtained by either a transduodenal extrahepatic approach through EUS-guided choledochoduodenostomy (EUS-CDS), or a transgastric intrahepatic approach, namely EUS-guided hepaticogastrostomy (EUS-HGS). We describe the case of a patient with locally advanced pancreatic cancer, jaundice and duodenal involvement successfully treated by EUS-HGS with placement of the newly designed HANAROSTENT BPE.
Patient Case & BPE Procedure
A 75-year-old male with locally advanced pancreatic cancer previously treated by ERCP with placement of a fully covered self-expandable metal stent (FC-SEMS), was referred to our centre due to jaundice recurrence, nausea and vomiting. An upper-GI endoscopy was carried out showing complete stricture of the duodenal bulb, thus making the papilla unreachable; an EUS-CDS was considered not feasable due to the extensive duodenal involvement: therefore, after multidisciplinary discussion, an EUS-HGS was planned.
By using an interventional echoendoscope, the left liver was visualized, and dilated hepatic bile duct was identified (Fig.1)
After puncturing the intrahepatic bile duct with a 19-gauge fine needle under combined fluoroscopic and ultrasound guidance, biliary tract opacification was obtained by contrast injection to confirm successful biliary access (Fig.2)
A 0.035-inch guide wire was gently manipulated and advanced into the biliary tree. An electrocautery dilation with a 6F cystotome was performed in order to allow insertion of the dedicated stent. Finally, under radiological and endoscopic control a 10x80mm HANAROSTENT BPE with an uncovered intra-hepatic end and antimigratory systems was placed using the intra-channel release technique. The rapid outflow of bile (Fig. 3) and contrast medium confirmed the correct placement of the stent (Fig. 4, 5, 6).
Outcome
The patient was discharged 4 days after the procedure, with bilirubin values decreased by half compared to the admission. A second-line chemotherapy treatment was started. The patient had no recurrence of jaundice in the last 4 months.
Summary
EUS-HGS is emerging as a possible therapeutic alternative when an endoscopic internal biliary drainage is otherwise impossible. Nowadays, EUS-HGS still remains a complex procedure that must be conducted by very experienced endoscopists in interventional EUS and ERCP procedures only in referral centres. However, with standardization of the technique and the introduction in clinical practice of dedicated devices (e.g. HANAROSTENT BPE) EUS-HGS may become one of the cornerstones of EUS-BD.
As medical knowledge is constantly growing, technical modifications or changes of the product design, product specifications, accessories and service offerings may be required.
- Content Type