Step-by-step technique for laparoscopic segment 8 segmentectomy.
1) Positioning the patient, positioning the trocars
The patient is placed on their back with their legs apart and a little bent. The hemithorax is raised with cushions placed under the right shoulder and the left arm held in a splint above the head. Counter-supports are placed on either side of the torso, especially at pelvis level, in order to allow the table to be tilted to the right for the initial dissection, when the surgeon stands between the legs and the assistant on the right or left. Then the table is tilted to the left when the surgeon comes to the right side with the assistant placed between the legs.
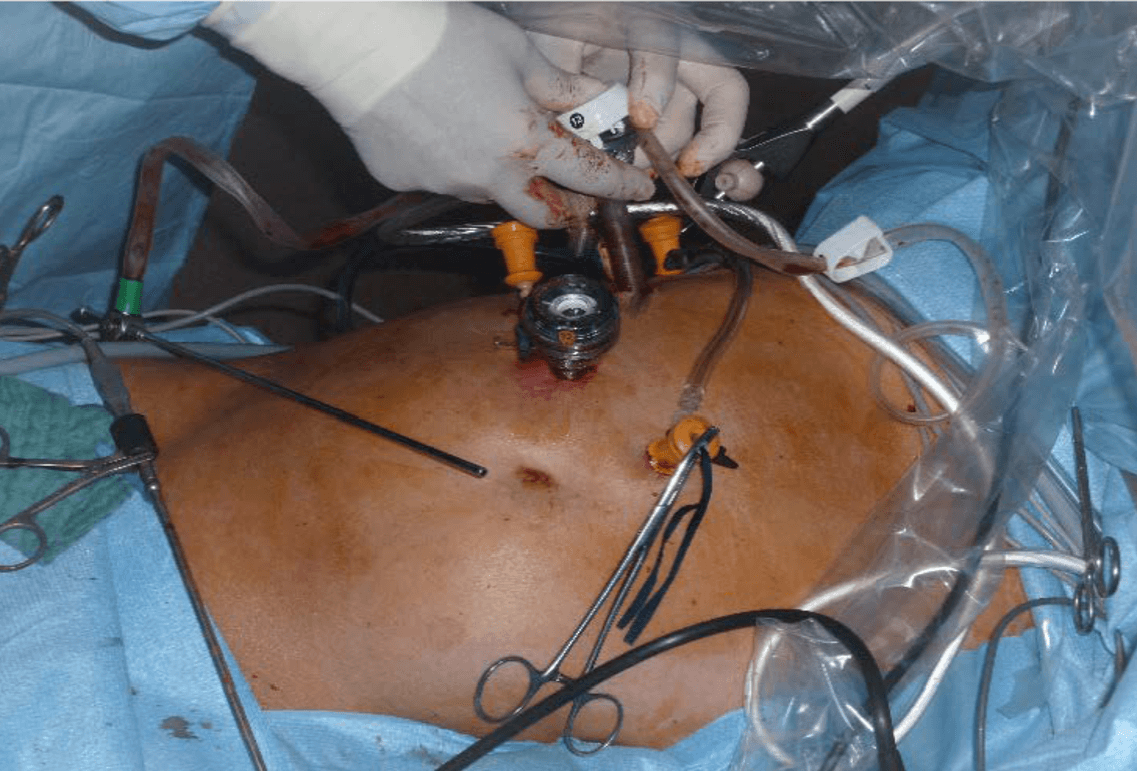
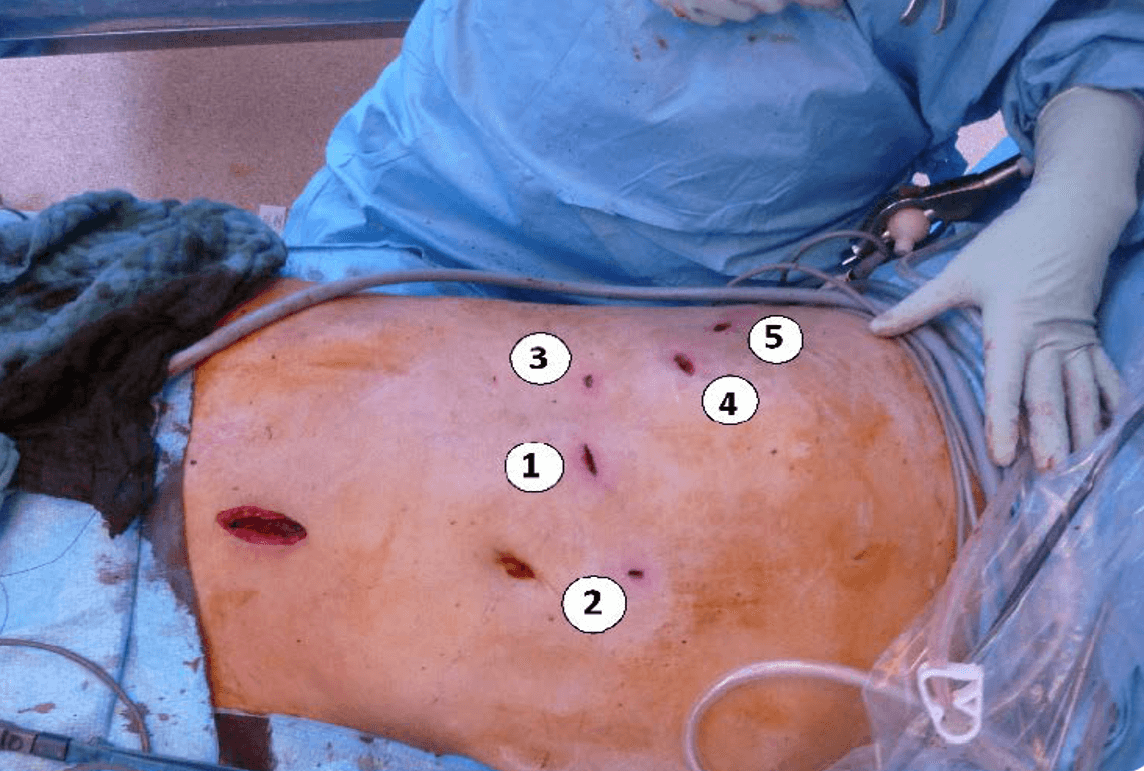
Five trocars are used (two 12 mm and three 5 mm) with the option to add another 5 mm trocar in case of exposure difficulty. To begin the intervention, three of these are positioned in the abdomen parallel with the costal margin at a height dependent on the hepatic volume, and if required, two are then positioned in the intercostal area – one 12 mm usually in the 7th space to be decided after mobilization of the liver. These two trocars are inserted under the control of the endoscopic view by pushing the diaphragm upwards to facilitate introduction. We use balloon foam trocars at this level to avoid pneumothorax. If this occurs nevertheless, a small angiocatheter placed in the pleura is left open during the entire operation to prevent ballooning of the diaphragm. The 12 mm trocar is used for ultrasound scanning and for the possible positioning of large 10 mm or 12 mm clips at the beginning of the procedure and for the laparoscope during the second stage of the resection.
2) Techniques for minimizing bleeding
Before starting the resection of segment 8, the surgeon must ensure they are operating on the “dry side” with minimal filling, ideally less than 500 ml intravenous, with ventilation pressure as low as possible. Finally, a system is placed around the hepatic pedicle allowing for global clamping in case of a hemorrhage that is difficult to control by compression. We use a percutaneous cotton tape so that the assistant can clamp it from outside the body. In this case, it is an intermittent 15-minute clamping with 5-minute revascularization intervals. For certain 8 segments with a large volume, the hepatic pedicle can also be dissected, the anterior pedicle can be followed intrahepatically, and selective clamping of the pedicle of segment 8 can be performed. In the case of intraoperative bleeding, it will be possible to have a positive end-expiratory pressure (PEEP) removed or even ventilation stopped for a minute or two. After intraoperative dye injection, by ICG using an infrared camera, this selective clamping also makes it possible to identify the real, and not just theoretical, boundaries of segment 8 or a sub-segment as appropriate.
3) Liver mobilization
The abdominal exploration and a possible lymphadenectomy are performed according to the usual technique with the patient placed in the Anti-Trendelenburg position with the head in the air. The liver mobilization begins at the right part of the coronary ligament without losing sight of the inferior vena cava (IVC). The accessory veins must be dissected and coagulated. Apart from an anatomical variation in the form of a large accessory vein of more than 8 mm which is then doubly clipped or tied by a crimped thread, we always use THUNDERBEAT for coagulation and then cutting without ever having a single recurrence of bleeding. We do not use “single” clips on the IVC anymore because they are easy to tear off when inserting instruments or during surgical maneuvers, and it is easy to fail to notice bleeding that may sometimes be very severe because the patient’s head is up.
4) Means of exploration: preoperative liver reconstruction, IR-ICG visualization, ultrasound
A thorough analysis of the liver before surgery is essential, and MRI is now an indispensable examination. For complex cases, we systematically carry out a 3D analysis with reconstruction and hepatic volumetry using dedicated Vincent software. We can thus know if we are dealing with a single, double or even triple segment 8. Using an injection of ICG the day before surgery, it is also possible to get an infrared image of the tumor or its periphery during the procedure. Intraoperative ultrasound is essential except in the case of small superficial lesions. It is necessary to define the boundaries of the tumor, but also the connections to the numerous vessels at this level: The IVC, the portal pedicle or pedicles in the case of sub-segments and the two V8 that flow one into the median hepatic vein (MHV), the other into the right hepatic vein (RHV). The projections of these structures can be marked on the liver capsule.
5) Surgical strategy for an anatomical segmentectomy of segment 8
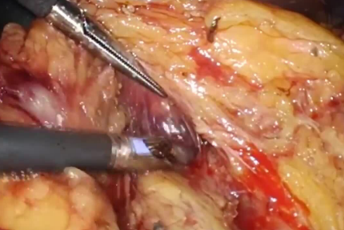
(a) The surgeon starts with a hepatic dissection between S4a and S8 from bottom to top until they find the MHV identified by the ultrasound. THUNDERBEAT is then very slowly used in cutting mode without trying to speed up the cutting by excessive pressure. To follow the vein, it is possible to use an ultrasound dissector. Here too we prefer to keep the THUNDERBEAT using it open, in small strokes, without pressing the vein with very brief bipolar coagulations on the small holes oozing blood. At the top of the cutting plane, we discover the left V8, go around, clamp it, and we can then fuse it using THUNDERBEAT and section. The dissection is continued backward and to the right towards the IVC to release segment 8 of the IVC up until the ending of the RHV that is spotted.
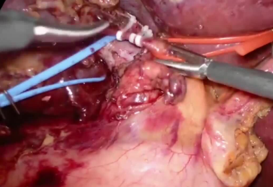
(b) Then change the cutting plane starting from the bottom and going horizontally to the left to find, fuse and cut the portal pedicle, and therefore the vessels or ducts P8, A8 and B8. The same technique is used combining THUNDERBEAT and bipolar coagulation for a dissection that is as dry as possible.
(c) Depending on the volume of segment 8, its release can be completed by going back to the IVC and the RHV. It is also possible to go further to the right, and in this case the surgeon goes to the right side of the patient and using trocars 3, 4 and 5, the surgeon completes the hepatotomy no longer from the bottom to the top, but starting from the top and actually from the RHV to dissect, fuse and cut the hepatic vein 8 that flows into the RHV (right V8). It is then necessary to finish the resection of segment 8 by following the RHV from top to bottom.
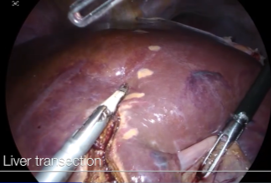
6) Parenchymal transection using the Clamp-Crush technique
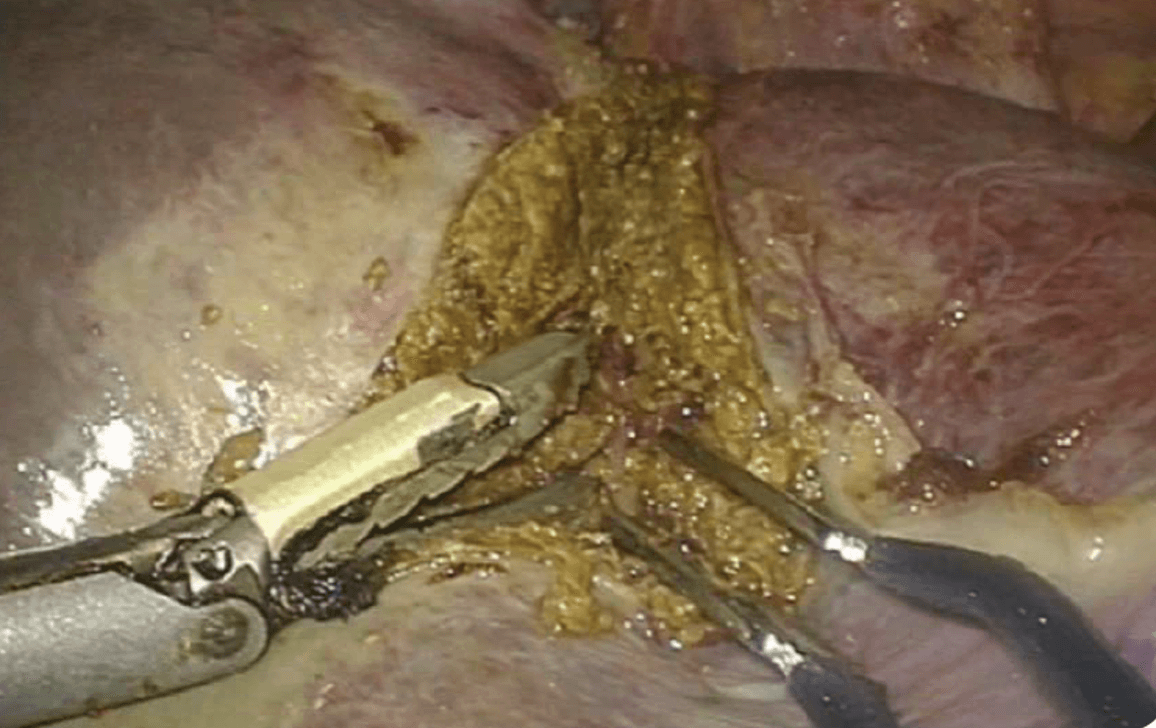
Neither of these techniques is superior to the other according to the literature, and each surgeon adopts the one that suits him. After we started using THUNDERBEAT, we gradually abandoned the other tools used until then – in our case Surgitron™ and Ligasure™. Currently, apart from dissectors (right angle), vascular clamps or needle holders that are always ready to be used, we perform the entire dissection with 3 tools: THUNDERBEAT, a suction unit with a foam tip and a bipolar forceps that we have designed with parallel jaws that we also use as forceps. This suction unit helps maintain a clear field during hemostasis, and sometimes it helps when following vessels by using gentle suction to dissect them upon contact like a ultrasonic surgical aspirator, but without irrigation that tends to contaminate the optics. Small bleeds are controlled with bipolar energy using either the dedicated clamp or the half-open THUNDERBEAT and placed laterally on the tissue. Bleeding in a vessel that has retracted into the parenchyma and persists after a haemostasis attempt is treated by applying a small fibrillated Surgicel nugget held in compression for approximately 1 minute. We no longer use glue, but we sometimes use Tachosil™ hemostatic compresses for people who are frail or who are to undergo post-operative anticoagulant treatment when large dissection sections are not absolutely dry.
No systematic drainage regardless of the intervention. This is reserved for patients who have bled over 600 cc or who have had a biliary suture or patients who have a highly pathological liver, for example after long-term chemotherapy or severe non-alcoholic steatohepatitis (NASH).
Optimal Instrument for Laparoscopic Liver Resections:
THUNDERBEAT is an excellent instrument especially for laparoscopic liver resections because it can be used to fuse and cut in the same procedure or – and this is essential in liver surgery – only to fuse without cutting which makes it possible to see the relevant structures properly before cutting them. With good training, it can also be used to dissect the tissues in the manner of an ultrasonic dissector without using water which can easily cause contamination of the laparoscope. This is especially true with a 3D camera (ENDOEYE Flex 3D) whose lenses are smaller and easily obscured by the slightest projection.
In the case of oozing, the possibility of using the THUNDERBEAT for bipolar coagulation with the open jaws in contact with the tissue makes it possible to maintain a clearer and drier operating field. It is therefore a versatile instrument that removes the need to insert and remove different instruments and thus reduces the risk of visceral or vascular wounds for each entry. Finally, coupling with an automatic suction unit at each device actuation rounds out its qualities by suppressing vapor, which is often a cause of visual and general fatigue for the surgeon in liver surgery, leading to unnecessary time wasted waiting for its dissipation.
Ref. 1 – Kawaguchi Y, Fuks D, Kokudo N, Gayet B. Difficulty of Laparoscopic Liver Resection: Proposal for a New Classification. Ann Surg. 2018 Jan;267(1):13-17
- Content Type