Case : Tumor in the right upper lobe
Kei Morikawa, MD
Division of Respiratory and Infectious Diseases,
Department of Internal Medicine
St. Marianna University School of Medicine
Scope: BF-1TH1200
Location: Right upper lobe
Patient information: Male, 66 years old
Medical history: Angina pectoris (treated with PCI), stroke, and heavy smoking (40 cigarettes per day). For past 3 months, he has experienced swelling in the right upper limb and increased difficulty in breathing during exertion. Two weeks ago, he coughed up blood and went to a nearby clinic, where a chest X-ray revealed a mass shadow in the right upper lung field. He was then referred to our institution for further examination.
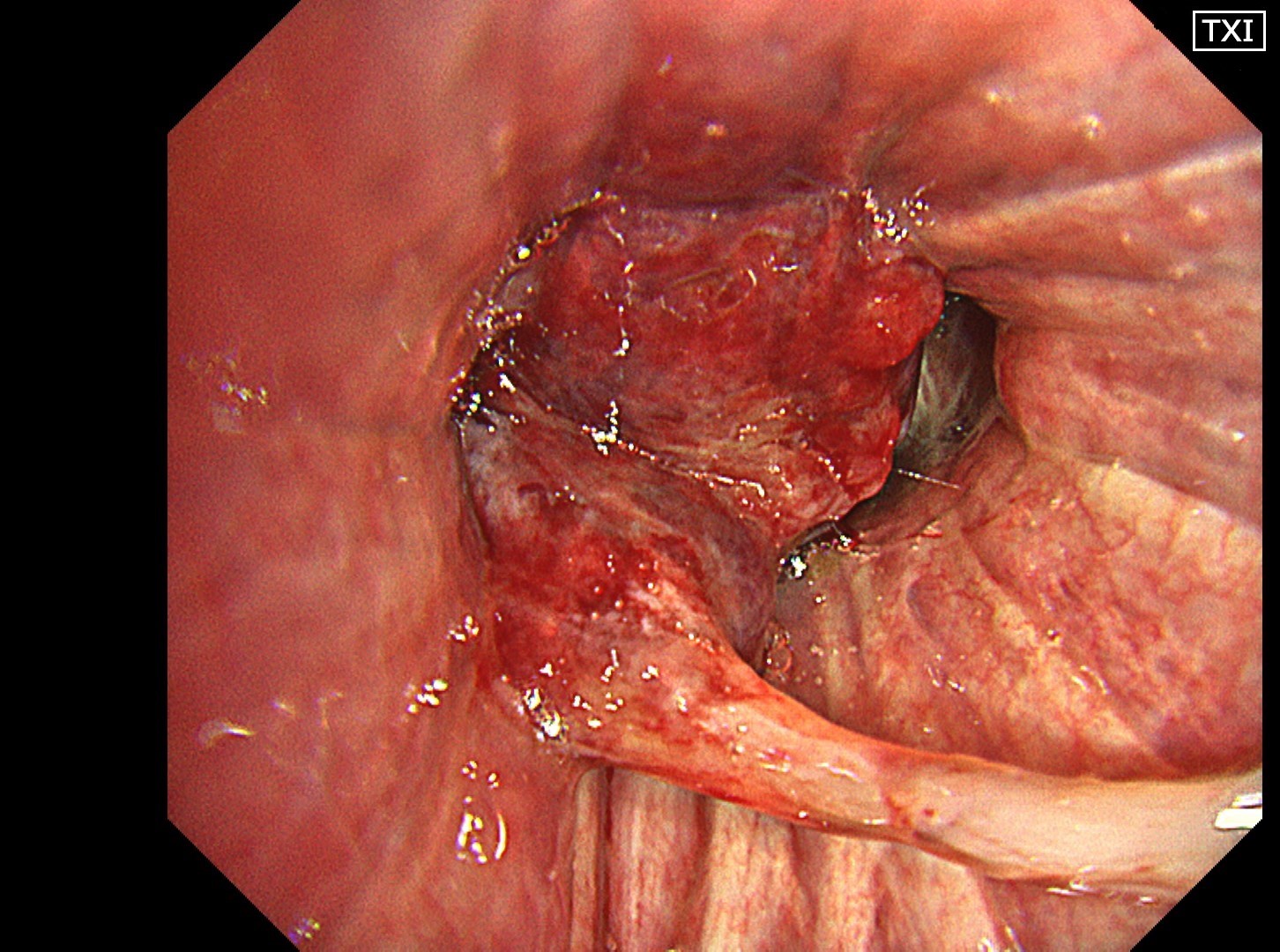
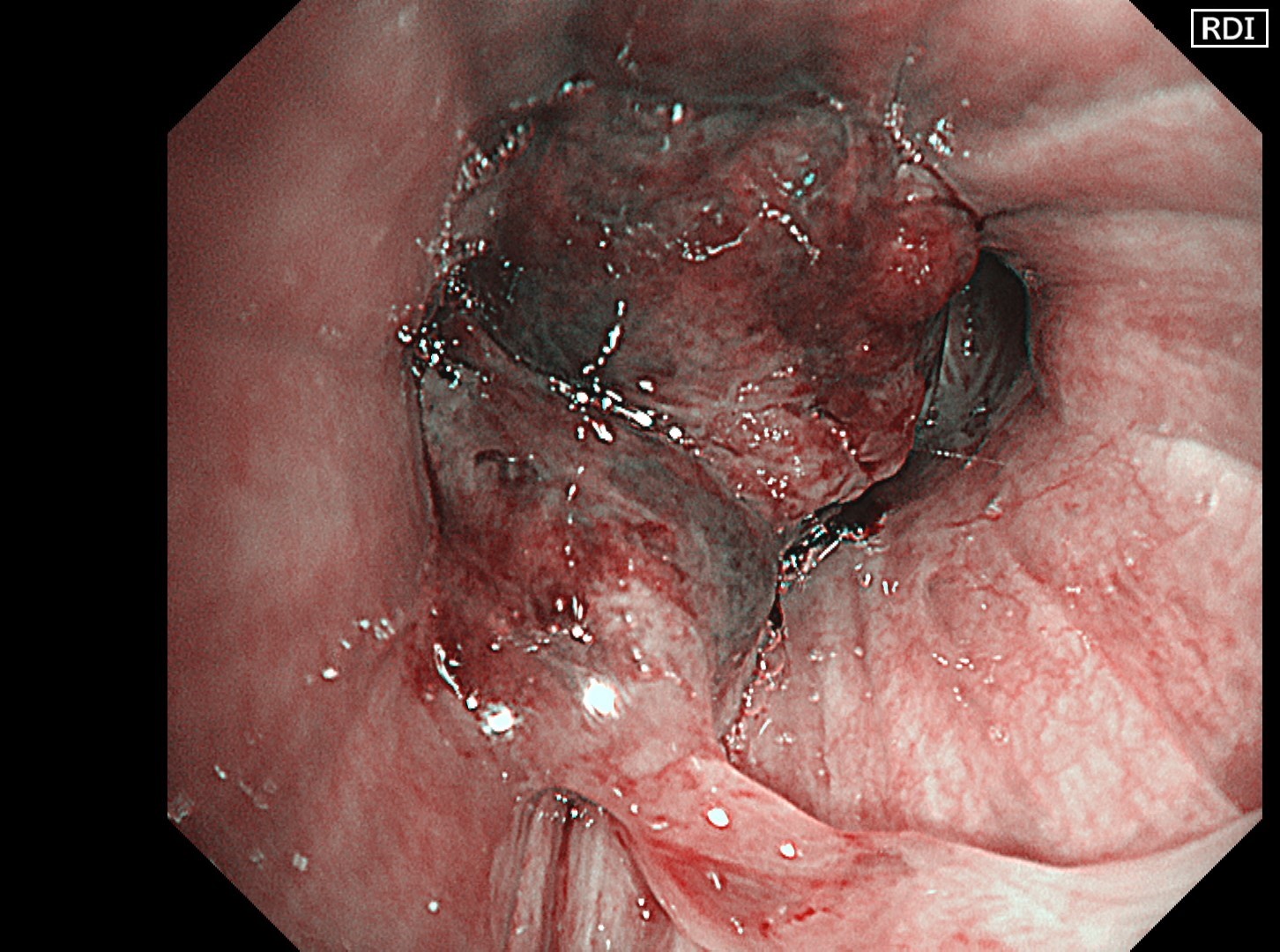
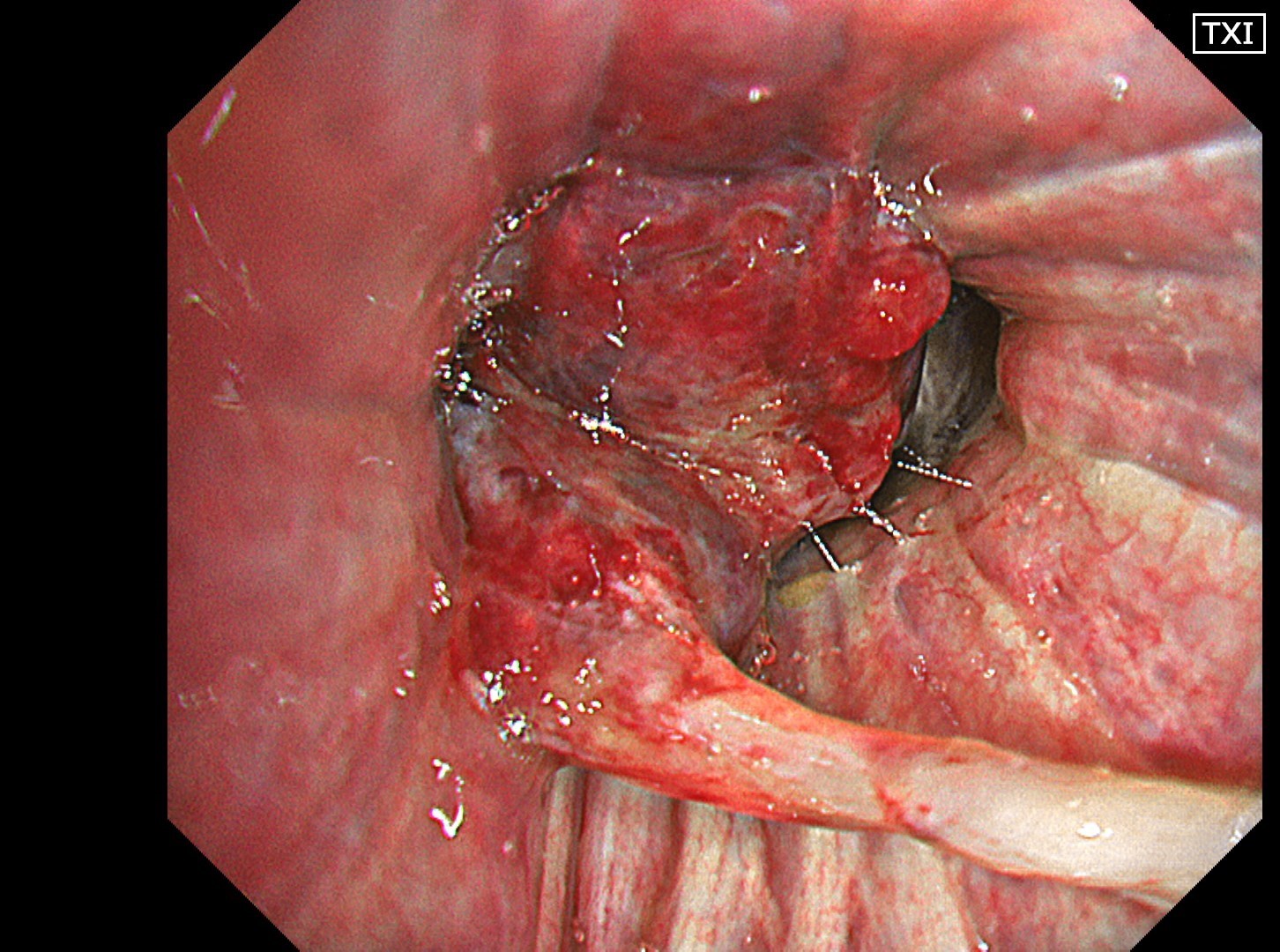
1-1 Right upper bronchus (WLI)
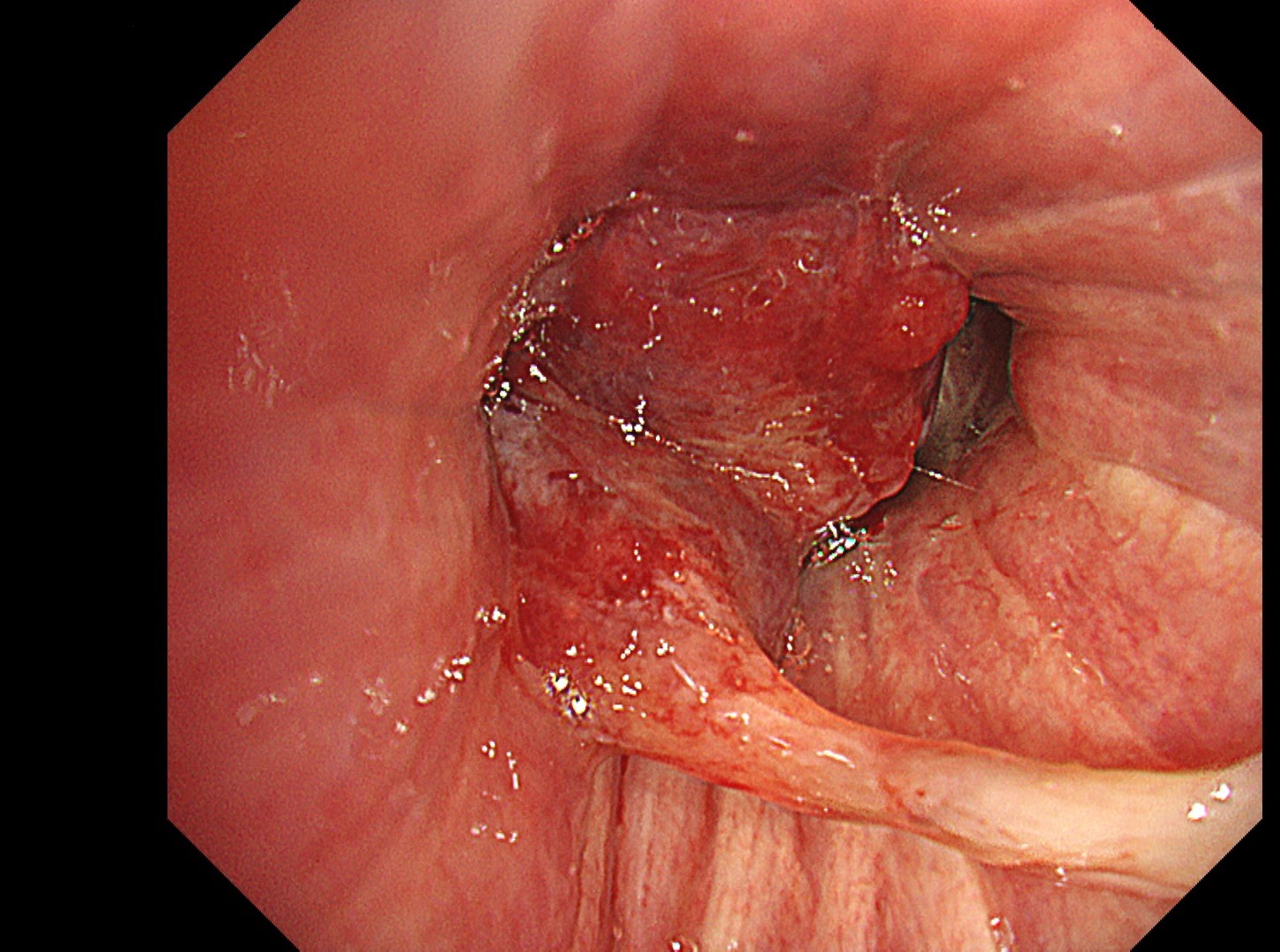
1-2 Right upper bronchus (TXI 1)
Case Video
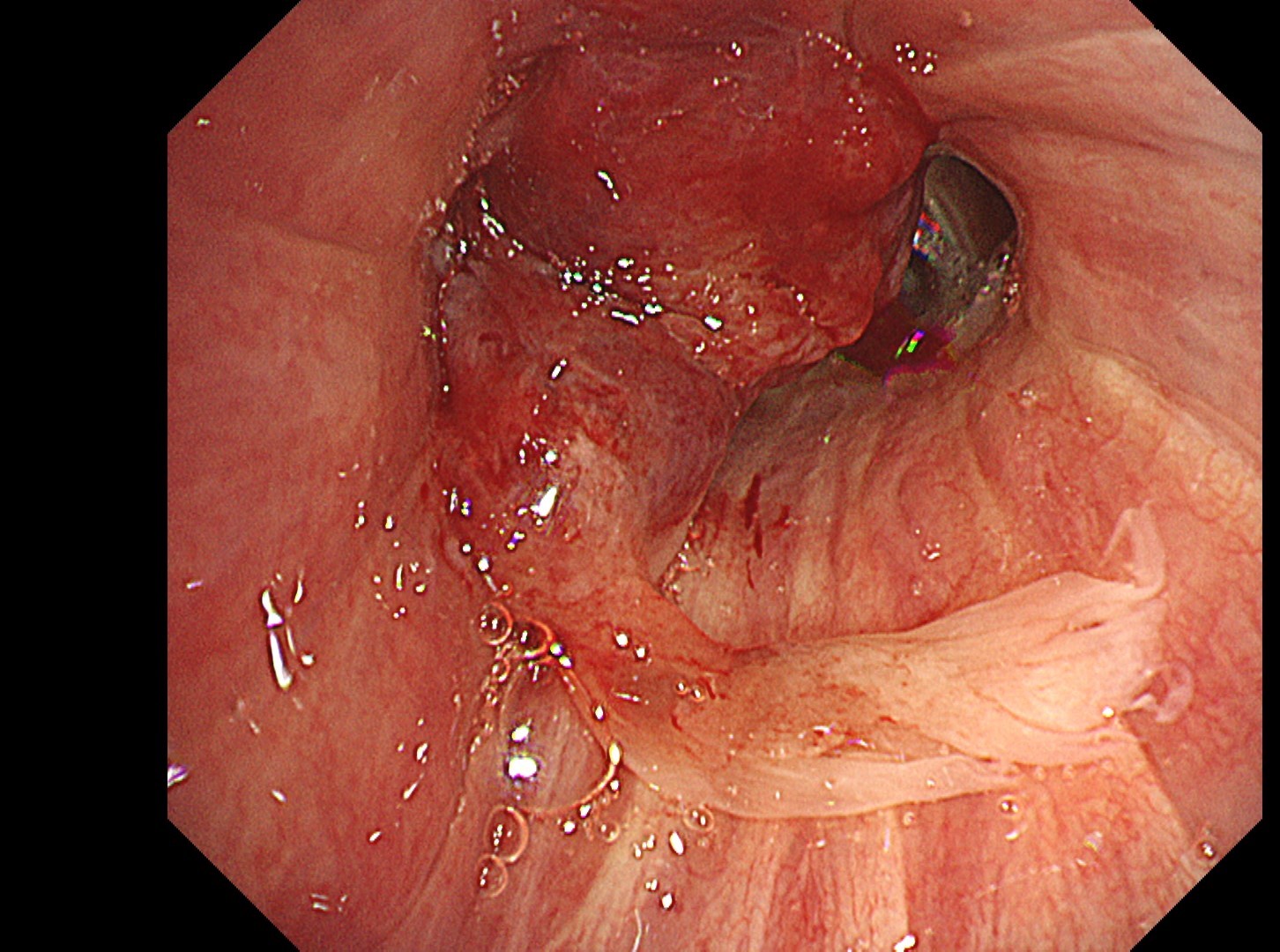
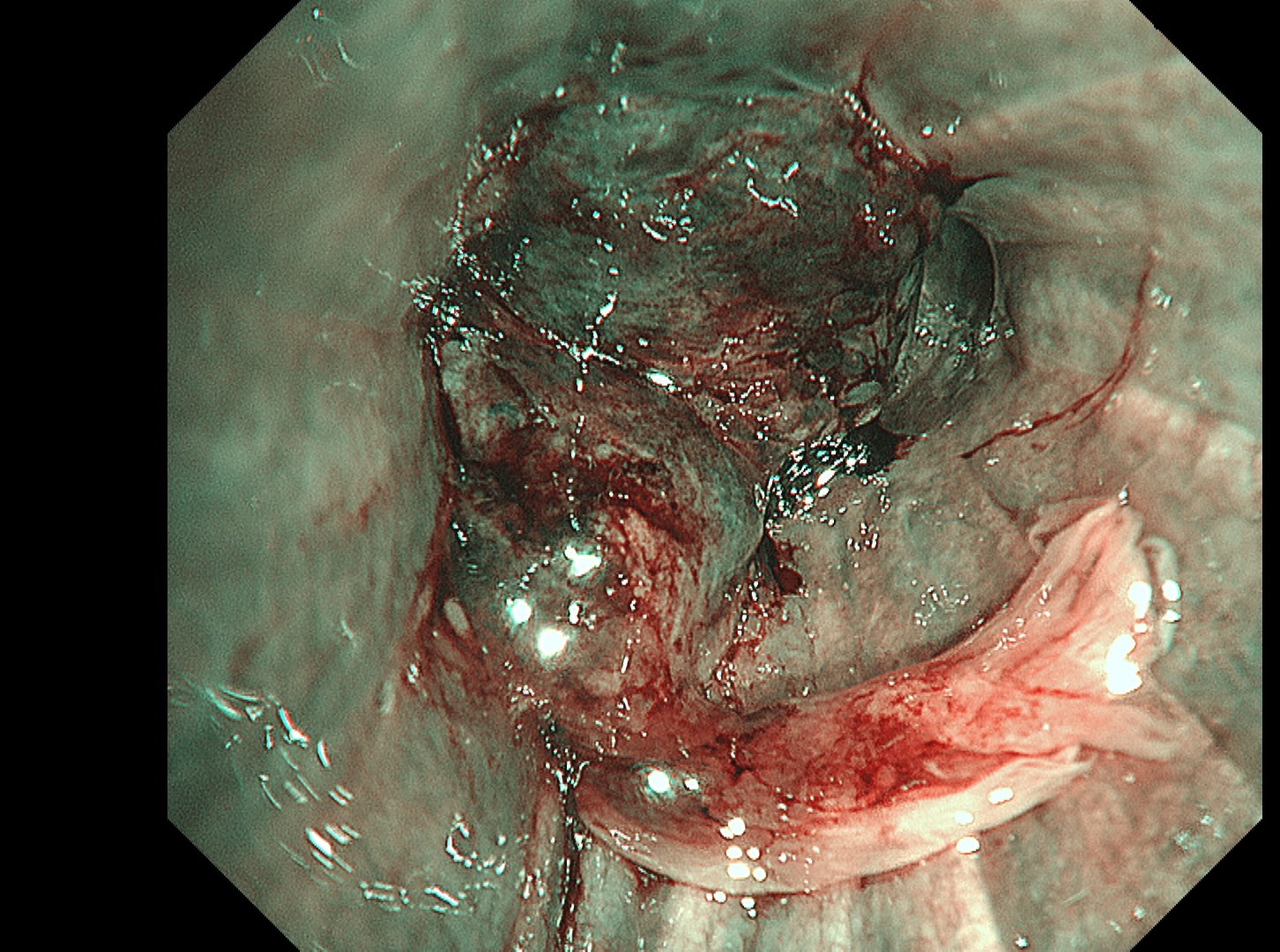
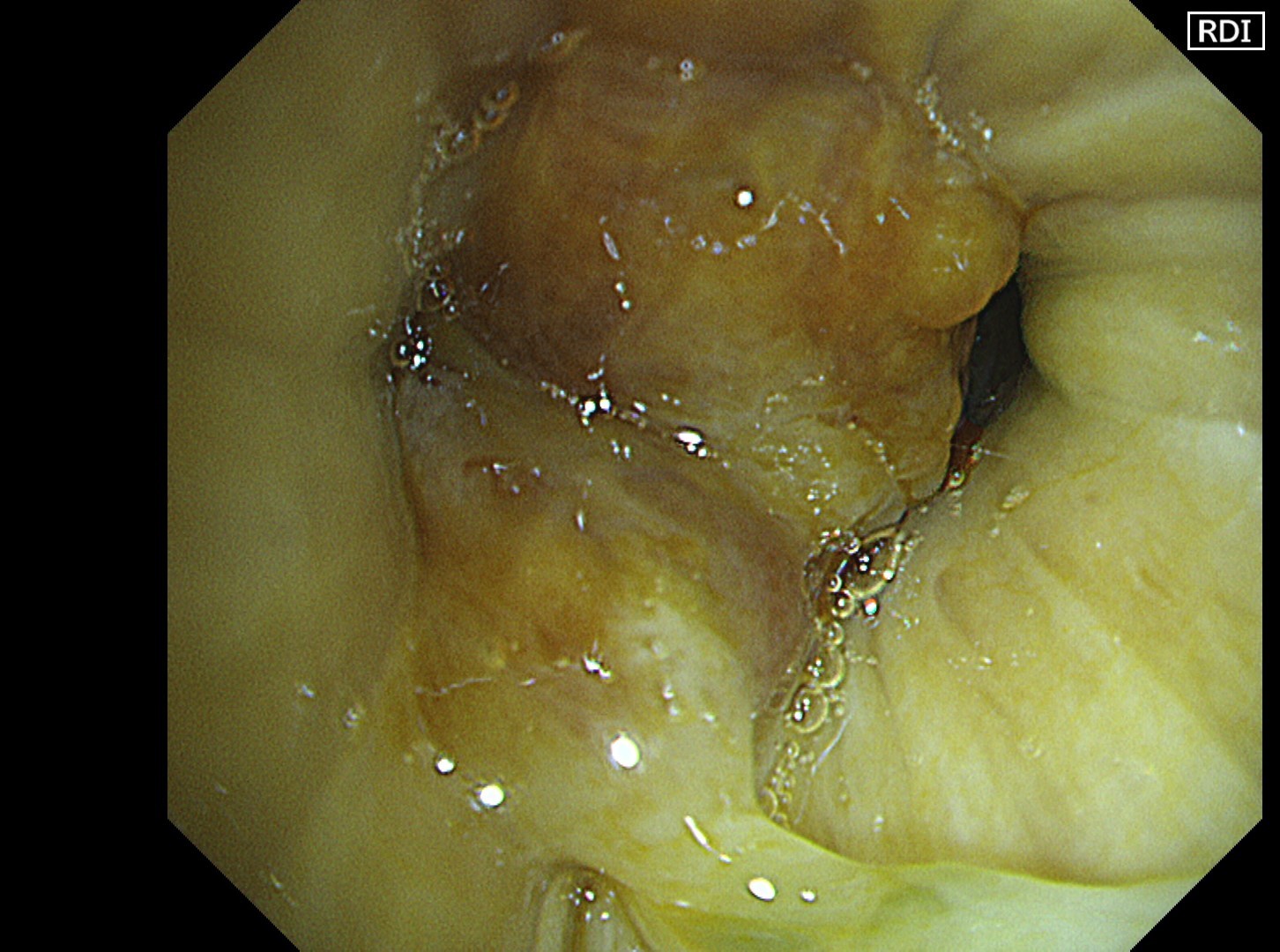
Using a spray catheter, the vocal cords are anesthetized under direct observation with the endoscope while the scope is advanced. The right upper lobe branch, which is the target of this examination, has a tumor growing in a polypoid fashion and protruding accompanied by distal necrosis. Although the subepithelial vessels of the tumor are unclear, the localization of the tumor blood flow can be estimated in NBI and RDI observation — which leads to the removal of necrotic tissue and subsequent collection of samples from the main body of the tumor.
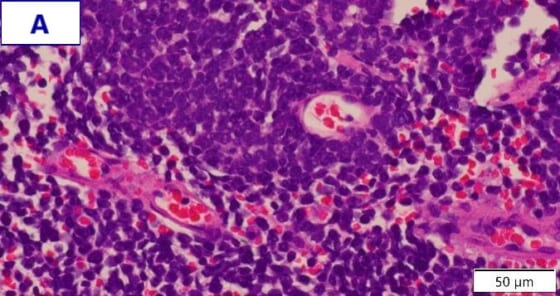
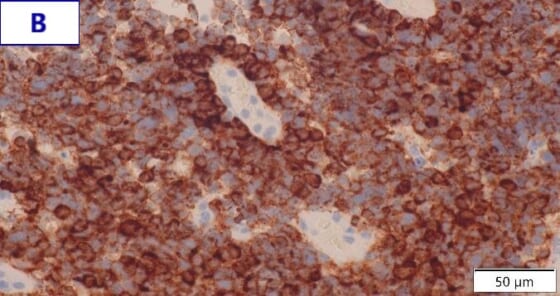
Pathological Findings
- Figure A (HE staining): Dense proliferation of small, round tumor cells can be observed. The cells have bare nuclei and sparse cytoplasm with delicate nuclear chromatin and indistinct nucleoli.
- Figure B (chromogranin A immunostaining): Tumor cells show expression of chromogranin A, which is a neuroendocrine marker.
- Final diagnosis: Primary lung cancer (small cell lung carcinoma)
Overall Comment
Dense proliferation of tumor cells made it difficult to observe subepithelial vessels. However, it was possible to evaluate the local blood flow of the tumor in NBI and RDI observation in addition to white light observation. This facilitated removal of necrotic tissue and subsequent biopsy. When a biopsy is performed, selection of an optimal site is important from a safety standpoint when using ROSE in combination. Thus, it may be useful to evaluate a site of particular interest in a multifaceted manner using various modes with different characteristics and then check for consistency between the findings produced by each mode.
Co-editor:
Dr. Nobuyuki Ohike
Department of Pathology, St. Marianna University School of Medicine
- Content Type