Scope: BF-H1200
Patient information: Male, 78 years old
Medical history: Known metastatic NSCLC and concomitant mycobacterium abscessus colonization near the primary at lingular segment. On second-line line gemcitabine-platinum doublet with good response.
Reason for bronchoscopy:
Differential radiological responses to chemotherapy over lingular shadows. Bronchoscopy was arranged to differentiate between disease progression vs. mycobacterium infection.
Known LMB orifice tumor partially covering the LLL opening.
New tumor nodule noted over LC (between LB1+2 & LB3) – biopsied
Foreign body seen inside LB3a (between LB3ai & LB3aii) – removed
LB3c pEBUS-GS TBBX performed according to pre-procedural planning.
Diagnosis:
LC (between LB1+2 & LB3) EBBX biopsy – Suspicious of malignancy
LB3a (between LB3ai & LB3aii) foreign body analysis – Consistent with bone, foreign in nature
LB3c TBBX biopsy – Suspicious of malignancy
Culture (BAL & LB3c TBBX): No growth of Mycobacterium
Treatment:
Continue with chemotherapy treatment
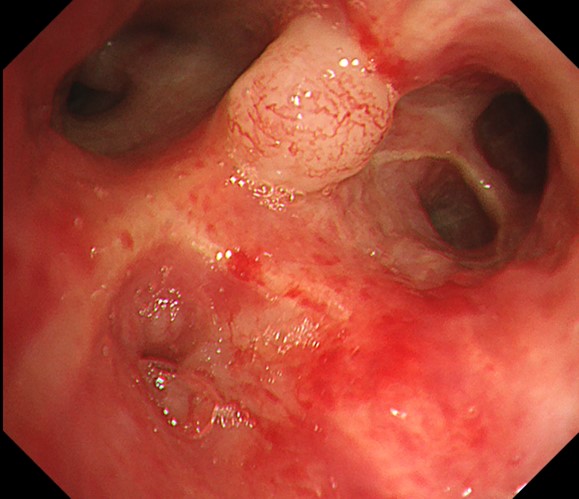
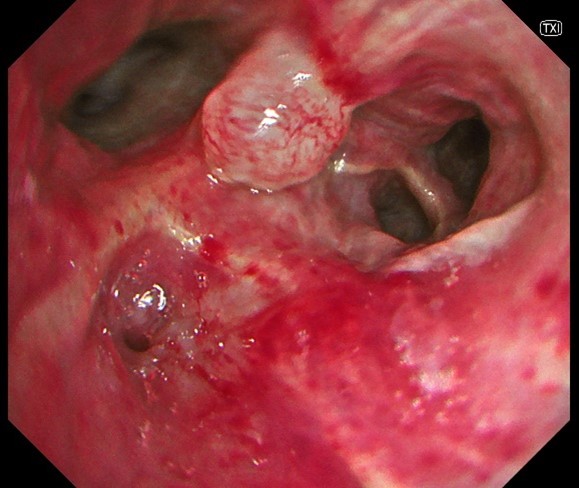
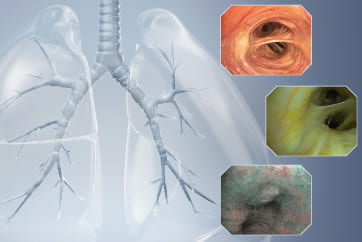
1. WLI vs. TXI observation
Generalized mucosal changes at 6 o-clock position over this short segment of LUL bronchus extending to the orifice of LB1+2c. The irregularities were much more appreciable with the use of TXI imaging.
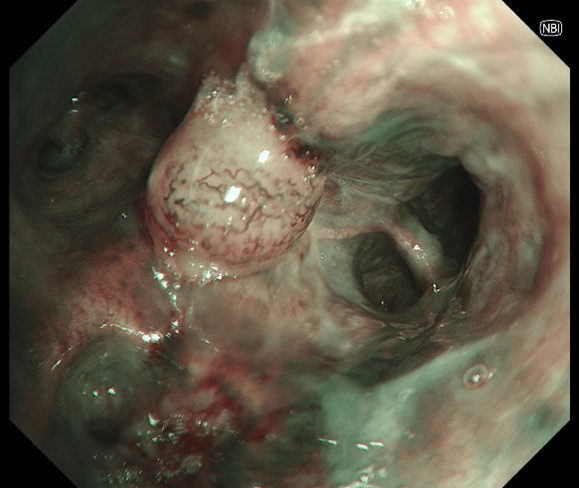
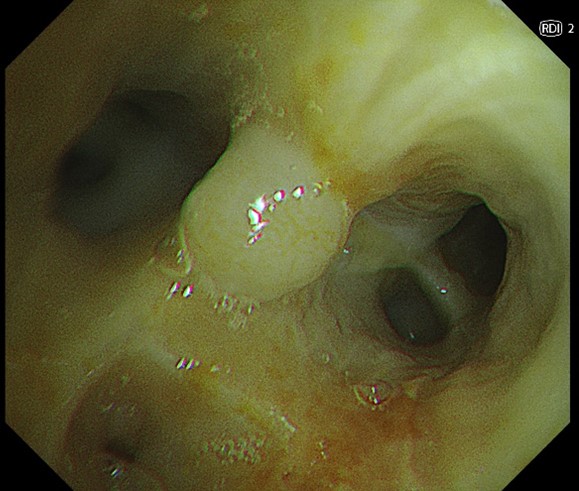
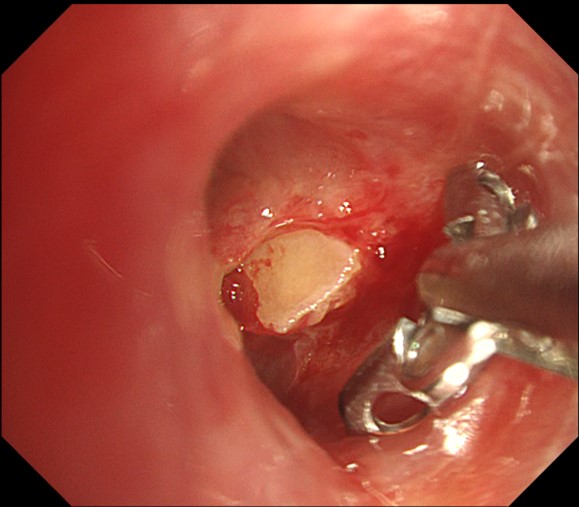
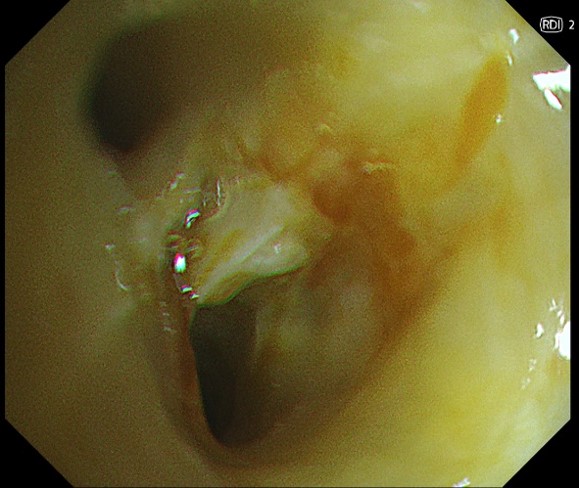
2. NBI vs. RDI observation
New tumor nodule over LC (between LB1+2 & LB3). NBI showed significant neo-vascularization, but the lack of deeper mucosal vessels on RDI over the central part of the nodule help assure that EBBX is safe.
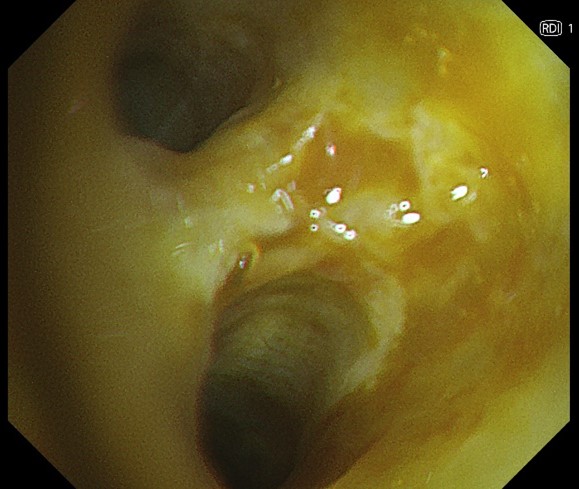
3. WLI vs. RDI observation
Foreign body seen inside LB3a with some slow bleeding. RDI confirmed no vessel encroachment at deeper level around the foreign body.
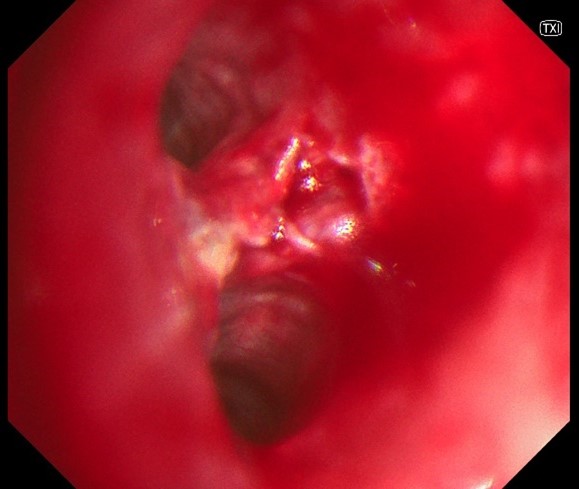
4. RDI vs. TXI observation
Multiple attempts were tried before the foreign body was successfully removed. RDI mode confirm that the only source of (mild) bleeding is from where the foreign body had previously impacted.
Case video
LB3c is shown at 1 o’clock position in the video clip. With BAI-MAC imaging on, the distal branching pattern within LB3c can be clearly seen from more than 2 bifurcations away (contrast this with the loss of detail when BAI-MAC were transiently turned off earlier in the clip). Pre-procedural planning had localized the pathology of interest with in LB3a & LB3c, but CT resolution was otherwise inadequate for more detailed planning; details picked up BAI-MAC imaging facilitating the decision to include LB3c pEBUS TBBX as part of the sampling procedure.
Overall Comment
BAI-MAC mode seems particularly suited to facilitate the observation of distant branching pattern in bronchoscopy, which is very useful in peripheral/navigational bronchoscopy procedure. Keeping the BAI-MAC mode turned on throughout the procedure does not otherwise seems to have an adverse effect on performance.
TXI mode gives a slightly better appreciation of subtle mucosal changes, but bronchoscopist might need to acclimatize to the new ‘red hue’ that can dominate the palette when there is significant surrounding inflammation or after local bleeding.
NBI is not a new imaging modality and continues to be useful in identifying neovascularization pattern; the vessels pickup looks even more obvious than previous generation.
RDI mode is very useful in confirming the absence, or the position of, deeper mucosal vessels to guide the site for safer endobronchial biopsy.
* Specifications, design and accessories are subject to change without any notice or obligation on the part of the manufacturer
- Keyword
- Content Type