Imaging Techniques Transduodenal bulb approach
IMAGING STEPS
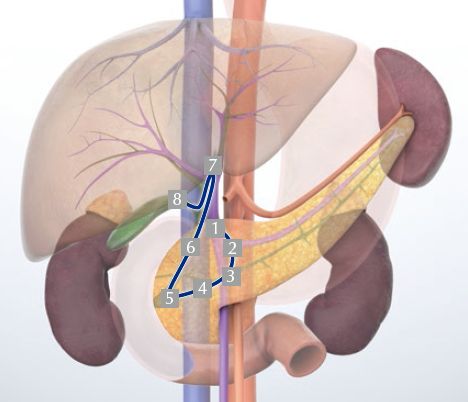
1 Portal vein
2 Portal confluence
3 Neck of the pancreas
4 Head of the pancreas/bile duct
5 Major papilla
6 Bile duct/right hepatic artery
7 Hepatic hilum
8 Gallbladder
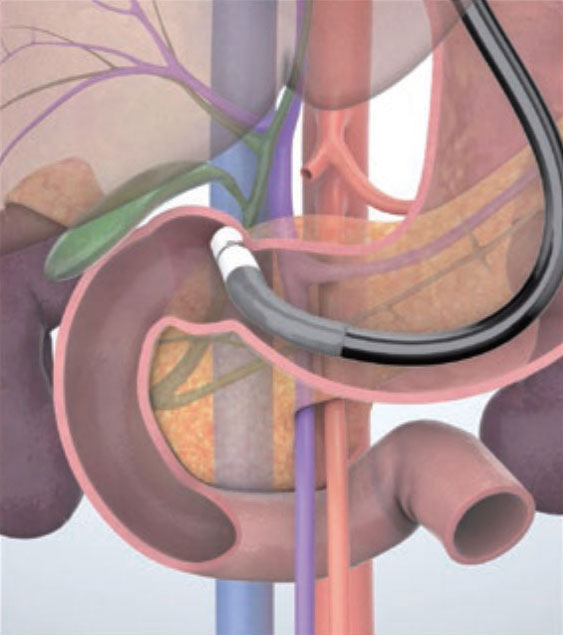
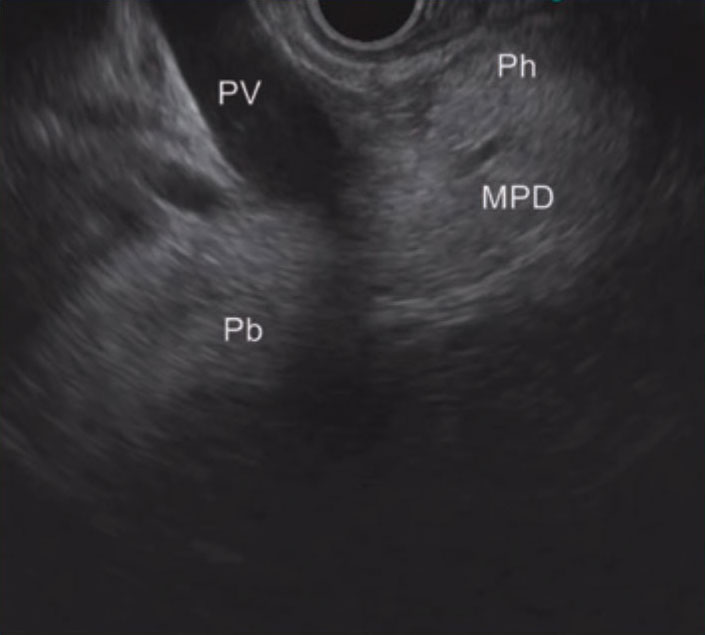
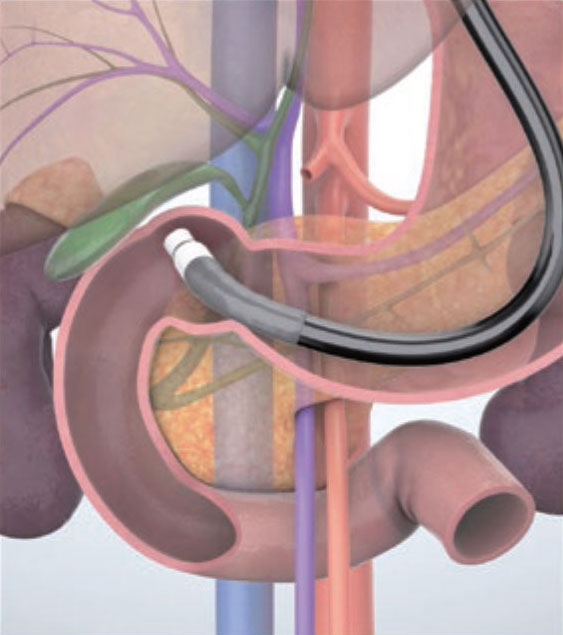
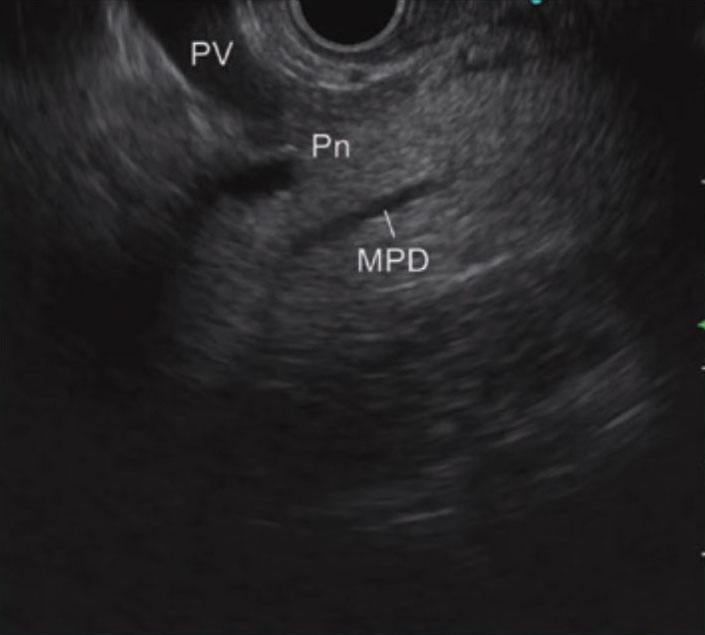
STEP 1 Portal vein
Insert the scope into the duodenal bulb to image the portal vein. If identification of the portal vein is difficult, first identify the intrahepatic portal vein and follow it towards the extrahepatic side.
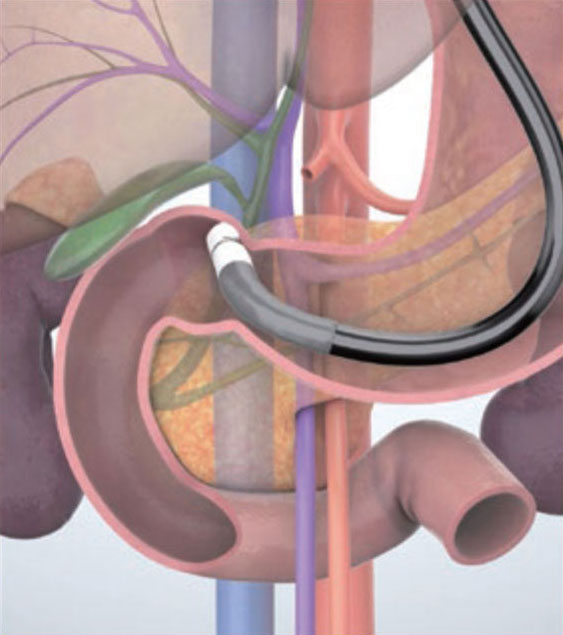
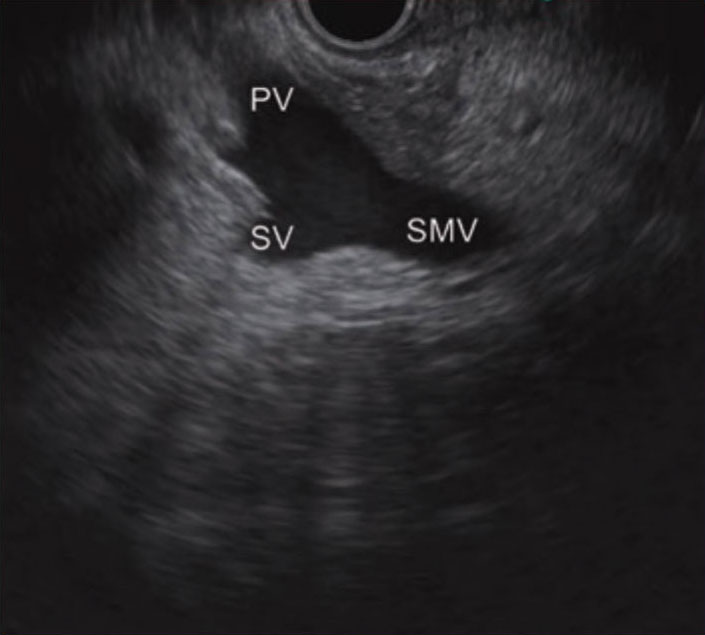
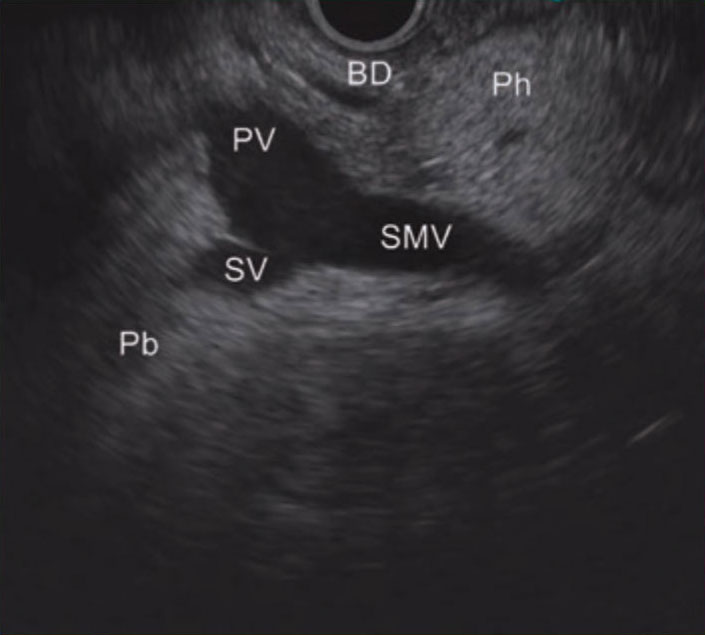
STEP 2 Portal confluence
Turn the scope clockwise while following the portal vein. The portal confluence will be imaged.
STEP 3 Neck of the pancreas
After having identified the main pancreatic duct, follow the main pancreatic duct from the confluence towards the body of the pancreas while turning the scope counterclockwise. The region where the main pancreatic duct crosses the superior mesenteric vein and portal vein is the neck of the pancreas. Observe this area carefully.
STEP 4 Head of the pancreas/bile duct
Visualize the bile duct that runs along the transducer side of the portal vein. While slowly advancing the scope, turn it clockwise to observe as far as the head of the pancreas.
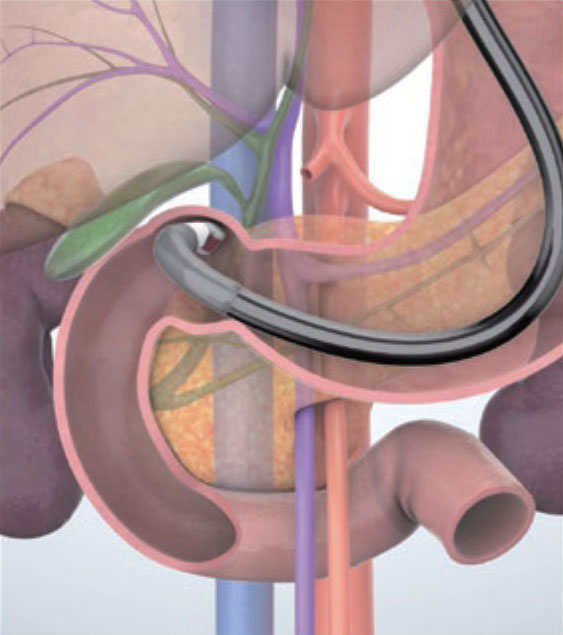
STEP 5 Major papilla
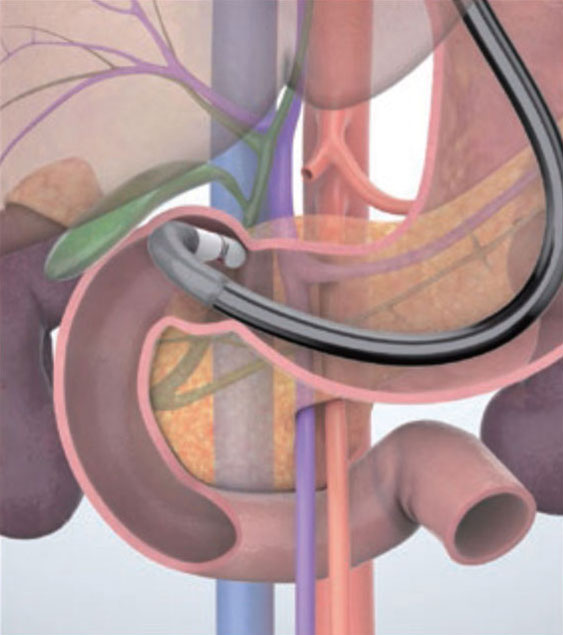
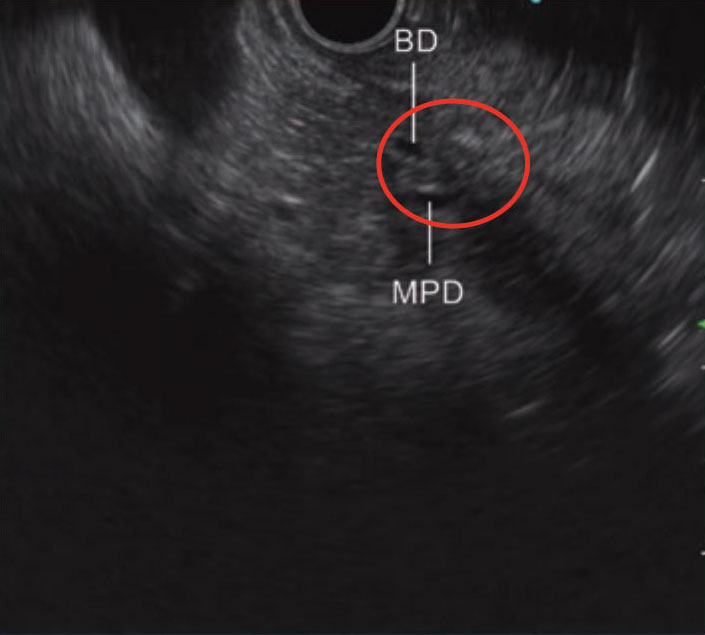
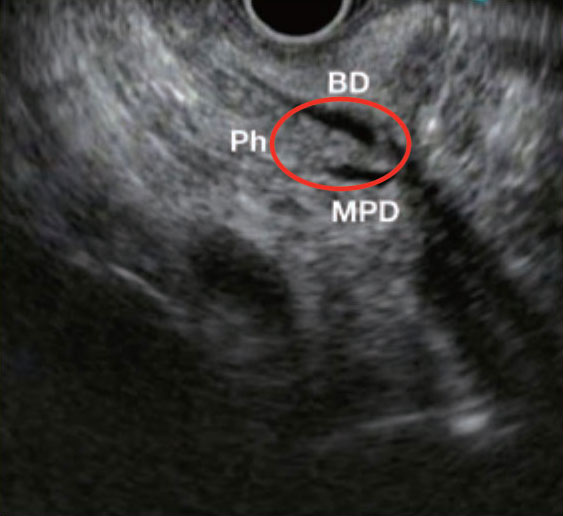
Keep turning the scope clockwise and advance the scope while bending the scope tip slightly upward. The head of the pancreas and the area of the major papilla (circled section) will be imaged on the right side of the screen. (see “Tip 6”).
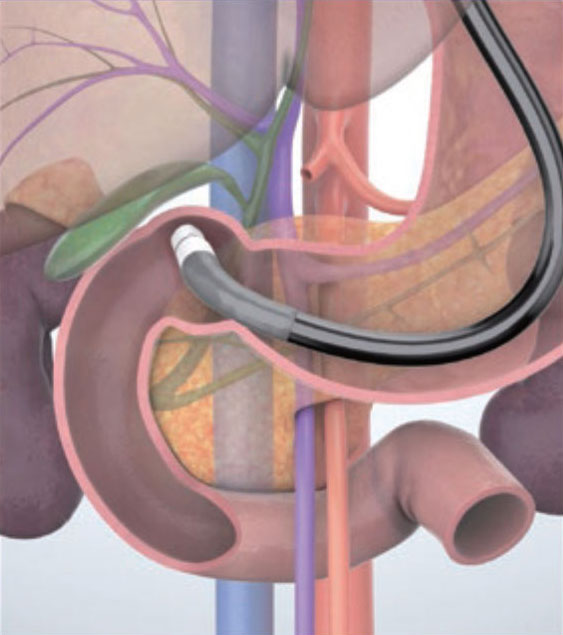
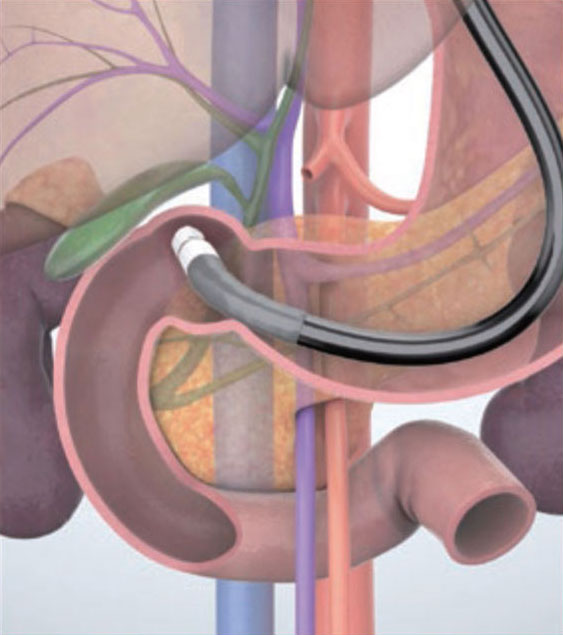
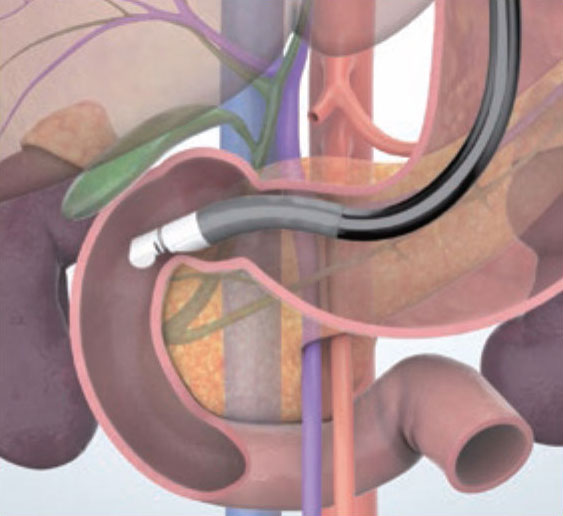
Since the scope tip may sometimes be forced against the duodenal wall in the operations in steps 4 and 5 (see the illustration), be careful not to perforate the wall by moving the scope around too much.
STEP 6-1 Bile duct
While withdrawing the scope with the scope turned counterclockwise and the scope tip angulated slightly downward, follow the bile duct that you identified in the area of the major papilla, to the direction of the hepatic hilum. Image the extrahepatic bile duct in the long axis direction (to the extent possible) and observe carefully.
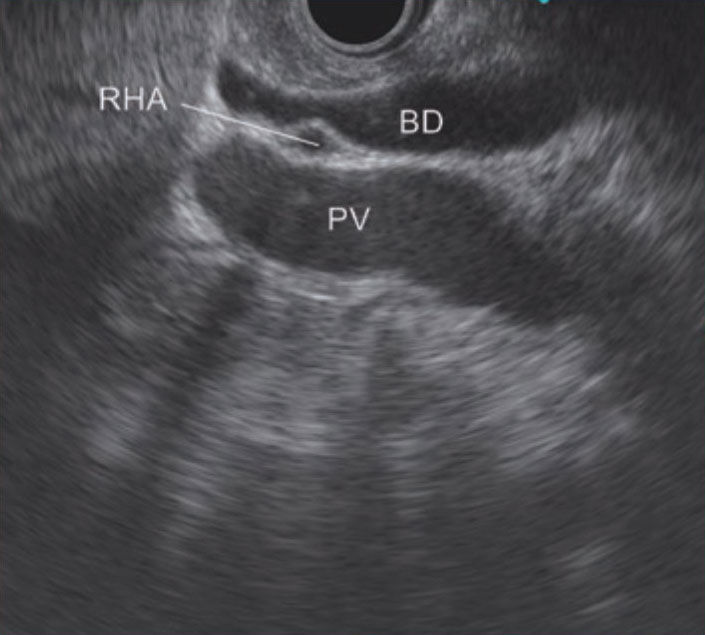
STEP 6-2 Right hepatic artery/proper hepatic artery
The right hepatic artery is imaged in sliced sections between the extrahepatic bile duct and the portal vein.
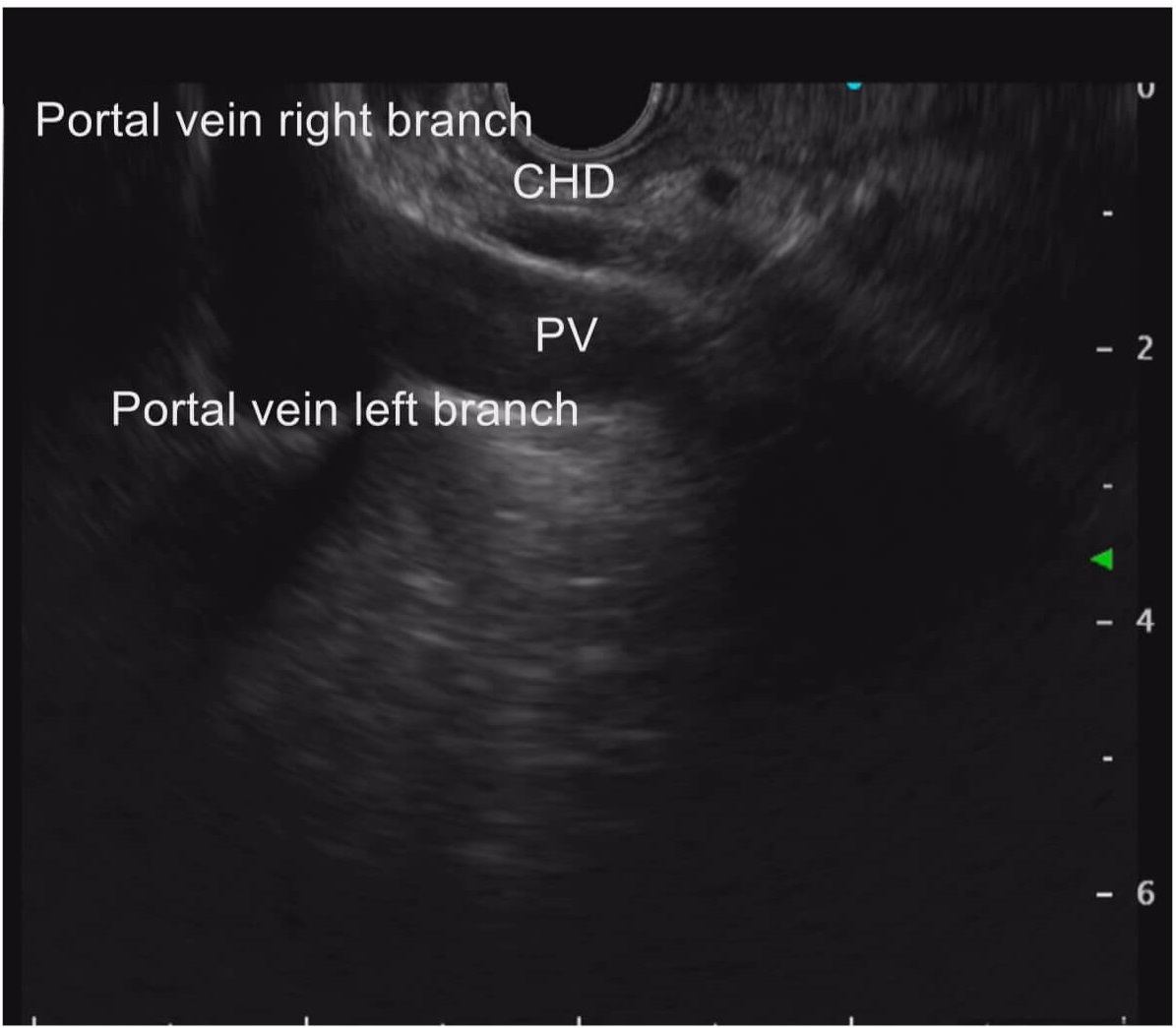
STEP 7 Hepatic hilum
Now proceed to observe the hepatic hilum while following the portal vein and bile duct in the direction of the liver by applying down angulation and counterclockwise rotation.
STEP 8 Gallbladder
At this point, you should be able to identify the junction where the bile duct and cystic duct join. From there, follow the cystic duct carefully and observe the gallbladder from the neck to the fundus. If visualization of the cystic duct is difficult, the gallbladder can usually be imaged if you turn the scope counterclockwise. (see “Tip 7”).
Imaging the inferior head of the pancreas from the duodenal bulb (See step 5 in “Transduodenal bulb approach”.)
The portal vein is the most obvious reference point in the transduodenal bulb approach — when the transducer is pushed into the duodenal bulb (with the scope tip slightly pointing to the superior side). The portal vein is the vessel that runs from the lower right of the ultrasound screen to the upper left (the liver is positioned in the upper left at this time). To observe the inferior neck of the pancreas in this condition, image the confluence of the portal vein, superior mesenteric vein, and splenic vein while slightly turning the scope clockwise (Fig. a).
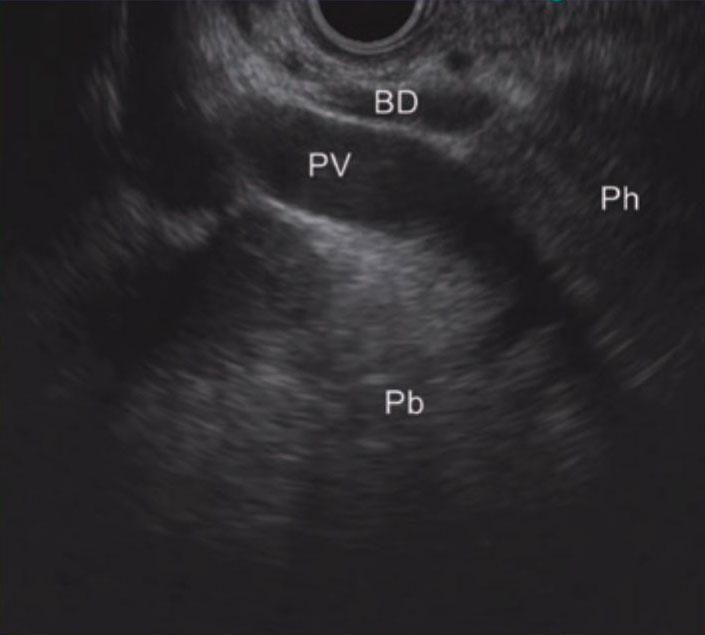
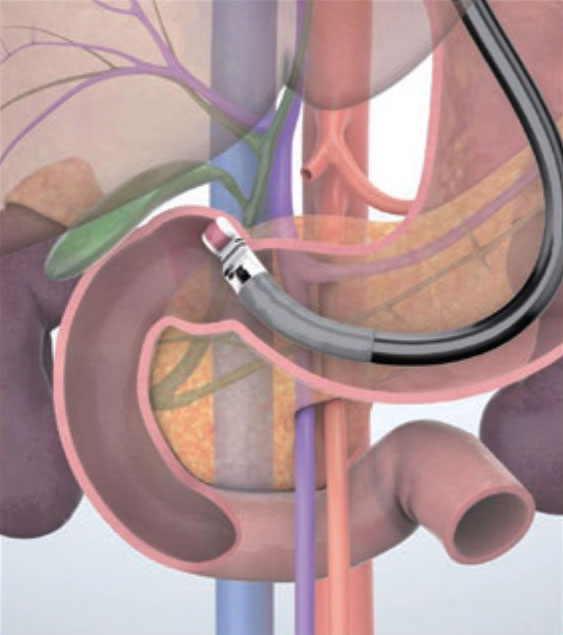
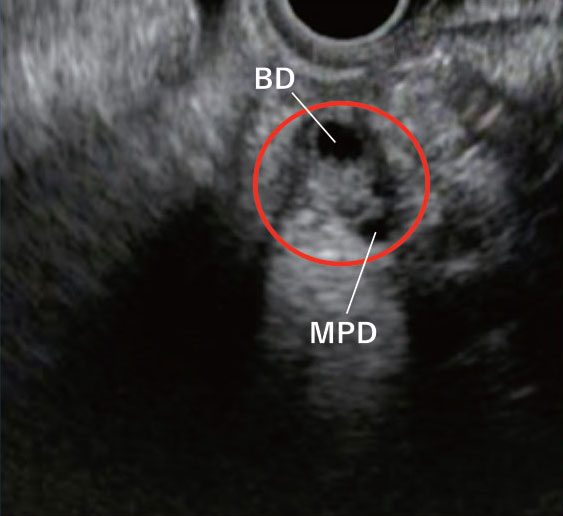
By slightly advancing the scope while turning it clockwise, you can visualize the head of the papilla and the area around the papilla (Fig. b, circled section) on the right side of the screen. In a clinical case where the scope tip is likely to drop into the descending part of the duodenum (Fig. c), the direction of the scope will change. As a result, the papilla (Fig. d, circled section) may be observed near the center of the visualized pancreas with the bile duct and main pancreatic duct shown in sectional slices. Hence, it is necessary to pay careful attention to their positional relationships.
Nevertheless, what is usually observed in this region is the area around the superior head of the pancreas. In other words, it is possible that the inferior head of the pancreas will not be properly imaged. Using force to advance the scope to observe the inferior head of the pancreas may cause duodenal perforation. Caution is required. At any rate, to properly observe the area around the inferior head of the pancreas, it is essential to obtain imaging from the descending part of the duodenum.
Imaging the gallbladder from the duodenal bulb (See step 8 in “Transduodenal bulb approach”.)
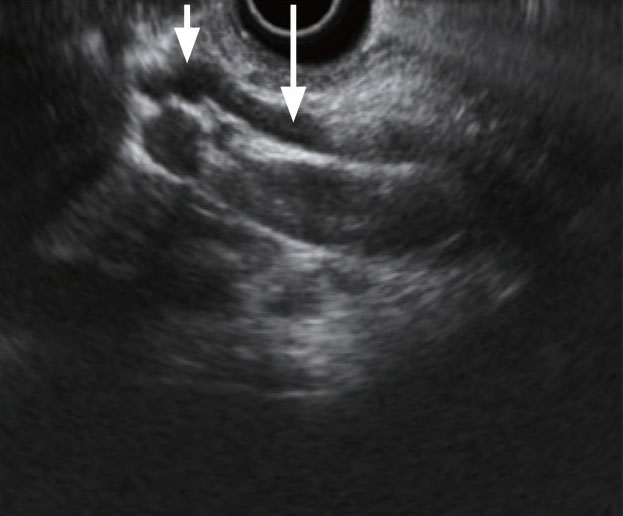
After having imaged the extrahepatic bile duct between the portal vein and transducer, you may recognize the cystic duct confluence (short ↓ in Fig. a) as you follow the extrahepatic bile duct (long ↓ in Fig. a) until the hepatic hilum. Once you have identified the cystic duct, you can image the gallbladder by following the cystic duct.
When you turn the scope clockwise or counterclockwise (we cannot say which is better because there are individual differences) while observing the cystic duct, you will be able to observe the entire area of the gallbladder from the neck to the fundus. However, the confluence morphology of the cystic duct and the position of the gallbladder differs from one individual to another. Keep in mind that proper visualization may not always be possible.
If imaging of the gallbladder is difficult using the above procedure, insert the scope into the duodenal bulb and point the transducer towards the anterior wall by turning the scope counterclockwise. This may visualize the gallbladder (Fig. b). Normally, the neck of the gallbladder will be imaged on the left side of the ultrasound screen, while the fundus will be imaged on the right side. However, this is not always the case, so observe the direction of the neck of the gallbladder while turning the scope clockwise or counterclockwise. If you can identify the neck, you will be able to observe from there to the cystic duct and extrahepatic bile duct as you continue to move the scope.
- Content Type