Standard Imaging Techniques
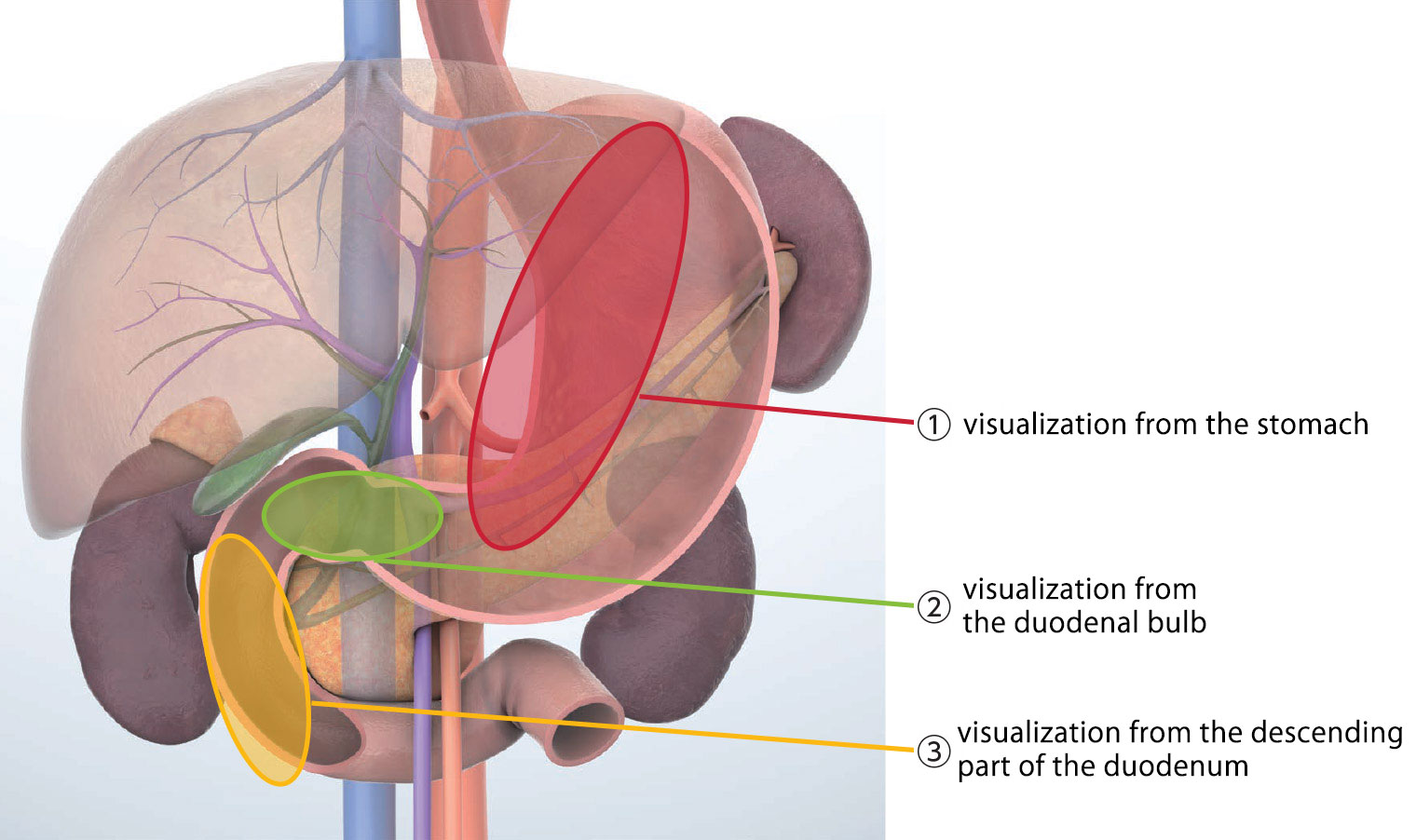
Scanning positions in radial EUS can be divided into: ① visualization from the stomach, ② visualization from the duodenal bulb (D1), and ③ visualization from the descending part of the duodenum (D2). When scanning from the duodenal bulb, observation is done in the “long-scope” position, in which the scope is pushed into the duodenal bulb. When scanning from the descending part of the duodenum, observation is made in the “short-scope” position, which is the same positioning used in ERCP procedures.
There is no specific rule regarding the order in which sites should be observed. The main point is to remember that observation of each site should not be performed from a single location. Rather, the site should be observed from multiple locations so that the site can be visualized from every possible point of view. Each scanning position has its own observable regions. Landmarks have been specified to support visualization of those regions from each scanning position. Again, although these landmarks do not need to be visualized in any particular order, they should be visualized one step at a time. To ensure optimal observation, visualization should be carefully performed by following the steps set out for the observable regions of each scanning position (Table a).
Basic maneuvers of the endoscope are clockwise/counterclockwise rotation, up/down angulation, and left/right angulation, as well as pushing and pulling. Combining these various maneuvers as necessary enables you to comprehensively observe the region of interest. When you rely on ultrasound imaging rather than endoscopic imaging, you may find yourself operating blindly when maneuvering the scope. Consequently, you need to be especially cautious in order to avoid making any perforations – particularly when inserting the scope in the pharynx or duodenal bulb, as well as when maneuvering the endoscope into a “short-scope” position in the duodenum.
To obtain clear images with good quality and fewer artifacts, it is necessary to sufficiently suction the gastrointestinal tract. It is also necessary to inflate the balloon as needed to keep the scope tip in close contact with the wall of the gastrointestinal tract. Lukewarm water should also be instilled ‘as needed’ to expand the lumen of the gastrointestinal tract.
Observable regions and landmarks (Table a)
| Scanning position | Observable region | Landmark |
|---|---|---|
| Stomach | Pancreatic body Pancreatic tail |
Splenic artery/vein Left kidney Spleen Superior mesenteric artery Celiac artery Aorta Left adrenal gland |
| Duodenal bulb | Pancreatic head Pancreatic head/body junction Main pancreatic duct Bile duct Cystic duct Gallbladder |
Portal vein Superior mesenteric vein Splenic vein |
| Descending part of the duodenum | Pancreatic head Duodenal papilla Main/accessory pancreatic ducts Bile duct Gallbladder |
Aorta Inferior vena cava Superior mesenteric artery/vein Portal vein |
 ①
①Scroll/display range
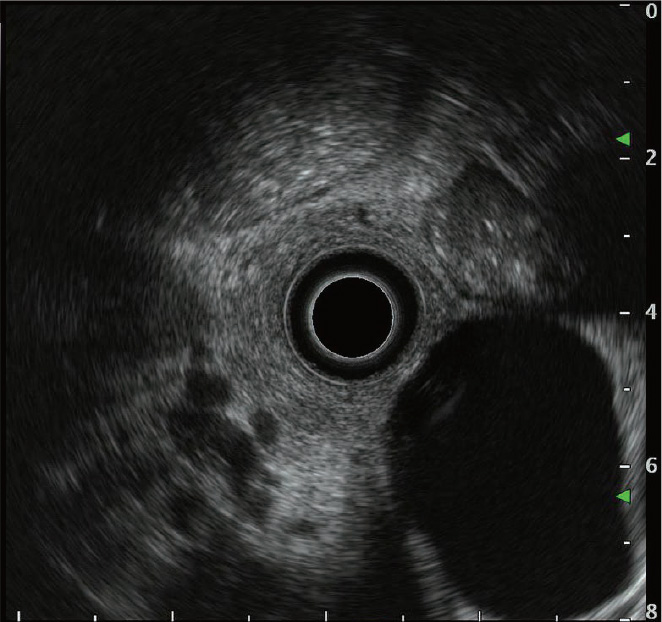
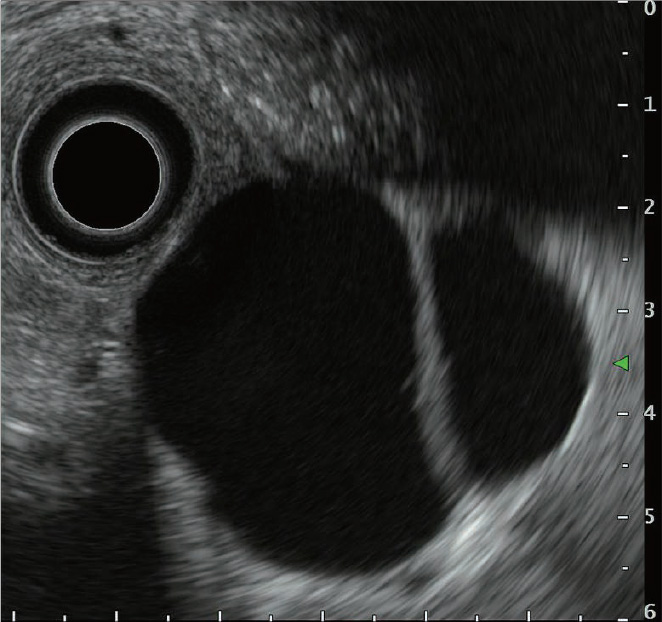
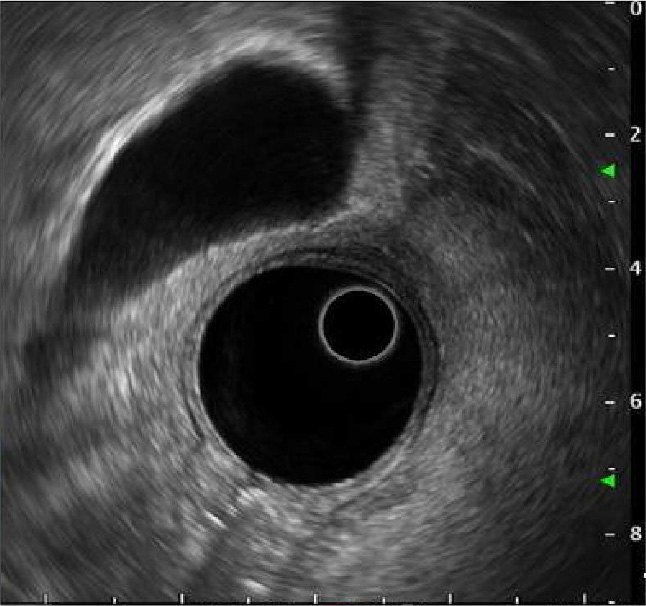
Even though radial EUS offers 360-degree ultrasound images, targeted objects are often located on the periphery of the view field, potentially making observation more difficult (Fig. a). In this case, simply move the object to the center of the view field using the scroll function to make it easier to observe (Fig. b).
Lesions related to pancreatobiliary diseases are often quite small, which may result in them being displayed too small in the default display range. The ultrasound image display range can be changed to accommodate this – an especially useful feature when the targeted object is too small (Fig. c).
 ②
②How to inflate the balloon
To obtain good-quality images with fewer artifacts in radial EUS, the scope tip (transducer) must make close contact with the gastrointestinal wall. The use of a balloon is critical to facilitating this procedure.
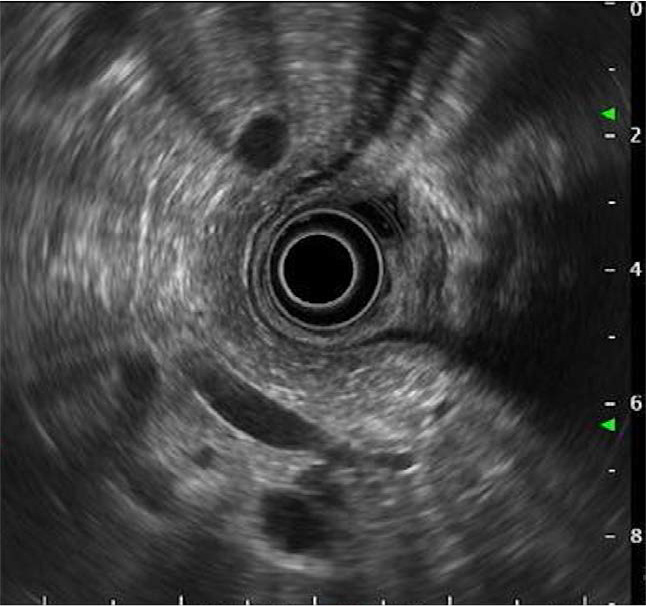
Mount the balloon appropriately on the scope tip and confirm that water stays inside the balloon without leaking. Moreover, as bubbles inside the balloon can produce unwanted artifacts, make sure that you eliminate them by repeatedly inflating and suctioning the balloon while keeping the scope tip downward (Fig. a).
Press the air/water valve of the scope to inflate the balloon. While confirming the size of the balloon on the ultrasound screen, continue to press the air/water valve to inflate the balloon. The size of the balloon is optimal when the scope tip is directly contacting the gastrointestinal wall and artifacts disappear.
In fact, in most procedures all you need do is fill enough water to slightly inflate the balloon (Fig. b). In the case of the duodenal bulb, however, the balloon needs to be inflated to the point where it fills most of the lumen because artifacts are likely to occur (Fig. c). Also when you are maneuvering the endoscope in a “short-scope” position, it may be a good idea to inflate the balloon to the point where it is large enough to keep the scope stable and prevent the scope from with losing position. Nevertheless, caution is required not to overly inflate the balloon because doing so may immobilize the scope tip and make it difficult to change the direction of the scope.
- Content Type