Colorectal Case 32

Dr. Hiroaki Ikematsu
Department of Gastroenterology and Endoscopy, National Cancer Center Hospital East, Japan
The CF-XZ1200 will contribute to lesion detection with clear images of color tones and unevenness of the mucosal surface in middle to long distance view
In endoscopic diagnosis of colorectal lesions, endoscopists have pursued the accuracy of lesion detection in screening under WLI or NBI in middle to long distance view. They have also pursued the accuracy of qualitative/invasion-depth diagnosis in magnifying endoscopy under NBI or magnifying chromoendoscopy under WLI. The CF-XZ1200 (XZ1200), a new magnifying endoscope,exhibits improved various points of observation performance, as compared to conventional models. I find that the XZ1200 imaging is useful to advance the accuracy for both of screenings and detailed examinations.
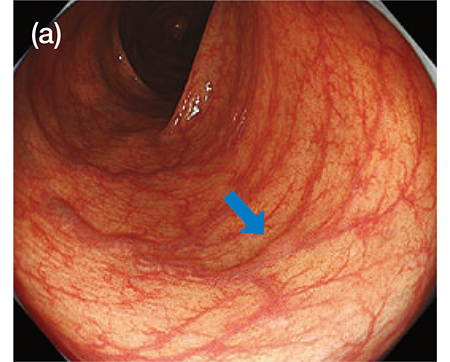
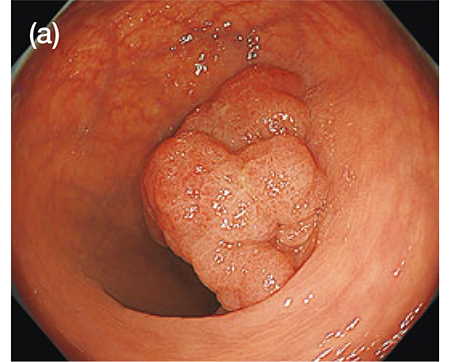
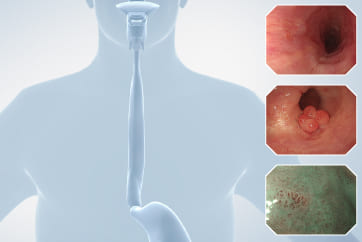
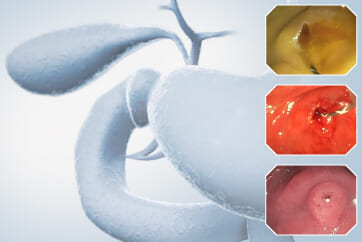
During screening tests, the key point of lesion detection is certain capturing of changes in color tones and unevenness of the mucosal surface under WLI or NBI in middle to long distance view during scope withdrawal. In corporation of a highly sensitive CMOS image sensor chip into the XZ1200 achieved noise reduction and high resolution image. I find that these improvements in image quality enables clear imaging in middle to long distance view, as compared to conventional models. Therefore, it appears that slight changes in unevenness and color tones (such as pale redness) of the lesion are captured more clearly under WLI (Fig. 1a). The improvements in image quality also could be realized in observations under NBI. In my first experience utilizing NBI with the XZ1200, I was deeply impressed by the differences in image clarity from previous models. I find that observations under NBI by using the XZ1200 will increase the lesion detection rate because of improved visibility of brownish areas even for flat or depressed lesions with only little unevenness. Because the lesion detection is the most important outcome of screening, I think that the observation performance advanced by these improvements is one of the greatest benefits of the XZ1200.
The adoption of a high-speed sequential-frame method to the XZ1200 increased the frame rate (120 fps). This improvement reduced the color misregistration caused from shifts of the endoscopic field of view, as compared to conventional sequential frame method. In practice, with the conventional model, I sometimes noticed color misregistration during water washing or quick scope manipulations. However, when using the XZ1200, I have found that color misregistration is no longer noticeable, even in similar situations. Alternatively, retakes of endoscopic images were occasionally required for the acquisition of still images in conventional models because the color misregistration made the images obscure, particularly in scenes with movement of the mucosa. However, it seems that high certainty for acquisition of clear images with the XZ1200 reduced the number of retakes.
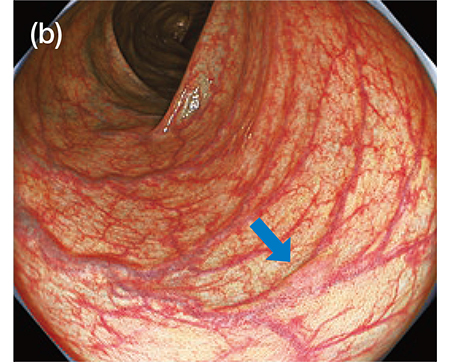
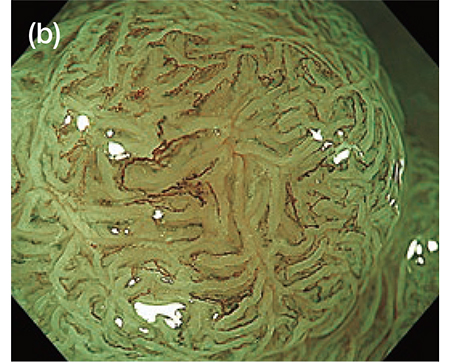
[Fig. 1]Images of the same lesion in middle distance view obtained by the XZ1200 under WLI (a) and TXI (Mode 1) (b)
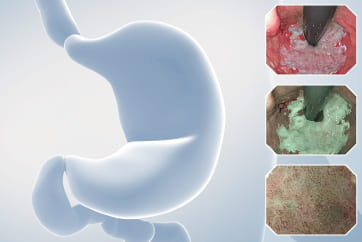
The combination of the XZ1200 with TXI observation/BAI-MAC function equipped with the EVIS X1 may lead to further improvements in the lesion detection rate
TXI is a texture and color enhancement function developed for the EVIS X1 by using original image processing technology of Olympus. TXI will improve the visibility of lesions as compared to WLI becauseTXI enhances slight changes in color tones and texture. Besides, the color tone of endoscopic image under TXI is similar to that under WLI. Therefore, additional use of TXI in difficult situations for evaluation will improve the lesion detection rate for endoscopists who primarily conduct screening under WLI during scope withdrawal. At our hospital, colorectal screening tests are primarily conducted under NBI because we find that observations under NBI during scope withdrawal are useful for detecting lesions. In adequate bowel preparation leads to low visibility because the residue appearsred under NBI. In these difficult situations, we used to rinse off the residue with water washing. However, this method can be substituted by simply switching to TXI. Thus, use of TXI instead of WLI will improve visibility and the lesion detection rate (Fig. 1b).
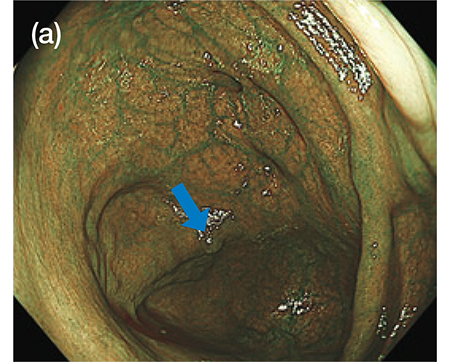
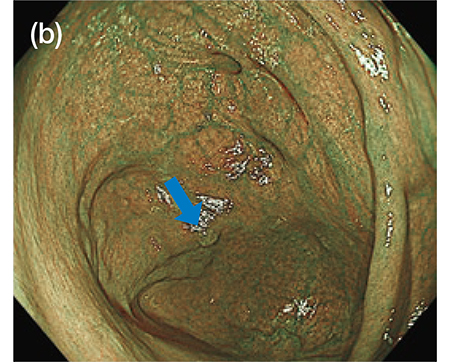
Furthermore, the EVIS X1 is equipped with BAI-MAC function that can increase the brightness of far points while maintaining the brightness of near points during observation in middle to long distance view under NBI or WLI. I find that the use of BAI-MAC function in combination with the XZ1200 allows for brighter and clearer visualization of far points which tend to be dark under NBI, compared to the combination of conventional scope and endoscope system (Fig. 2a, b).
[Fig. 2]Images of the same lesion in long distance view obtained by the XZ1200 under NBI
(a) BAI-MAC off; (b) BAI-MAC on
High quality and high magnification imaging in magnifying endoscopy during detailed examination will advance the accuracy of qualitative/invasion-depth diagnosis
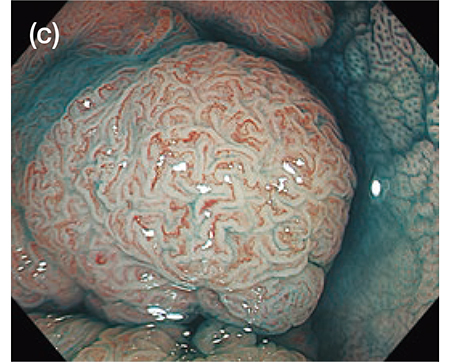
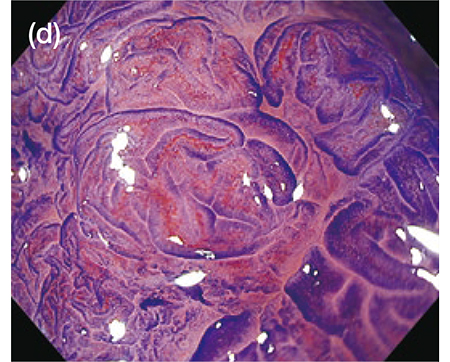
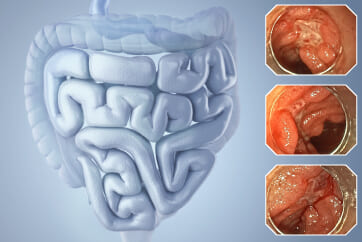
At our hospital, CF-HQ290Z or PCF-H290Z magnifying endoscopes in combination with a 26-inch monitor OEV262H have been used for all endoscopic examinations, including screening tests as well as detailed examinations for lesions detected at screening. However, there were several situations where I wished I could evaluate lesions with magnifying observation at a slightly higher magnification. This newly developed endoscope, the XZ1200 achieved higher qualityof images even with the same diameter as that of CF-HQ290Z (tip;13.2 mm, insertion; 12.8 mm). In addition, the combination with the EVIS X1 and OEV321UH monitor (32-inch, 4K-compatible) enables clear magnifying endoscopic view at the maximum magnification of 135x. I find that these improvements in the XZ1200 will advance the quality of diagnosis of invasion depth for colorectal cancer in magnifying endoscopy under NBI and magnifying chromoendoscopy. It is because that the XZ1200 provides more detailed observation and evaluation for the lesions in difficult cases, especially in situations with low confidence (Fig. 3).
In magnifying observation under NBI with the XZ1200, I have an impression that both the vessel pattern and the surface pattern of the lesions are clearly visualized as compared to conventional models (Fig. 3b). This may lead to advances in the accuracy and the confidence of magnifying NBI diagnosis based on the JNET classification. Specifically, regarding the diagnosis of invasion depth of T1a/T1b cancer by the differentiation of Type 2B/Type 3, its accuracy has been questioned. However, the XZ1200 will advance the confidence of this diagnosis. Besides, the vessel pattern in Type 1 is defined as “invisible”. Furthermore, vessel pattern-based differentiation is difficult between hyperplastic polyps and SSL (both are classified in Type 1). It is possible that the improved visibility of vessel pattern provided by the XZ1200 leads to the future discovery of vessel findings which can be used for the differential index of these histological types. In other words, the current diagnostic system for magnifying endoscopy was established from the vascular findings which can be captured by magnifying endoscopes with conventional observation performance. It is possible that the diagnostic system will need to be updated in the future because previously invisible vessel patterns will become visible with the XZ1200.
Additionally, regarding the differentiation of non-tumor/tumor by the differentiation of Type 1/Type 2A, the sufficient accuracy with conventional magnifying observation under NBI has already been confirmed. However, some adenomas still can be classified as Type1 because the vessel pattern cannot be recognized with conventional magnifying observation under NBI. Here again, the improved visibility of the vessel pattern in the endoscopy with the XZ1200 may advance the accuracy and the confidence of this differentiation.
Alternatively, in magnifying chromoendoscopy for the pit pattern diagnosis, I have an impression that the XZ1200 enables more detailed evaluation of the pit pattern by the improved visibility of each pit in the lesion compared to the conventional models regardless of image types of chromoendoscopy (indigo carmine spraying or crystalviolet staining) (Fig. 3c, d). Therefore, I expect that the XZ1200 advances the accuracy and the confidence of pit pattern diagnosis, including the evaluation of type V pit pattern for the diagnosis of invasion depth of submucosal colorectal cancer. Additionally, the EVIS X1 is also equipped with RDI, an image-enhanced observation technology which improves the visibility of superficial to deep blood vessels. I find that the pit pattern is more clearly visualized by magnifying chromoendoscopy in combination with the EVIS X1 by using TXI or RDI instead of conventional WLI. Switching from WLI to TXI after indigo carmine spraying appears to emphasize the pit edges. On the other hand, switching to RDI after crystal violet staining changes the color tone in whole endoscopic view and appears to clearly visualize the gland ducts with high contrast. The combined use of the EVIS X1 and the XZ1200 may make it possible to obtain such clear images, and to evaluate the pit pattern more easily.
[Fig. 3] The XZ1200 observation images of a Is+IIa (LST-G) lesion
(adenocarcinoma, tub1, in tubular adenoma, pTis, Ly0, V0, the size; 30 mm)
(a) Middle distance view under WLI;
(b) Magnified view under NBI (JNET classification: Type 2A);
(c) Magnified view after indigo carmine spraying;
(d) Magnified view after crystal violet staining (pit pattern: IV)
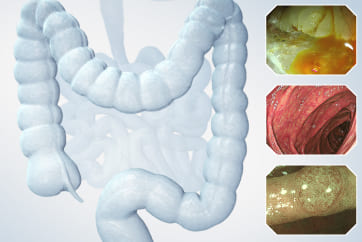
Improvements in the image quality and the brightness of NBI observation by the XZ1200 contribute to the advanced quality of diagnosis from screening to detailed examination
Al though there are var ious improvements in observation performance with the XZ1200, In my experience, the biggest advantage is the quality and the brightness of images under NBI, particularly in combination with the EVIS X1 and OEV321UH. In screening tests in middle to long distance view under NBI, I find that BAI-MAC function of the EVIS X1 enables brighter and clearer images regardless of observation distances compared to conventional models, leading to an improvement in the lesion detection rate. In detailed examinations, more precise evaluations of the vessel pattern and the surface pattern of the lesions are difficult with conventional models. However, I find that these evaluations become easier in magnifying observation under NBI with the same combination. These improvements may advance the quality of magnifying diagnosis, including histological type differentiation and diagnosis of invasion depth.
Regardless of their previous experiences, all users will realize the benefits of the improved image quality with the XZ1200 in various aspects of colonoscopy. I hope fewer overlooked lesions and higher diagnostic accuracy will be achieved in colonoscopy, leading to the advancements in the quality of endoscopic diagnosis and treatment for colorectal cancer.
* Specifications, design and accessories are subject to change without any notice or obligation on the part of the manufacturer
- Content Type